Postoperative nausea and vomiting are a frequent complication and are of particular interest to the surgical team. Its prevalence is 50% and 30% respectively, increasing to 80% in high-risk patients. It has special importance for anaesthetic management, since the presence of these symptoms prolongs the length of hospital stay, and delays discharge in outpatient surgery, with a consequent increase in the cost of care. 5-hydroxytryptamine type-3 antagonists (ondansetron) are the gold standard treatment; however there are many additional therapeutic options, including propofol, which is a widely distributed and easily accessible drug.
ObjectiveTo demonstrate that ondansetron and propofol are an equipotent prophylactic therapy for the control of postoperative nausea and vomiting in nasal surgery.
MethodologyAfter obtaining informed consent and receiving approval from the institutional research ethics committees, a randomised, prospective, longitudinal, blind, comparative, clinical trial was conducted in which 46 patients were studied, divided into two groups. One group received 4mg intravenous ondansetron and the second group received 20mg intravenous propofol; both drugs were administered at the end of the surgery. The presence of nausea and vomiting was evaluated in the immediate post-anaesthetic period and 2, 4 and 6h afterwards.
ConclusionsThere were no statistically significant differences in the presence of postoperative nausea and vomiting between the two groups.
Las náuseas y el vómito postoperatorio son una complicación frecuente y de especial interés para el equipo quirúrgico; su prevalencia es del 50% y 30% respectivamente, presentando un incremento hasta el 80% en pacientes de alto riesgo. Cobra especial importancia para el manejo anestésico, puesto que la presencia de estos síntomas prolonga el tiempo de estancia hospitalaria, y retrasa el egreso en cirugía ambulatoria, con el consiguiente aumento en los costos de la atención. Los antagonistas de los receptores tipo 3 de la 5–hidroxitriptamina (ondansetrón) son el gold estándar de tratamiento; sin embargo, hay múltiples opciones terapéuticas adicionales, entre las que se encuentra el propofol, que es un medicamento de amplia distribución y fácil acceso.
ObjetivoDemostrar que existe equipotencia terapéutica profiláctica para el control de las náuseas y el vómito posoperatorio entre el ondansetrón y el propofol en cirugía nasal.
MetodologíaPrevio consentimiento informado y aprobación de los comités institucionales de investigación y ética, se realizó un ensayo clínico comparativo, prospectivo, longitudinal, ciego y aleatorio en el cual se estudiaron 46 pacientes divididos en dos grupos. Un grupo recibió ondansetrón 4mg endovenoso y el segundo grupo recibió propofol 20mg endovenoso; los fármacos se administraron al término del evento quirúrgico. Se evaluó la presencia de náuseas y vómito en el periodo postanestésico inmediato, a las 2, 4 y 6 horas posteriores.
ConclusionesLa presencia de náuseas y vomito postoperatorios no tuvo diferencia estadísticamente significativa entre los dos grupos.
Every year, 75 million patients are anaesthetised worldwide, of which an estimated one-third present postoperative nausea and vomiting (PONV).1 Despite advances in surgical and anaesthetic techniques, such as the development of antiemetic drugs combined with non-pharmacological measures to control this problem, the prevalence of PONV in the general population remains constant around 20–50%, increasing to 80% in high-risk patients.2
From the patient's perspective, having PONV is one of the problems causing the most fear, especially if the patient has previously had surgery and suffered it in the postoperative period. One prospective study conducted in 10,811 patients undergoing different types of surgery found that PONV is the third-most common fear for patients, after postoperative pain and the possibility of waking during the surgery.3
The aetiology of PONV is multifactorial and involves factors related to the patient, the surgery and the anaesthesia. The patient-related factors are outside the anaesthetist's control, but they should be identified and assessed during the pre-anaesthetic assessment. These include, age, sex, history of vertigo, PONV, and history of tobacco use; some patients have co-existing medical conditions such as gastrointestinal (hiatal hernia, gastro-oesophageal reflux) or metabolic (diabetes mellitus, uraemia, water–electrolyte imbalances) diseases, pregnancy or preoperative anxiety, which can predispose them to presenting PONV. Patients with increased intracranial pressure as in the case of brain tumours, undergoing chemotherapy/radiotherapy or with intestinal overstimulation such as acute abdomen have a higher risk of PONV. The surgery-related factors are also unable to be altered, but they should be taken into account for prevention and treatment, since certain types of surgery such as ear, nose and throat surgery, dental surgery, breast augmentation, laparoscopic surgery and strabismus surgery have been associated with a higher incidence of PONV than other procedures.
Another surgery-related factor affecting incidence is the surgery duration, since this increases the exposure to potentially emetogenic anaesthetic drugs. Anaesthesia-related factors can be controlled; these factors include: pre-medication, anaesthesia technique, anaesthetic drugs, hydration and postoperative pain management.4
Apfel created a modified score to establish the risk of postoperative nausea and vomiting which includes five items worth one point each. These include: female gender, history of postoperative nausea and vomiting, under 50 years of age, non-smoker, opioid use, or presence of nausea in the post-anaesthetic care unit; a score of 0, 1, 2, 3, 4 or 5 of these conditions corresponds to an approximate risk of postoperative nausea and vomiting of 10%, 20%, 30%, 50%, 60% and 80%, respectively.5
Pathophysiology of nausea and vomitingA large number of molecular signalling pathways and receptors are involved in the origin of PONV, including dopamine type-2 (D2), serotonin type-3 (5-HT3), histamine type-1 (H1) and muscarinic cholinergic type-1 (M1). Most antiemetic drugs act by antagonising one or more of these receptors.
The chemoreceptor trigger zone is rich in D2 and 5-HT3 receptors. The vomiting centre is located on the reticular formation of the medulla oblongata and is stimulated by three types of inputs:
- (1)
Vestibular: These come from motion sickness. The main neurotransmitter for the vestibular nerve fibres is glutamate, however most of the receptors are for histamine H1 and H2.
- (2)
Visceral: These are vagal parasympathetic and splanchnic sympathetic inputs, transmitted through the solitary tract (structure containing a number of histamine and acetylcholine receptors), which proceed to structures in the gastrointestinal tract and are activated by inflammation and mechanical distension, among others.
- (3)
Chemoreceptor trigger zone (CTZ): This area is found in the area postrema near the floor of the fourth ventricle. It has a high number of serotonin and dopamine receptors. Its location outside the blood–brain barrier enables it to constantly control the blood and cerebrospinal fluid flow, identifying the presence of toxic substances such as alcohol or different drugs (dopaminergic drugs, opioids, digitalis drugs, theophylline, salicylates and anti-cancer drugs), and to transmit that information to the vomiting centre.
Ondansetron was the first serotonin (5-HT3 receptors) antagonist described with high antiemetic power and fewer side effects compared with previous antiemetics.6 It is considered the gold standard, at doses 4mg and 8mg in cancer patients.5 The importance of serotonin-receptor antagonists lies in the pathophysiological aspects, since ingesting toxic substances results in the release of serotonin by enterochromaffin cells and indirectly by other receptors such as M3-B adrenoceptors and H3 receptors. Serotonin is secreted and travels through the spinal cord via the solitary tract triggering nausea and vomiting, therefore serotonin antagonists are one of the many measures for preventing the development of nausea and vomiting.6
Trammer et al. suggest that using 4-mg or 8-mg doses regardless of the type of patient prevents postoperative nausea and vomiting, especially during the first 24h. Ondansetron was administered at the end of the surgery since Tangs’ study demonstrated that administering it immediately after finishing the surgery was more effective for preventing PONV.7
Propofol is currently the most commonly used intravenous anaesthetic. It belongs to the alkylphenol family and is used as a hypnotic, sedative, anticonvulsant, and recently an antiemetic drug. It has a fast onset of action but a short duration, thanks to its rapid plasma clearance.8
It mainly acts on the GABA receptor by increasing the chloride ion conduction. It has an inhibitive effect on smooth muscle calcium channels, is an agonist of dopaminergic receptors, and is a serotonin-receptor antagonist, the mechanism of action that explains its antiemetic effect. Its pharmacokinetic profile is based on a three-compartment system with an alpha half-life of 2–4min, a beta half-life of 30–60min and a gamma half-life of 6–10h. It has a clearance rate of 30ml/kg/min.9
Propofol is commonly used in total intravenous anaesthesia. Its use to induce and maintain anaesthesia enables the risk and incidence of PONV to be decreased in the first 6h, with a number needed to treat (NNT=5).10,11
The combination of propofol and air/oxygen reduces the risk of PONV by approximately 25%.15 A systematic review of 58 studies demonstrated that the use of propofol vs inhalational anaesthesia reduced the incidence of nausea and vomiting after medical discharge.12
In small doses (20mg), propofol can be used as a salvage therapy in patients with nausea and vomiting in the post-anaesthetic recovery room who are resistant to conventional pharmacological therapy and is as effective as ondansetron.13,14
Numerous studies have demonstrated its antiemetic properties. The plasma concentrations associated with the antiemetic effect correspond to 343ng/ml, decreasing cases of nausea and vomiting up to 50%; its use to induce and maintain general anaesthesia has therefore been associated with a lower incidence of PONV.6,19
A study was conducted in Korea with 107 women who underwent a vaginal laparoscopic hysterectomy under general anaesthesia with patient-controlled postoperative analgesia. They were divided into three groups; all groups received the medication 15min before the end of surgery. Group A received fentanyl 50mcg+propofol 0.5mg/kg, Group B fentanyl 50mcg+propofol 1mg/kg, and Group C fentanyl 50mcg and saline solution. The incidence of postoperative nausea and vomiting was significantly lower in the propofol groups (12.1% vs 14.7% and 40%).15
The incidence of nausea and vomiting can decrease with subhypnotic doses of propofol. Numasake showed that low doses of propofol reduce nausea and vomiting in patients with a neuraxial blockade. In their study, Razzoli et al. confirmed that patients who received a 20mg dose of propofol presented a significant reduction in the incidence of nausea and vomiting, without causing more sedation or respiratory depression.16
MethodologyA clinical trial was conducted (randomised, prospective, longitudinal, blind, comparative). The sample size was determined based on the difference between two independent means.
Input parameters:
- •
Effect size=0.8
- •
P-value (alpha)=0.05
- •
Power=0.800
Output parameters:
- •
Delta non-centrality parameter=2.5922963
- •
Critical t=1.6838510
- •
Df=40
- •
Size group 1=21
- •
Size group 2=21
- •
Total size=42
- •
Actual power=0.8167878
Since there is little published data about improvement in the clinical course of nausea and vomiting in patients who received ondansetron and/or propofol, we took the article by Unlugenc et al. “Comparative study of the antiemetic efficacy of ondansetron, propofol and midazolam in the early postoperative period”; in which a difference in means (DM) of −0.49 was reported as a basis for calculating the number of subjects needed per group using the sample size formula, where the objective is to compare two samples with a two-tailed α of 0.05 and a power (1−β) of 0.84.
N=42 patients per group
Considering a 10% loss of subjects in the study, the sample was increased to a total of 46 patients (23 per group).
The study objective was to demonstrate equivalent prophylactic therapeutic potency for the control of postoperative nausea and vomiting between ondansetron and propofol in nasal surgery.
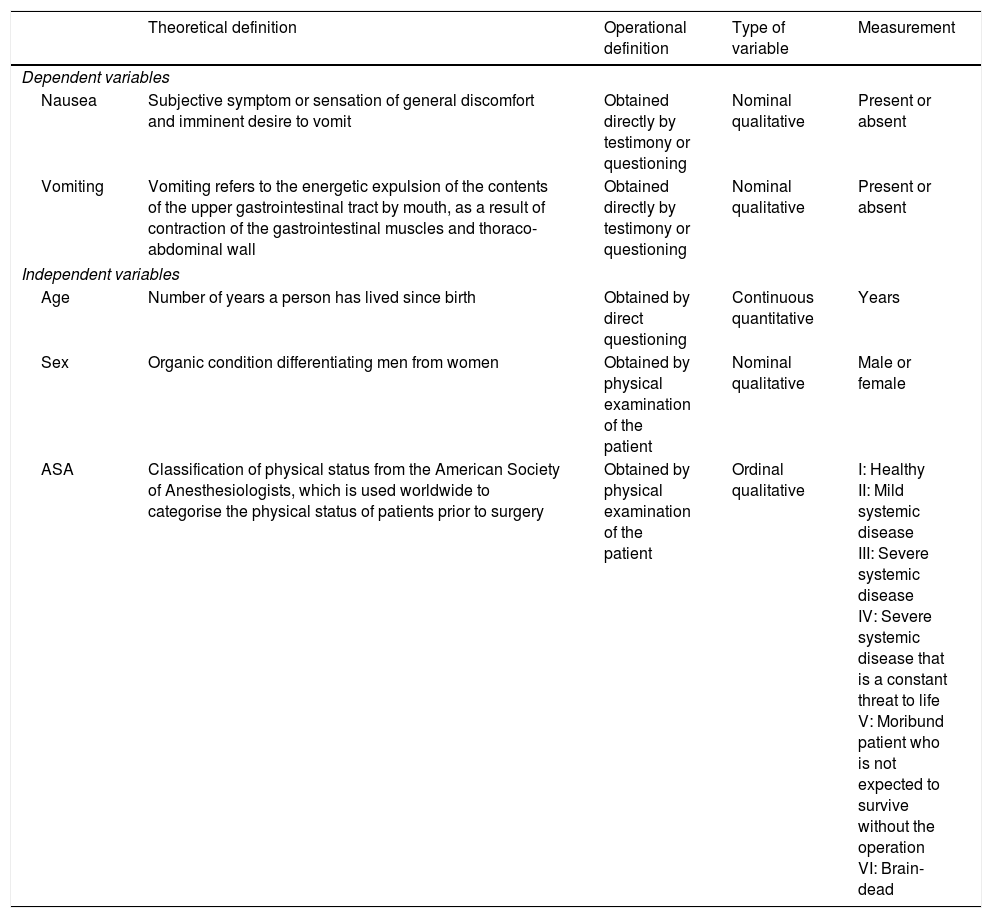
The independent variables were: age, gender and ASA classification. The dependent variables were nausea and vomiting. The definitions for each variable are shown in Table 1.
Definitions of dependent and independent variables.
| Theoretical definition | Operational definition | Type of variable | Measurement | |
|---|---|---|---|---|
| Dependent variables | ||||
| Nausea | Subjective symptom or sensation of general discomfort and imminent desire to vomit | Obtained directly by testimony or questioning | Nominal qualitative | Present or absent |
| Vomiting | Vomiting refers to the energetic expulsion of the contents of the upper gastrointestinal tract by mouth, as a result of contraction of the gastrointestinal muscles and thoraco-abdominal wall | Obtained directly by testimony or questioning | Nominal qualitative | Present or absent |
| Independent variables | ||||
| Age | Number of years a person has lived since birth | Obtained by direct questioning | Continuous quantitative | Years |
| Sex | Organic condition differentiating men from women | Obtained by physical examination of the patient | Nominal qualitative | Male or female |
| ASA | Classification of physical status from the American Society of Anesthesiologists, which is used worldwide to categorise the physical status of patients prior to surgery | Obtained by physical examination of the patient | Ordinal qualitative | I: Healthy II: Mild systemic disease III: Severe systemic disease IV: Severe systemic disease that is a constant threat to life V: Moribund patient who is not expected to survive without the operation VI: Brain-dead |
The study was blinded, meaning that the type of antiemetic drug administered was not revealed to the patients or to the investigator responsible for the methodology. Patients were randomised using simple randomisation tables by recording the patient number in a notebook where a code was assigned for later evaluation.
Patients of both sexes aged 18–60 years with an ASA 1 or ASA 2 status who underwent nasal surgery were included. Patients who received induction anaesthesia with propofol, undergoing chemotherapy or radiotherapy management, preoperative antiemetic treatment, or with a known allergy to propofol, egg or ondansetron were excluded; patients requiring surgical reintervention or who were administered other antiemetic drugs in the postoperative period were eliminated.
ProcedureAfter obtaining informed consent and receiving approval from the institutional research ethics committees (Hospital General de México No. DI/15/203/03/28), 46 patients were studied and divided into two groups by simple randomisation using a randomisation table created and implemented by the principal investigator, keeping the patients blinded as they were not informed of which group they were in or what type of drug would be administered. All the patients received balanced general anaesthesia using thiopental (5mg/kg) as an inducer, rocuronium (600mcg/kg) as a muscle relaxant, and a fentanyl perfusion as an analgesic (plasma concentration 2–4ng/ml, i.e. 0.026–0.052mcg/kg/min), all administered intravenously with the dose adjusted per kilogram of ideal body weight. The volatile anaesthetic of choice was desflurane at 1.0 MAC. Midazolam (30mcg/kg) was used as a pre-anaesthesia medication, adjusted per kilogram of body weight; intravenous metamizole (30mg/kg) was used for postoperative analgesia. Type I monitoring was used, which consisted of non-invasive blood pressure, pulse oximetry, temperature, 5-lead electrocardiogram, capnography and gas analysis; mechanical ventilation was in volume control mode with lung protection measures. Group A received intravenous ondansetron 4mg and Group B received intravenous propofol 20mg; both drugs were supplied at the end of surgery.
The presence or absence of nausea and vomiting in the immediate postoperative period and 2, 4 and 6h afterwards was recorded on a case report form.
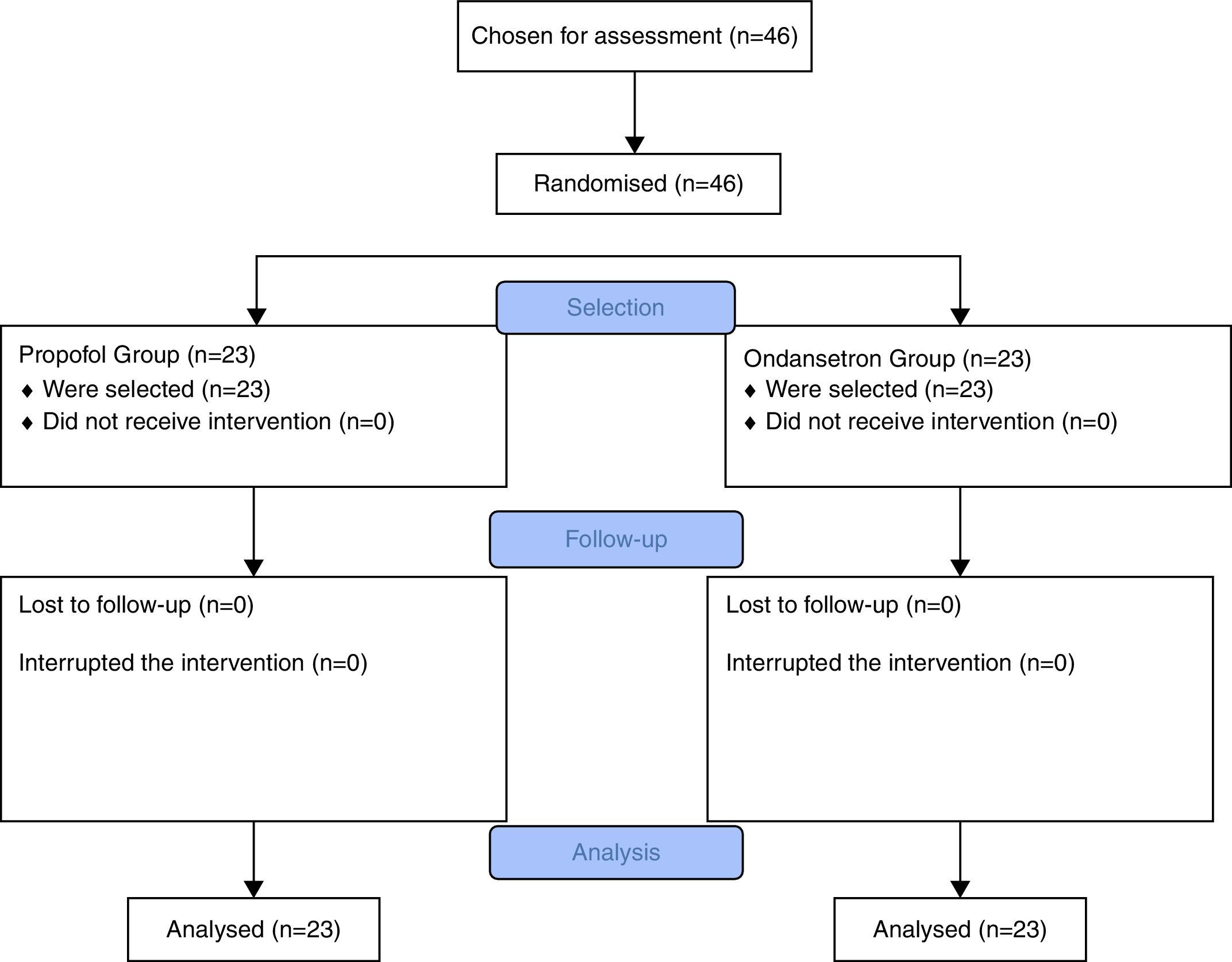
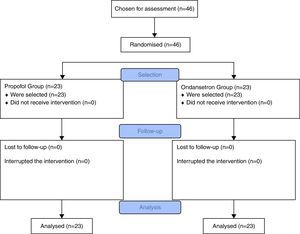
Selection, follow-up and analysis is summarised in the flow chart in Fig. 1.
Statistical analysisFor the statistical analysis, descriptive statistical measures such as simple frequencies, percentages and proportions were used. The data were analysed with Student's two-tailed t-test for independent samples.
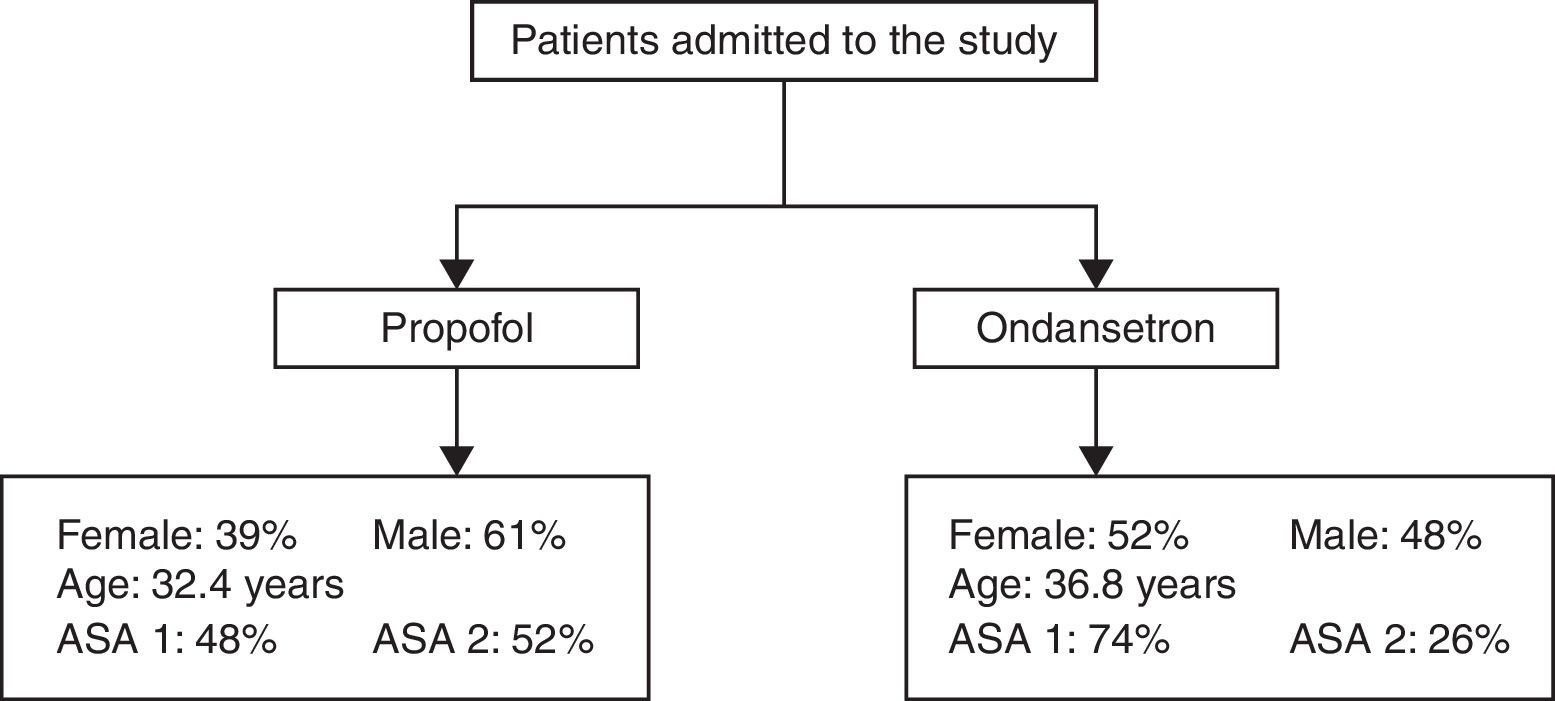
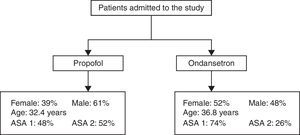
ResultsOf the total propofol group sample (N=23), 61% were male and the remaining 39% female; for the ASA classification, 11 patients (48%) were classified as ASA 1 and 12 were ASA 2 (52%). The ondansetron group was comprised of 12 (52%) men and 11 (48%) women; for the ASA classification 74% were ASA 1 and the remaining 26% were ASA 2. This is shown in Fig. 2.
The ages of the sample (N=46) went from 18 years as the lower limit to 59 years as the upper limit. The mean age was 33 years.
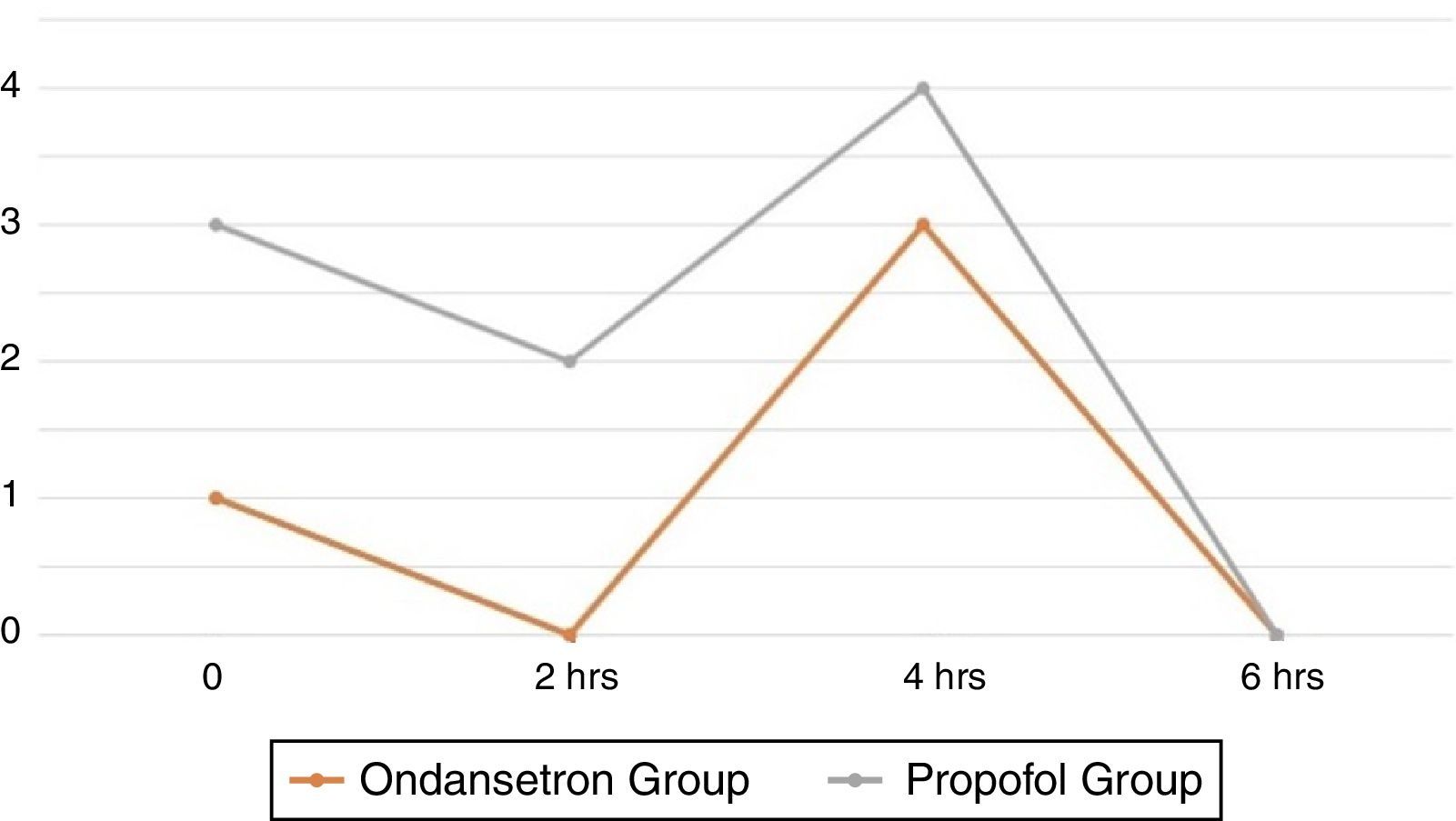
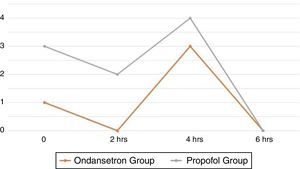
By comparing the presence of nausea between the two groups, it was found that there was an immediate postoperative presence in 4% of the patients in the propofol group and in 9% in the ondansetron group, with p=0.550; no statistically significant differences were found. Two hours after surgery, the presence of nausea was only 9% in the group of patients who received ondansetron, p=0.148; no significant differences. Four hours after the surgery, 13% of the patients in the propofol group had nausea and 4% of the ondansetron group; as p=0.295 this difference was not statistically significant.
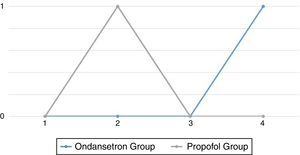
The differences in the frequency of nausea are shown in Fig. 3.
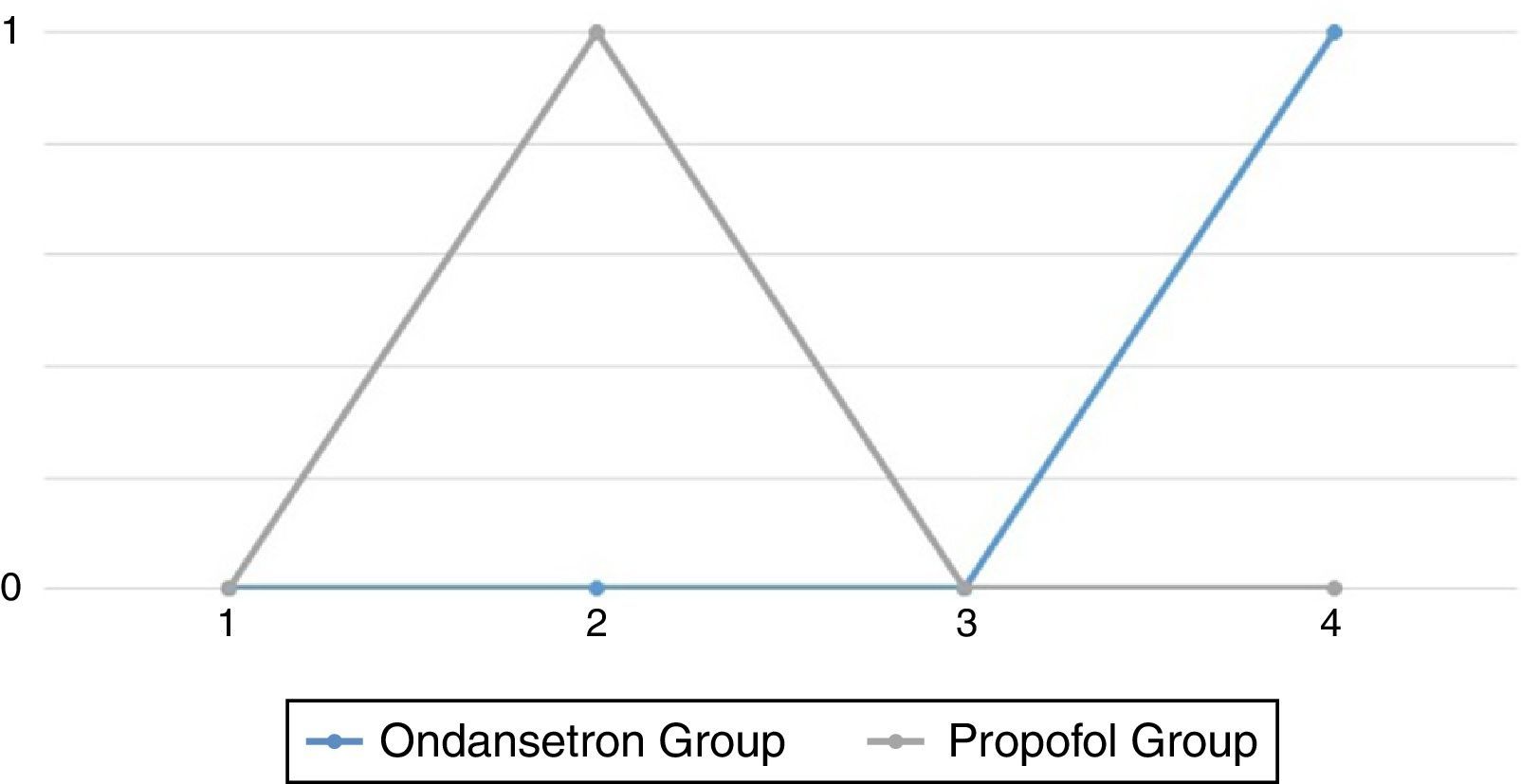
Six hours after the surgery, 4% of the patients who received propofol presented vomiting, with p=0.312; in the ondansetron group, 4% presented vomiting 2h after the surgery, p=0.312; there were no statistically significant differences. The difference in the frequency of vomiting between the two groups is shown in Fig. 4.
DiscussionThe importance motivating this research is focused on the high level of reported incidence of postoperative nausea and vomiting. Together with the increased hospital costs and the fear towards this condition felt by patients, this makes it a topic of special interest for anaesthetists.
The impact of this research study is based on the fact that 5-hydroxytryptamine antagonists (ondansetron), which are considered the gold standard for postoperative nausea and vomiting prophylaxis and treatment, are not always available worldwide; but propofol is available, which is the most recently developed anaesthesia inducer by the pharmaceutical industry and perhaps the most commonly used for general anaesthesia in the world.
The results obtained in this randomised, prospective, longitudinal, blind, comparative clinical trial regarding the incidence of postoperative nausea and vomiting in nasal surgery by measuring the prophylactic effect of ondansetron and propofol suggest the following:
Despite having been randomly assigned to either of the two groups, the study population shows a homogeneity in terms of sex, ASA classification and age. The mean age was 33 years, with a minimum age of 18 years and a maximum age of 59.
The presence of immediate postoperative nausea was similar in both groups, with p=0.550; 2h afterwards, only the ondansetron group presented nausea with p=0.148; 4h afterwards, p=0.295; 6h after surgery, there was no nausea in any of the patients evaluated. As for vomiting, this was present in 4% of the patients in the ondansetron group 2h after surgery with p=0.312, while the propofol group presented the same percentage 6h after surgery, with p=0.312.
The protection exercised by ondansetron to prevent postoperative nausea and vomiting showed no statistically significant difference with respect to propofol, in line with the study published by Kalidag et al.17 They found an identical decrease in nausea and vomiting between propofol and ondansetron (71.4%). Splinter et al.18 found a similar efficacy even though their sample was from among the paediatric population.
The limitations of this study include the fact that the selection criteria did not take into account the risk of PONV according to the Apfel scale, which could be a bias since the probability of presenting PONV varies depending on the number of factors from the scale presented by the patient. Furthermore, the nausea and vomiting follow-up time only included the 6 postoperative hours following nasal surgery. Another weakness of the study was that the sample size was calculated with a difference of means and not proportions since efficacy was sought in an intervention measured in percentages of two populations, although the sample size was sufficient to be able to reach reliable results and conclusions.
ConclusionsUpon evaluating the efficacy of the postoperative nausea and vomiting control of propofol versus ondansetron in nasal surgery, it was observed that there is no statistically significant difference between the two drugs in terms of protection, which leads to thinking that administering propofol or ondansetron is equally effective for postoperative antiemetic prophylaxis.
This research still needs to be expanded, using larger samples and evaluating other types of surgery, using different therapeutic measures for pain control, and surveying the subjective perception of the patients; however it opens a new, easy-access, low-cost option in the therapeutic arsenal available to anaesthetists.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Conflict of interestThe authors declare that they have no conflict of interests.