Cervical adenocarcinoma has increased in recent years, and there is no early form of detection other than cervicovaginal cytology, which has a high sensitivity and specificity for squamous lesions, but poor sensitivity in detecting adenocarcinoma. In our hospital, previous research on this topic has not been done.
ObjectiveTo know the number of cases of cervical adenocarcinoma diagnosed by cervicovaginal cytology, as well as the degree of discordance by histopathological study.
Material and methodA cytohistological correlation was performed in 82 of 120 cases diagnosed as “adenocarcinoma” in cervical cytology at the General Hospital of Mexico “Dr. Eduardo Liceaga “in the period from 2007 to 2016.
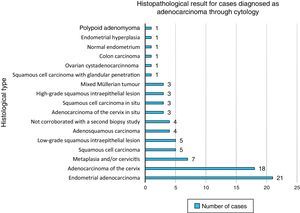
Results82 cases with biopsy study by the Surgical Pathology service were categorised into 25 cases (30.48%) of adenocarcinoma of the cervix, 21 (25.60%) of adenocarcinoma of the endometrium, 17 (20.73%) squamous lesions, 7 (8.53%) changes by metaplasia or cervicitis, 3 (3.65%) mixed Müllerian tumours, and 1 case (1.21%) of the following: papillary cystadenocarcinoma of the ovary, colonic mestastasic adenocarcinoma, endometrial hyperplasia, normal endometrium and polypoid adenomyoma. Four cases (4.87%) did not have an adequate biopsy at the first time, and the diagnosis could not be corroborated.
ConclusionsCervicovaginal cytology is a useful tool for the detection of glandular lesions, however, it is difficult to discriminate on origin only through morphology, since many other entities overlap.
El adenocarcinoma cervicouterino se ha incrementado en los últimos años, y no existe hasta la fecha una forma de detección temprana diferente a la citología cervicovaginal, la cual cuenta con una alta sensibilidad y especificidad para lesiones escamosas, pero pobre sensibilidad en la detección de lesiones glandulares. En nuestro hospital no se han realizado previas investigaciones sobre este tema.
ObjetivoConocer el número de casos de adenocarcinoma cervicouterino diagnosticados mediante citología cervicovaginal, así como el grado de discordancia mediante el estudio histopatológico.
Material y métodoSe realizó la correlación citohistológica de 82 de 120 casos diagnosticados como «adenocarcinoma» en citología cervicouterina en el Hospital General de México «Dr. Eduardo Liceaga» en el periodo comprendido entre el 2007 al 2016.
ResultadosLos 82 casos que contaban con estudio de biopsia por parte del servicio de Patología Quirúrgica fueron categorizados en: 25 casos (30.48%) de adenocarcinoma de cérvix, 21 (25.60%) de adenocarcinoma de endometrio, 17 (20.73%) de lesiones escamosas puras, 7 (8.53%) cambios por metaplasia o cervicitis, 3 (3.65%) tumores mixtos müllerianos, y 1 caso (1.21%) de cada uno de los siguientes: cistadenocarcinoma papilar de ovario, adenocarcinoma de colon metastásico, hiperplasia endometrial, endometrio sin alteraciones y adenomioma polipoide. Cuatro casos (4.87%) no contaron con una biopsia adecuada en la primera toma, y no pudo ser corroborado el diagnóstico.
ConclusionesLa citología cervicovaginal es una herramienta útil para la detección de las lesiones glandulares, sin embargo, resulta difícil poder discriminar su origen mediante la morfología, pues muchas entidades se sobreponen.
In 2015, cervical carcinoma represented the fourth most common neoplasm in women worldwide, with an estimate of 528,000 new cases diagnosed annually, 85% of which were recorded in developing countries. In Latin America, it is the second most common neoplasm, with an incidence of 21.2 cases per 100,000 women and a mortality rate of 8.7 deaths per 100,000 women. The situation in Mexico is similar to that of Latin America, with an incidence of 23.3 cases per 100,000 women. The Mexican states with the greatest rates of mortality due to cervical cancer are Morelos (18.6), Chiapas (17.2) and Veracruz (16.4).1
The Oncology Department at Hospital General de México analysed 2706 patients with cervical carcinoma from 2000 to 2007. Of these patients, 219 had adenocarcinoma, which represents an incidence of this disease of 8% at our hospital.2
Cervicovaginal cytology is used as a screening test for early detection of lesions, mainly high-grade squamous cell exocervical lesions. Glandular lesions may be detected indirectly, with a sensitivity of up to 55–70% in lesions in situ,3 which, according to the 2014 Bethesda system, encompass both endometrial and endocervical glandular cells, as well as glandular cells of non-specific origin, which are reported only when there is atypia or they are of endometrial origin in women over 45 years of age.4
Although squamous cell carcinoma of the cervix remains the most common histological type worldwide,4 the incidence of endocervical adenocarcinoma has doubled to 32% in the last 5 decades, mainly in white women, accounting for 5–30% of all cervical carcinomas.5 In developed countries, such as the United Kingdom, it went from an incidence of 13.3% in 1989 to an incidence of 22.1% in 2009, whereas the proportion of squamous cell carcinomas remained nearly constant (2.3–3.6%). This increase was mainly noted in white and young women; up to 78% of cases were in women under 30 years of age.6 In the United States, an increase of 107.4% in adenocarcinoma relative to cervical cancer in general has been reported; this increase was 95.2% relative to squamous cell carcinoma.7
As in squamous cell carcinoma of the cervix, precursor lesions to cervical adenocarcinoma are also linked to HPV (human papilloma virus); high-risk serotypes 18 and 45 are most commonly detected (in up to 77% of cases), whereas serotype 16 (mostly linked to squamous cell lesions) is expressed in only 27% of cases.8 Therefore, it is not uncommon to find a link between squamous cell carcinoma in situ of the cervix and cervical adenocarcinoma.
Some studies have demonstrated that, following regular 3–5-year screening tests, with negative results through cervicovaginal cytology, early-stage adenocarcinoma lesions are more likely to be detected.6 Its low sensitivity is probably secondary to the difficulty of obtaining a suitable endocervical sample and, in part, due to poor interpretation during the reading of the slide.5,8
Techniques such as Thinprep have been shown to have greater sensitivity and specificity in detecting lesions low-grade squamous cell lesions, high-grade squamous cell lesions and glandular lesions as well as subsequent usefulness for detecting HPV through molecular techniques.9 However, artefacts due to poor fixation and loss of architecture (formation of rosettes and feathered edges) during processing may complicate the diagnosis.10
Despite major advances in medicine, there is no other suitable method for detection of cervical adenocarcinoma, and its prevention has not been entirely achieved through cervicovaginal cytology.3
Adenocarcinoma not only affects deeper, more internal areas, with the development of precancerous lesions in the cervical canal that are more difficult to sample,9 but also tends to be asymptomatic and undetectable through colposcopy until it has reached advanced stages.11
Only half of adenocarcinomas are exophytic, polypoid or papillary masses. Deep penetration of the wall produces a barrel-shaped cervix, but it has been reported that up to 75% of cases have no visible lesion.12
Added to these difficulties is the fact that high-grade squamous cell lesions tend to involve the glandular epithelium, leading to erroneous interpretations in some cases.
Due to the treatment involved, it is important to determine the origin of these lesions. The role of the cytopathologist is to detect, corroborate and, to the extent possible, pin down the origin of the neoplasm, since patient follow-up and treatment will depend on this.
Studies in Mexico, such as one by Lazcano-Ponce et al., which evaluated 20 cytology interpretation centres by distributing 220 cytology specimens, demonstrated that laboratories with expertise in cervicovaginal cytology have a rate of false negative results of more than 25%, and that some even have a rate of false negative results in excess of 45%. This included 121 cases of invasive cervical carcinoma that were not identified and 31 false negative diagnoses of adenocarcinoma.13
The objectives of this study are to find out the number of cases of adenocarcinoma diagnosed by cytology within the study period and the degree of cytohistological inconsistency, to determine the most common causes of discrepancy and to establish the sensitivity of cytology for diagnosing cervical adenocarcinoma.
Material and methodsThis was a retrospective, descriptive study. The electronic database of the Cytopathology Department at Hospital General de México “Dr. Eduardo Liceaga” from 1 January 2007 to 30 April 2016 was consulted, and cases with a cytological diagnosis of adenocarcinoma based on the 2014 Bethesda system were selected. Cases with no histopathological study were excluded. If there was more than one cytology study, the one performed closest to the biopsy was taken into account. If there was more than one histological specimen per patient, the specimen providing greater diagnostic precision (e.g. hysterectomy over incisional biopsy) was taken into account, as was the immunohistochemical study corroborating its origin.
After the data were obtained, descriptive statistics with measures of central tendency mean, median and mode and determination of sensitivity were used.
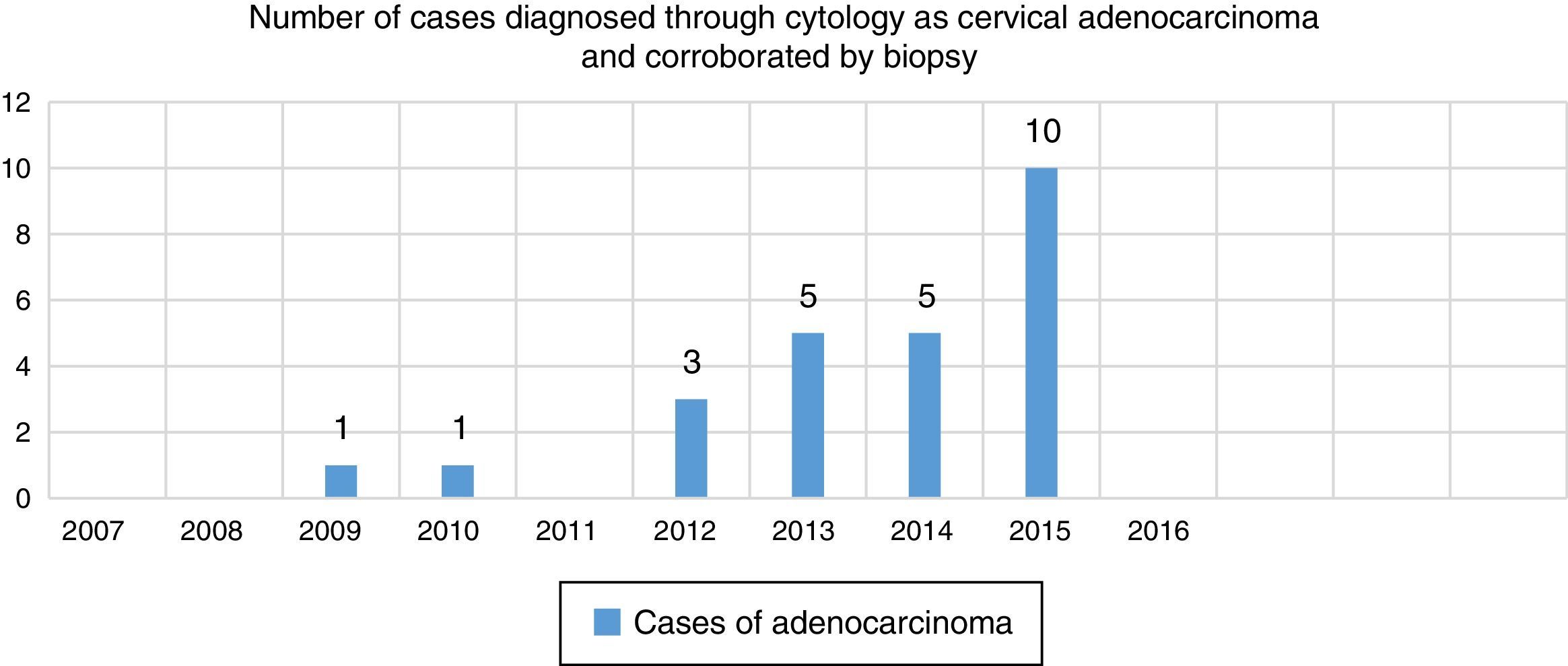
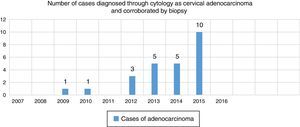
ResultsIn the Cytopathology Department at Hospital General de México “Dr. Eduardo Liceaga” 92,434 cervicovaginal cytology tests were diagnosed between 1 January 2007 and 30 April 2016. Of them, 120 were diagnosed as adenocarcinoma, but only 82 had a histopathological study.
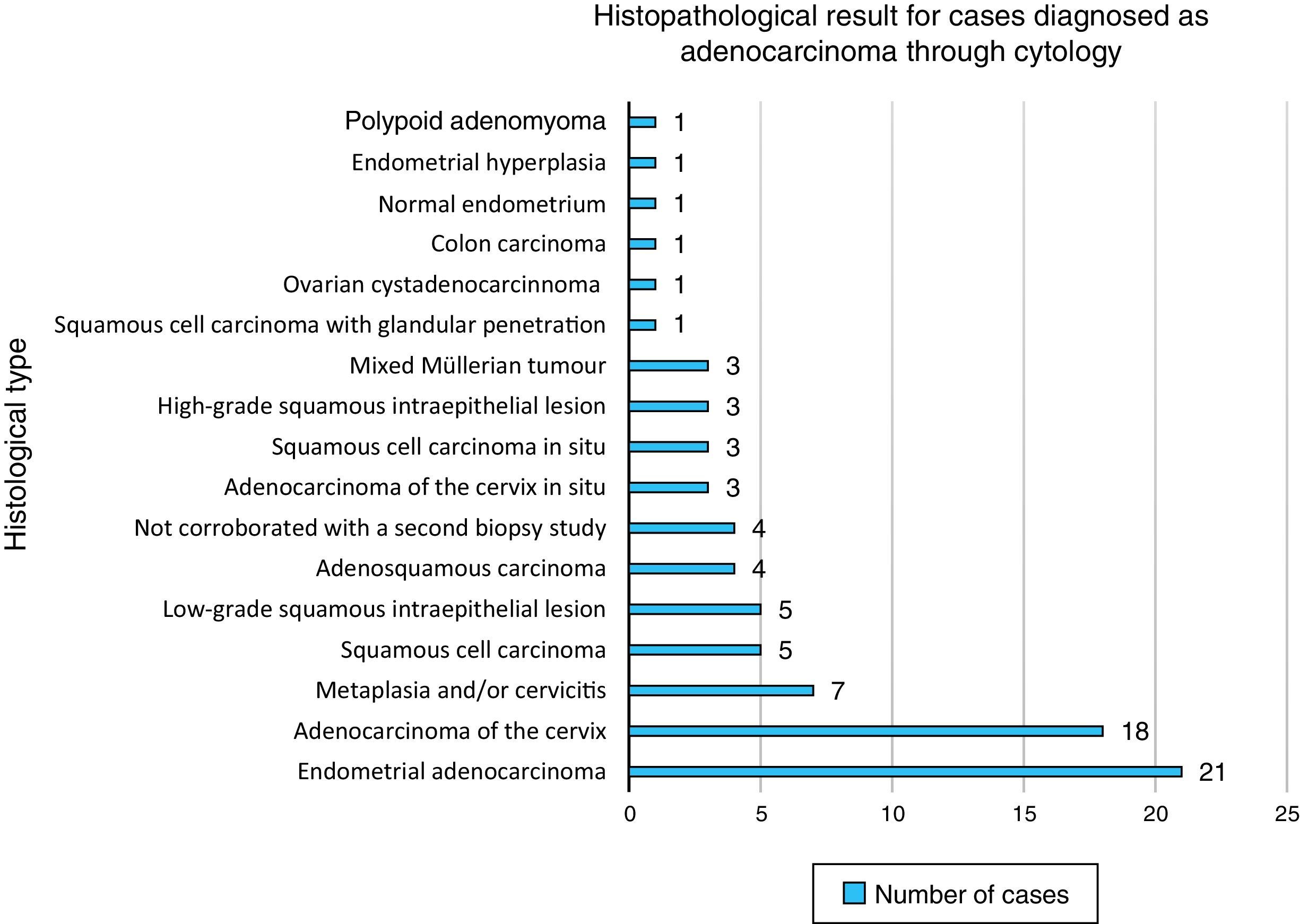
Cases were classified based on the diagnosis from the histopathological study. The most common diagnosis was adenocarcinoma of the cervix, with 25 cases (30.48%), followed by endometrial adenocarcinoma, with 21 cases (25.60%), and pure squamous cell lesions, with 17 cases (20.73%). Changes due to metaplasia and/or cervicitis occupied fourth place with 7 cases (8.53%), and mixed Müllerian tumours occupied fifth place with 3 cases (3.65%).
The other diagnoses had one case: papillary ovarian cystadenocarcinoma, metastatic colon adenocarcinoma, endometrial hyperplasia, endometrium with no abnormalities and polypoid adenomyoma (1.21%). Finally, 4 cases did not have a suitable biopsy at the first attempt, and the diagnosis could not be corroborated (4.87%) (Chart 1).
Sensitivity for detecting primary glandular malignant neoplastic cervical lesions through the use of cervicovaginal cytology at Hospital General de México was 30.48% (Chart 2). In retrospect, up to 62.14% of cases (51) diagnosed as adenocarcinoma by cytology were consistent, as neoplastic glandular elements were present in the biopsy study.
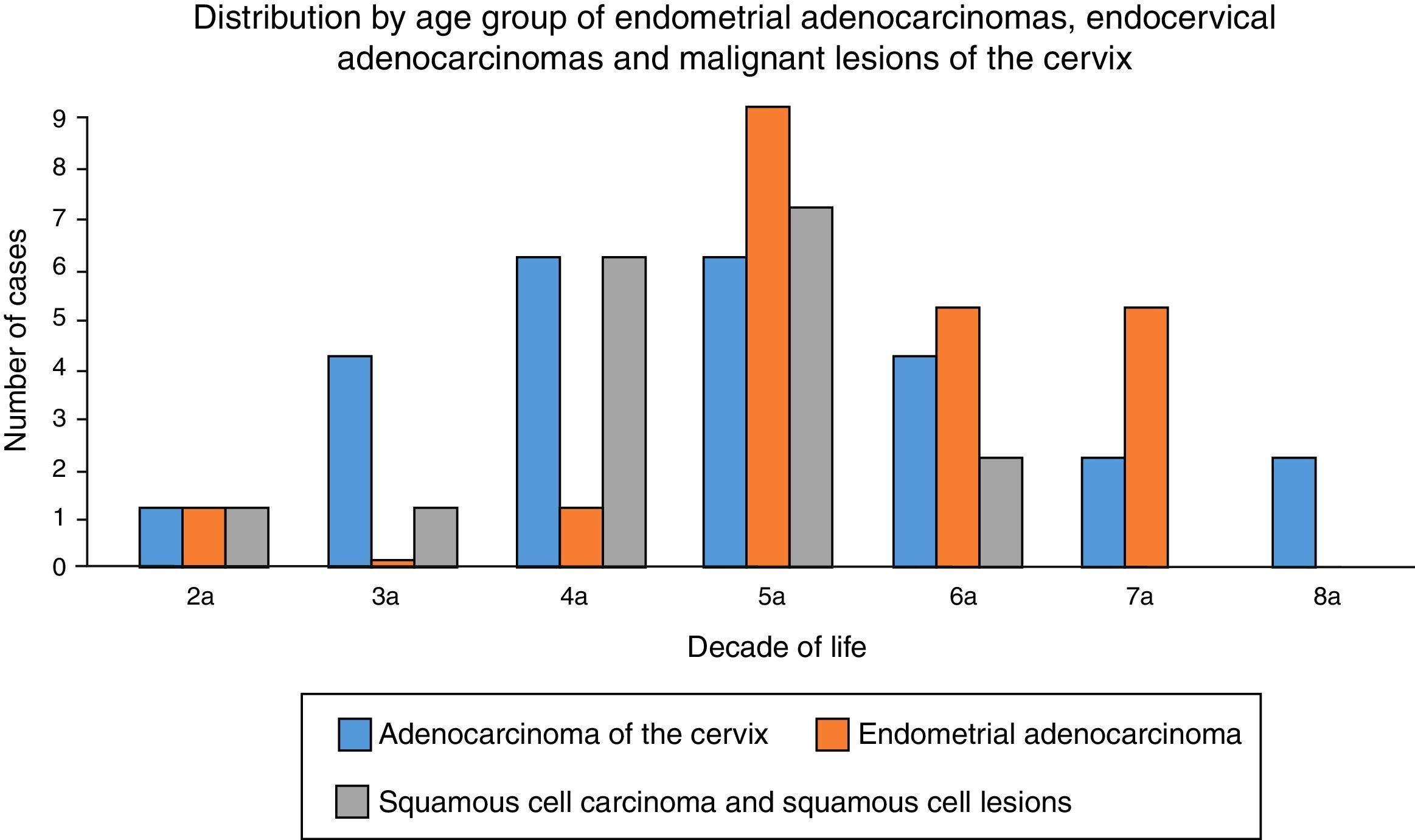
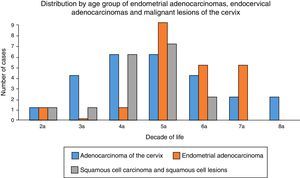
Moreover, the age range of the patients with this diagnosis was 25–83 years, with an average age of 52.58 years; the fifth decade of life was the most common (Chart 3).
DiscussionAt Hospital General de México, up to 30% of adenocarcinomas diagnosed by cervicovaginal cytology were primary cervical adenocarcinomas. This is the best method for detecting these lesions due to its cost/benefit ratio. Their diagnosis is a challenge for current medicine, since their frequency is increasing worldwide, with no highly effective method for early detection.
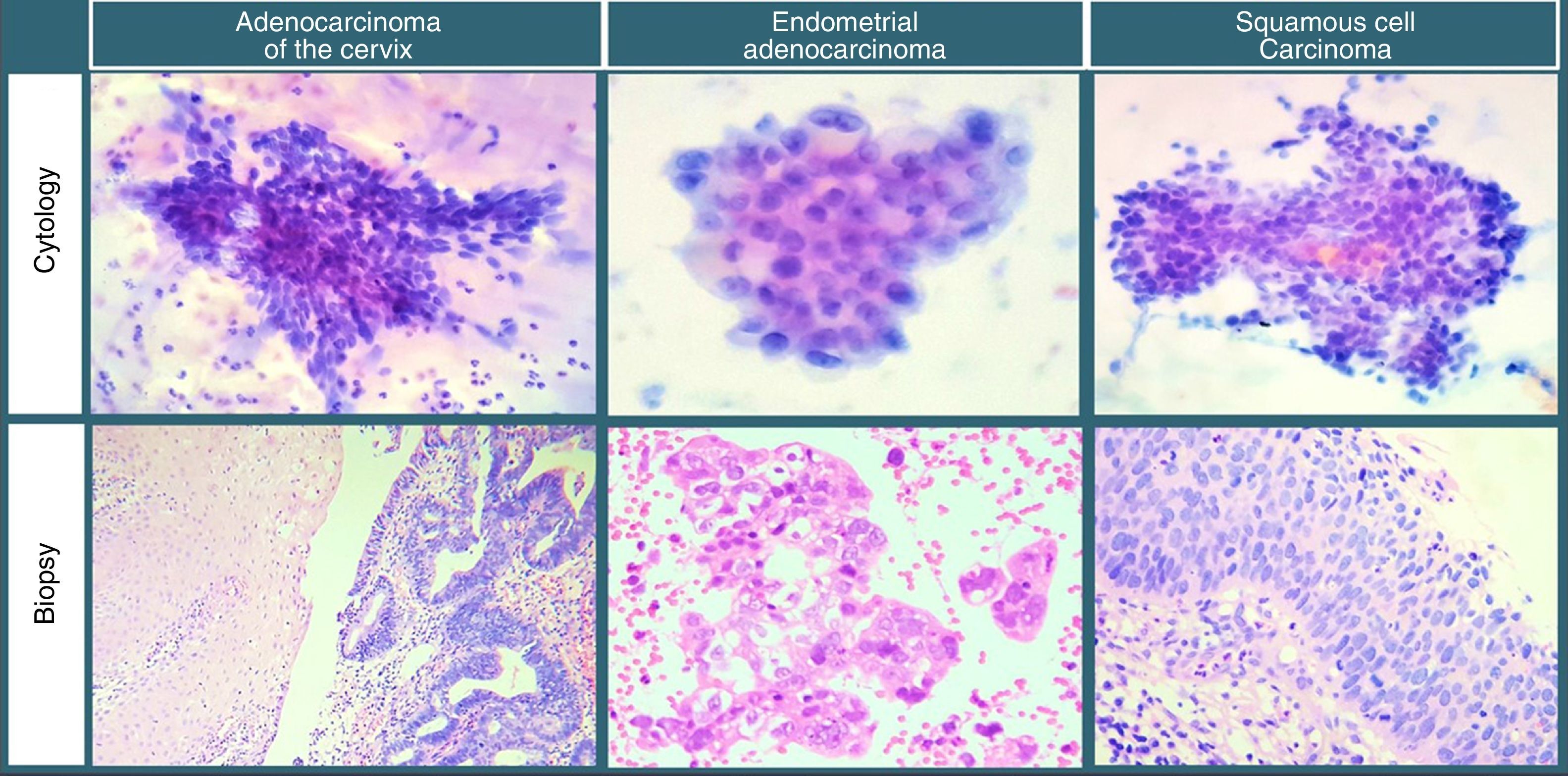
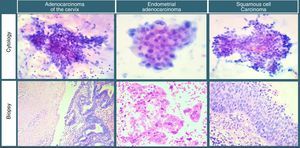
After adenocarcinoma of the cervix, endometrial adenocarcinoma and squamous cell lesions were the cases most commonly diagnosed as adenocarcinomas through cervicovaginal cytology (Image 1). This challenge presents itself due to cytological variants, the most common being mucinous, endometrial and clear-cell; these may also be found in the endometrium.
Some immunohistochemical markers may be used to determine their endocervical origin, such as positivity for the carcinoembryonic antigen, with negativity for oestrogen and vimentin receptors, thereby preventing diagnostic errors to the extent possible.11,12
Very few adenocarcinomas were from extrauterine sites. This is consistent with the literature, which features reports of carcinomas of the ovary and Fallopian tube, and even metastatic lesions to the cervix,3 such as extramammary Paget disease of the cervix, neuroendocrine carcinomas and even pancreatic tumours, which are rare due to the limited vascular and lymphatic supply of the cervix, but which have been shown to be capable of deriving from direct invasion by a contiguous organ or haematogenous, lymphoid or transcoelomic dissemination.14–16
Ten cases corresponded to non-neoplastic lesions, which, consistent with the literature, may be confused with glandular lesions, such as tubal metaplasia, reactive endocervical cells, changes due to an intrauterine device and endocervical polyps.4
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingExisting resources at the hospital.
Conflict of interestIt is hereby declared that there are no conflicts of interest in the publication and/or authorship of this article.