To evaluate whether nutritional intervention through a diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols reduces acute gastrointestinal toxicity by pelvic teletherapy in patients with gynaecological tumours.
Material and methodsA prospective unicentric randomised clinical trial comparing patients on a diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols versus a standard Mexican diet, designed to detect a decrease from 80% of grade 1–2 acute gastrointestinal toxicity in the normal diet group versus a 25% of acute gastrointestinal toxicity grade 1–2 in patients assigned to a diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols.
ResultsThirteen patients were recruited per group, with a higher gastrointestinal toxicity in the normal diet group, grade 1–2 (85% vs 77%) and 3 (23% vs 0%) compared to the diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols (p 0.16). The diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols group had a lower symptom score at the end of treatment in the quality of life questionnaire of patients with cervical cancer (1.41 vs 1.85, p 0.01) and a lower mean deterioration in performance status (0.61 of 0.5 vs 0.23 of 0.43, p 0.049). 85% of the patients had an excellent attachment to the diet. No significant factors associated with the presence of grade 3 gastrointestinal toxicity were found.
ConclusionThe implementation of a diet low in oligosaccharides, disaccharides, monosaccharides and fermentable polyols during treatment with pelvic teletherapy is a low cost and high attachment intervention, which decreases the deterioration of functional status and symptomatology at the end of treatment in patients with cervical cancer.
Evaluar si la intervención nutricional mediante una dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables disminuye la toxicidad gastrointestinal aguda por teleterapia pélvica en pacientes con tumores ginecológicos.
Material y métodosEnsayo clínico prospectivo aleatorizado unicéntrico, que comparó a pacientes con dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables contra una dieta normal mexicana, diseñado para detectar una disminución del 80% de toxicidad gastrointestinal aguda Grado 1-2 en el grupo con dieta normal a un 25% de toxicidad gastrointestinal aguda Grado 1-2 en pacientes con dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables.
ResultadosSe reclutaron 13 pacientes por grupo, reportándose una mayor toxicidad gastrointestinal en el grupo de dieta normal grado 1-2 (85% vs 77%) y 3 (23% vs 0%) respecto a la dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables (p 0.16), el grupo de dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables tuvo un menor puntaje de sintomatología al final del tratamiento en el cuestionario de calidad de vida de las pacientes con cáncer cervicouterino (1.41 vs 1.85, p 0.01) y un menor deterioro promedio en el estado funcional (0.61 DE 0.5 vs 0.23 DE 0.43, p 0.049). El 85% de las pacientes tuvieron un apego excelente a la dieta. No se encontraron factores asociados a la presencia toxicidad gastrointestinal grado 3.
ConclusiónLa implementación de una dieta baja en oligosacáridos, disacáridos, monosacáridos y polioles fermentables durante el tratamiento con teleterapia pélvica es una medida de bajo costo y alto apego, que disminuye el deterioro de estado funcional en las pacientes con tumores ginecológicos la sintomatología al final del tratamiento en pacientes con cáncer cervicouterino.
Malignant tumours of the cervix and uterine corpus represent the fourth and sixth leading tumours in women in terms of incidence, as well as the fourth and fourteenth leading tumours in terms of cancer mortality worldwide, respectively. In women in Mexico, cervical cancer is the second most common cancer in terms of incidence and mortality, while uterine cancer is the ninth most common cancer in terms of incidence and the thirteenth most common cancer in terms of mortality. These figures are expected to increase by 2020.1,2
Treatment with external radiotherapy or teletherapy is used in 60–71% of women with cervical cancer, as well as 38–45% of those with uterine tumours at some point in the course of their disease.3–5 Its main toxicity is gastrointestinal, which occurs in mild to moderate grades in 70–90% of patients and in severe grades (3–5) in around 3%.6 Its incidence and severity are increased by common factors such as prior surgery and concomitant chemotherapy, which doubles the risk of grade ≥3 gastrointestinal toxicity.7
Women who experience acute gastrointestinal toxicity during pelvic teletherapy experience a negative impact on their abdominal symptoms, which also affects their nutritional status and quality of life. Prolonging or suspending the treatment due to these symptoms increases the risk of achieving suboptimal outcomes in disease monitoring, life expectancy and quality of life.8
In recent decades, multiple strategies and interventions related to modifying technical aspects of the treatment have been developed to decrease gastrointestinal toxicity by means of teletherapy. Despite this, gastrointestinal toxicity remains the main adverse effect, and some measures cannot be used at all centers, due to the technical and economic requirements that they involve.9–16
Nutritional interventions are an easy-to-access, easy-to-implement option that may be used alone or in combination with other measures. However, their effectiveness in decreasing gastrointestinal toxicity has not been conclusively corroborated.17–20
Based on the lack of conclusive evidence of a decrease in gastrointestinal toxicity with nutritional interventions, which use the modification of a single dietary element in patients treated with radiotherapy, the advantage of the low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet lies in the modification of multiple factors that influence enteropathy due to radiation, such as regulation of intestinal motility, restriction of lactose and osmotic agents.9,21,22 All this is coupled with the improvement observed in the abdominal symptoms of patients with inflammatory bowel disease, which bears some resemblances to damage induced by radiation in terms of pathogenesis, as well as the high compliance reported.23–27
For this reason, evaluation of this type of nutritional intervention is needed in patients treated with pelvic teletherapy in order to improve treatment tolerance as well as positively influence cancer outcomes and patient quality of life.
The main objective of this trial was to evaluate whether nutritional intervention, through a low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet, decreases acute gastrointestinal toxicity due to pelvic teletherapy in patients with gynaecological tumours compared to a normal Mexican diet.
Material and methodsPatient selection and eligibility criteriaPatients diagnosed with cervical cancer or endometrial cancer treated at the Mexican National Medical Center of the Northeast of the Mexican Social Security Institute (UMAE 25) in Monterrey, Nuevo León, Mexico, were enrolled. To be considered eligible, they had to be between 18 and 70 years of age when they enrolled in the study; have histopathological corroboration of their diagnosis; have a performance status of 0–2 according to the Eastern Cooperative Oncology Group (ECOG) scale; have suitable kidney, liver and bone marrow function; not be pregnant or in the postpartum period; and be candidates for radical or adjuvant treatment with teletherapy with or without concomitant chemotherapy. Patients with prior pelvic radiotherapy treatment, inflammatory bowel disease, active severe comorbidity, active collagen disease or distant metastases according to studies of the spread of their cancer with chest X-ray or an abdominal and pelvic CT scan were excluded.
Before the study started, the protocol was approved by the Local Research and Ethics Committee in Health Research, and informed consent to participate in the study was obtained from the patients in accordance with institutional guidelines.
SurgeryPatients treated with primary surgery who were candidates for adjuvant treatment were treated with hysterectomy plus bilateral salpingo-oophorectomy with or without lymphadenectomy.
ChemotherapyIn patients who were candidates for concomitant chemotherapy, cisplatin was used at a dose of 40mg/m2 on days 1, 8, 15, 22 and 29 of radiotherapy. If cisplatin was contraindicated, then carboplatin was used at an area under the curve dose of 1.5 in accordance with the Calvert formula.
RadiotherapyAll patients received teletherapy to the pelvis with four fields, using a three dimensional conformal radiation therapy technique to deliver a dose of 50Gy in fractions of 2Gy or 50.4Gy in fractions of 1.8Gy, using 6MV or 18MV photons to cover 95% of the planning treatment volume with the specified dose.
DietThe types of diet to be assigned consisted of a low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet specified in a nutritional guide. Adherence to this diet was evaluated using weekly self-evaluation with a Likert scale, with adherence values of more than 75% of the time, 50–75% of the time, 25–50% of the time and less than 25% of the time. The other diet consisted of a normal Mexican diet, in accordance with the recommendations of Mexican Official Standard NOM-043-SSA2-2012, Basic Health Services, Nutritional Health Promotion and Education, Criteria for Offering Guidance.
Follow-upAt the start and end of teletherapy, symptoms, weight, performance status and quality of life were measured by administering the European Organisation for Research and Treatment of Cancer (EORTC) QLQ C-30 questionnaire28,29 to all patients, and the specific modules for cervical cancer (CX-24)30 and endometrial cancer (EN-24)31 depending on the primary tumour.
During treatment with teletherapy, the grade of gastrointestinal toxicity was evaluated weekly according to the United States National Cancer Institute (NCI) scale, version 4.03,32 and treatment was provided according to the grade of toxicity presented.
Study designA prospective, randomised, single-centre clinical trial was conducted in which random assignment tables were used to assign patients to the low FODMAP diet group or to the normal Mexican (NOM) diet group.
The study was designed to detect an 80% decrease in acute grade 1–2 gastrointestinal toxicity in the group with a normal diet to a 25% decrease in acute grade 1–2 gastrointestinal toxicity in patients with a low FODMAP diet, with an alpha value of 0.05, a statistical power of 80%, a rate of loss to follow-up of 10% and a case:control ratio of 1:1. It was planned to recruit 13 patients per group, with a total of 26 patients.
For the descriptive analysis of the information obtained, absolute frequencies, percentages and means or medians with standard deviation or limits were used. For the inferential analysis, the ×2 test or Fisher's exact test was used for qualitative variables, and Student's t test for independent samples or the Mann–Whitney U test was used for quantitative variables. To measure the magnitude of association, relative risk was measured with its confidence interval at 95%. A p≤0.05 was considered significant. The Statistical Package for Social Sciences (SPSS) was used for analysis of variables.
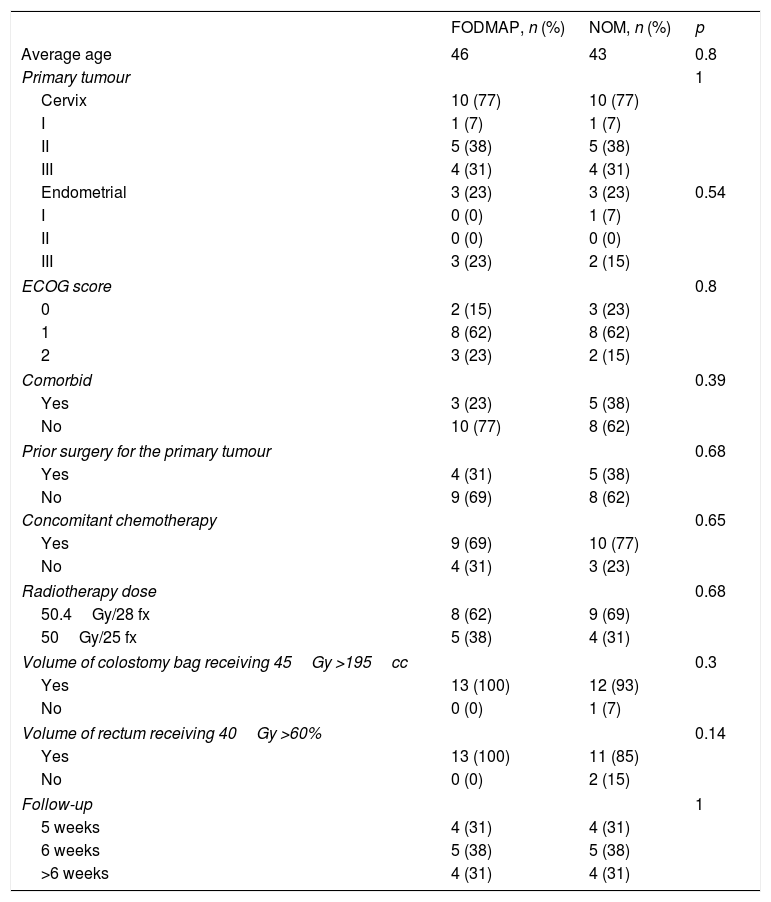
ResultsPatient characteristicsA total of 26 patients who agreed to participate in the study were recruited between August and October 2016. No significant differences between the two groups in terms of patient characteristics were found. The mean age in the low FODMAP diet group was 46 years, and the mean age in the NOM diet group was 43 years. Most patients had a diagnosis of cervical cancer (77% in both groups) and an ECOG of 1 (62% in both groups). Most treatments were radical and involved concomitant chemotherapy: 69% and 69% in the low FODMAP diet group and 62% and 77% in the NOM diet group, respectively (Table 1).
Patient characteristics.
| FODMAP, n (%) | NOM, n (%) | p | |
|---|---|---|---|
| Average age | 46 | 43 | 0.8 |
| Primary tumour | 1 | ||
| Cervix | 10 (77) | 10 (77) | |
| I | 1 (7) | 1 (7) | |
| II | 5 (38) | 5 (38) | |
| III | 4 (31) | 4 (31) | |
| Endometrial | 3 (23) | 3 (23) | 0.54 |
| I | 0 (0) | 1 (7) | |
| II | 0 (0) | 0 (0) | |
| III | 3 (23) | 2 (15) | |
| ECOG score | 0.8 | ||
| 0 | 2 (15) | 3 (23) | |
| 1 | 8 (62) | 8 (62) | |
| 2 | 3 (23) | 2 (15) | |
| Comorbid | 0.39 | ||
| Yes | 3 (23) | 5 (38) | |
| No | 10 (77) | 8 (62) | |
| Prior surgery for the primary tumour | 0.68 | ||
| Yes | 4 (31) | 5 (38) | |
| No | 9 (69) | 8 (62) | |
| Concomitant chemotherapy | 0.65 | ||
| Yes | 9 (69) | 10 (77) | |
| No | 4 (31) | 3 (23) | |
| Radiotherapy dose | 0.68 | ||
| 50.4Gy/28 fx | 8 (62) | 9 (69) | |
| 50Gy/25 fx | 5 (38) | 4 (31) | |
| Volume of colostomy bag receiving 45Gy >195cc | 0.3 | ||
| Yes | 13 (100) | 12 (93) | |
| No | 0 (0) | 1 (7) | |
| Volume of rectum receiving 40Gy >60% | 0.14 | ||
| Yes | 13 (100) | 11 (85) | |
| No | 0 (0) | 2 (15) | |
| Follow-up | 1 | ||
| 5 weeks | 4 (31) | 4 (31) | |
| 6 weeks | 5 (38) | 5 (38) | |
| >6 weeks | 4 (31) | 4 (31) | |
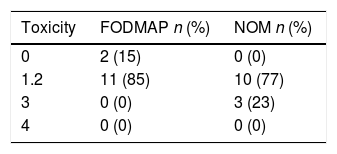
Regarding the maximum grade of gastrointestinal toxicity presented, no significant difference between the two groups was observed (p 0.16); grades 1–2 occurred in 85% of patients in the low FODMAP diet group and 77% of patients in the NOM diet group. Moreover, three grade 3 toxicity events occurred, all in the NOM diet group, corresponding to 23% of the patients assigned to this group (Table 2).
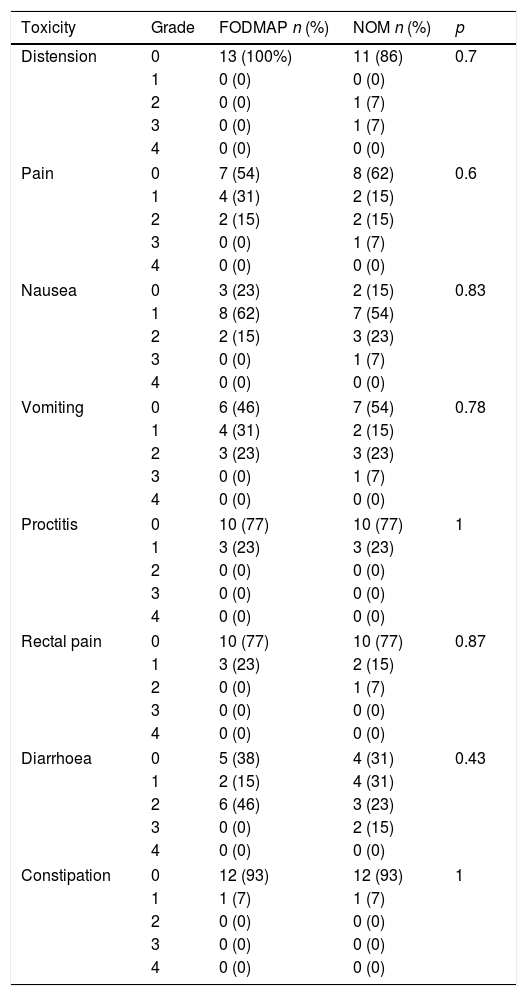
In both groups, the most common gastrointestinal toxicity was nausea, followed by vomiting (54% vs 46%) and diarrhoea (62% vs 69%). The grade 3 toxicity events presented corresponded to abdominal distension, abdominal pain, nausea, vomiting and diarrhoea (Table 3).
Type of gastrointestinal toxicity and grade of presentation according to assigned diet.
| Toxicity | Grade | FODMAP n (%) | NOM n (%) | p |
|---|---|---|---|---|
| Distension | 0 | 13 (100%) | 11 (86) | 0.7 |
| 1 | 0 (0) | 0 (0) | ||
| 2 | 0 (0) | 1 (7) | ||
| 3 | 0 (0) | 1 (7) | ||
| 4 | 0 (0) | 0 (0) | ||
| Pain | 0 | 7 (54) | 8 (62) | 0.6 |
| 1 | 4 (31) | 2 (15) | ||
| 2 | 2 (15) | 2 (15) | ||
| 3 | 0 (0) | 1 (7) | ||
| 4 | 0 (0) | 0 (0) | ||
| Nausea | 0 | 3 (23) | 2 (15) | 0.83 |
| 1 | 8 (62) | 7 (54) | ||
| 2 | 2 (15) | 3 (23) | ||
| 3 | 0 (0) | 1 (7) | ||
| 4 | 0 (0) | 0 (0) | ||
| Vomiting | 0 | 6 (46) | 7 (54) | 0.78 |
| 1 | 4 (31) | 2 (15) | ||
| 2 | 3 (23) | 3 (23) | ||
| 3 | 0 (0) | 1 (7) | ||
| 4 | 0 (0) | 0 (0) | ||
| Proctitis | 0 | 10 (77) | 10 (77) | 1 |
| 1 | 3 (23) | 3 (23) | ||
| 2 | 0 (0) | 0 (0) | ||
| 3 | 0 (0) | 0 (0) | ||
| 4 | 0 (0) | 0 (0) | ||
| Rectal pain | 0 | 10 (77) | 10 (77) | 0.87 |
| 1 | 3 (23) | 2 (15) | ||
| 2 | 0 (0) | 1 (7) | ||
| 3 | 0 (0) | 0 (0) | ||
| 4 | 0 (0) | 0 (0) | ||
| Diarrhoea | 0 | 5 (38) | 4 (31) | 0.43 |
| 1 | 2 (15) | 4 (31) | ||
| 2 | 6 (46) | 3 (23) | ||
| 3 | 0 (0) | 2 (15) | ||
| 4 | 0 (0) | 0 (0) | ||
| Constipation | 0 | 12 (93) | 12 (93) | 1 |
| 1 | 1 (7) | 1 (7) | ||
| 2 | 0 (0) | 0 (0) | ||
| 3 | 0 (0) | 0 (0) | ||
| 4 | 0 (0) | 0 (0) | ||
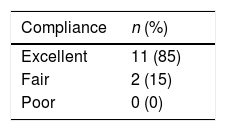
Adherence to the diet was considered excellent when a score for adherence to the diet of more than 75% was obtained using the Likert scale in 50% or more of the weeks evaluated. A percentage of 50–75% was considered fair adherence, and a percentage of less than 50% was considered non-adherence. Table 4 reports the data on adherence to the low FODMAP diet, which show excellent adherence to the diet in 85% of patients.
Excellent adherence to this diet was not significantly associated with prevention of the development of any grade of gastrointestinal toxicity, with an odds ratio of 0.93 (95% CI 0.93–11.77, p 0.96).
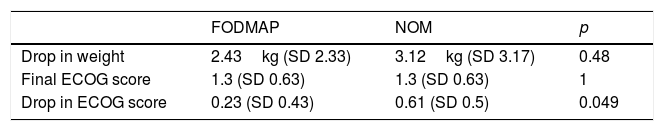
Weight loss and performance statusIn the evaluation at the end of treatment, a greater average decline in performance status was observed in patients assigned to the NOM diet group compared to patients assigned to the low FODMAP diet (0.23 [SD 0.43] vs 0.61 [SD 0.5], p=0.04).
No significant difference in terms of weight loss at the end of treatment between the two groups was observed, with an average decrease of 2.43kg (SD 2.33) in the low FODMAP diet group and 3.12kg (SD 3.17) in the NOM diet group, respectively (Table 5).
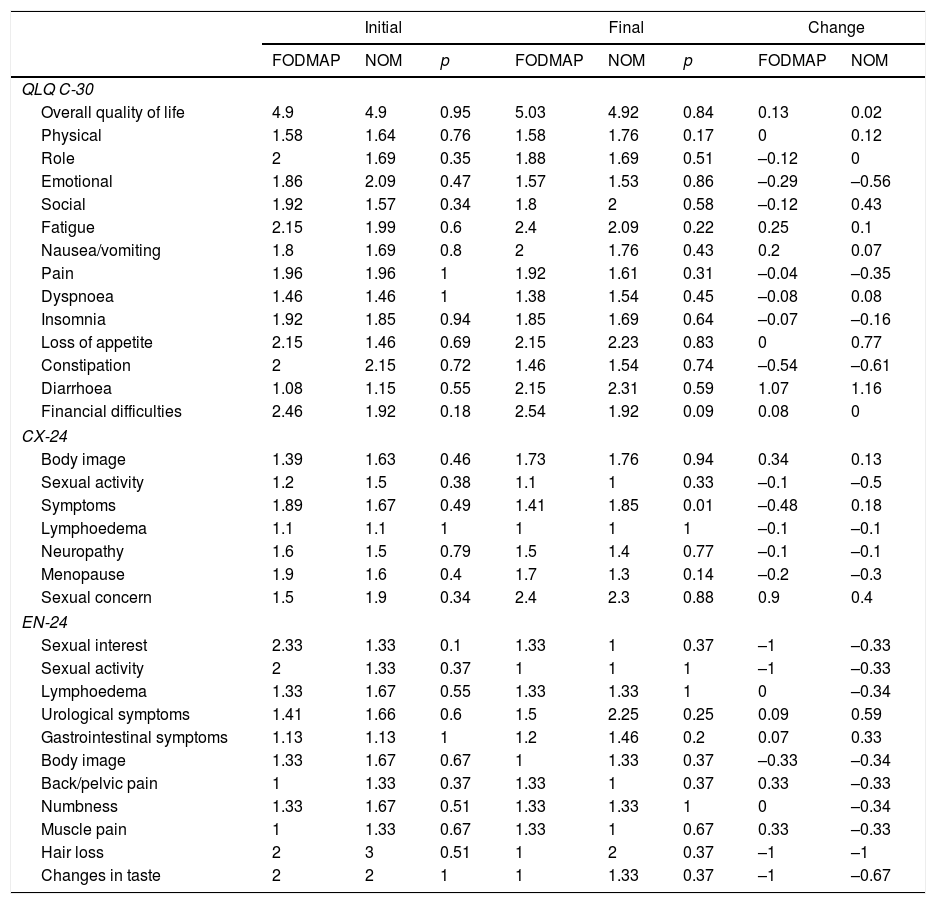
Quality of lifeThe averages of the initial and final scores on the EORTC QLQ C-30 general quality of life test and the EN-24 specific test for endometrial cancer had no significant differences. However, in the specific test for cervical cancer, a significant difference was observed in the symptoms section in the final questionnaire for patients assigned to the low FODMAP diet (Table 6).
Average initial and final quality of life scores and changes in scores.
| Initial | Final | Change | ||||||
|---|---|---|---|---|---|---|---|---|
| FODMAP | NOM | p | FODMAP | NOM | p | FODMAP | NOM | |
| QLQ C-30 | ||||||||
| Overall quality of life | 4.9 | 4.9 | 0.95 | 5.03 | 4.92 | 0.84 | 0.13 | 0.02 |
| Physical | 1.58 | 1.64 | 0.76 | 1.58 | 1.76 | 0.17 | 0 | 0.12 |
| Role | 2 | 1.69 | 0.35 | 1.88 | 1.69 | 0.51 | –0.12 | 0 |
| Emotional | 1.86 | 2.09 | 0.47 | 1.57 | 1.53 | 0.86 | –0.29 | –0.56 |
| Social | 1.92 | 1.57 | 0.34 | 1.8 | 2 | 0.58 | –0.12 | 0.43 |
| Fatigue | 2.15 | 1.99 | 0.6 | 2.4 | 2.09 | 0.22 | 0.25 | 0.1 |
| Nausea/vomiting | 1.8 | 1.69 | 0.8 | 2 | 1.76 | 0.43 | 0.2 | 0.07 |
| Pain | 1.96 | 1.96 | 1 | 1.92 | 1.61 | 0.31 | –0.04 | –0.35 |
| Dyspnoea | 1.46 | 1.46 | 1 | 1.38 | 1.54 | 0.45 | –0.08 | 0.08 |
| Insomnia | 1.92 | 1.85 | 0.94 | 1.85 | 1.69 | 0.64 | –0.07 | –0.16 |
| Loss of appetite | 2.15 | 1.46 | 0.69 | 2.15 | 2.23 | 0.83 | 0 | 0.77 |
| Constipation | 2 | 2.15 | 0.72 | 1.46 | 1.54 | 0.74 | –0.54 | –0.61 |
| Diarrhoea | 1.08 | 1.15 | 0.55 | 2.15 | 2.31 | 0.59 | 1.07 | 1.16 |
| Financial difficulties | 2.46 | 1.92 | 0.18 | 2.54 | 1.92 | 0.09 | 0.08 | 0 |
| CX-24 | ||||||||
| Body image | 1.39 | 1.63 | 0.46 | 1.73 | 1.76 | 0.94 | 0.34 | 0.13 |
| Sexual activity | 1.2 | 1.5 | 0.38 | 1.1 | 1 | 0.33 | –0.1 | –0.5 |
| Symptoms | 1.89 | 1.67 | 0.49 | 1.41 | 1.85 | 0.01 | –0.48 | 0.18 |
| Lymphoedema | 1.1 | 1.1 | 1 | 1 | 1 | 1 | –0.1 | –0.1 |
| Neuropathy | 1.6 | 1.5 | 0.79 | 1.5 | 1.4 | 0.77 | –0.1 | –0.1 |
| Menopause | 1.9 | 1.6 | 0.4 | 1.7 | 1.3 | 0.14 | –0.2 | –0.3 |
| Sexual concern | 1.5 | 1.9 | 0.34 | 2.4 | 2.3 | 0.88 | 0.9 | 0.4 |
| EN-24 | ||||||||
| Sexual interest | 2.33 | 1.33 | 0.1 | 1.33 | 1 | 0.37 | –1 | –0.33 |
| Sexual activity | 2 | 1.33 | 0.37 | 1 | 1 | 1 | –1 | –0.33 |
| Lymphoedema | 1.33 | 1.67 | 0.55 | 1.33 | 1.33 | 1 | 0 | –0.34 |
| Urological symptoms | 1.41 | 1.66 | 0.6 | 1.5 | 2.25 | 0.25 | 0.09 | 0.59 |
| Gastrointestinal symptoms | 1.13 | 1.13 | 1 | 1.2 | 1.46 | 0.2 | 0.07 | 0.33 |
| Body image | 1.33 | 1.67 | 0.67 | 1 | 1.33 | 0.37 | –0.33 | –0.34 |
| Back/pelvic pain | 1 | 1.33 | 0.37 | 1.33 | 1 | 0.37 | 0.33 | –0.33 |
| Numbness | 1.33 | 1.67 | 0.51 | 1.33 | 1.33 | 1 | 0 | –0.34 |
| Muscle pain | 1 | 1.33 | 0.67 | 1.33 | 1 | 0.67 | 0.33 | –0.33 |
| Hair loss | 2 | 3 | 0.51 | 1 | 2 | 0.37 | –1 | –1 |
| Changes in taste | 2 | 2 | 1 | 1 | 1.33 | 0.37 | –1 | –0.67 |
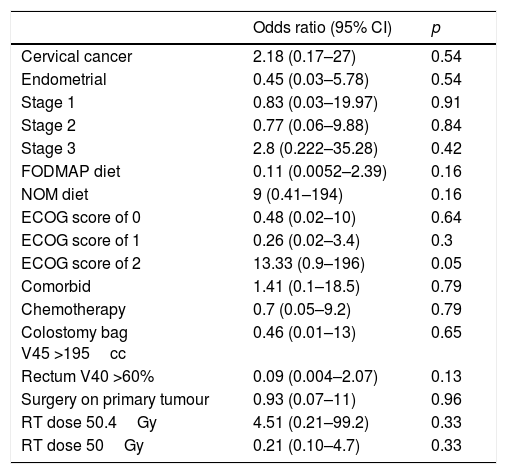
The univariate analysis of factors predictive of grade 3 gastrointestinal toxicity found no factors with a significant association, with an odds ratio of 9 (0.41–194, p=0.16) for the NOM diet and 0.11 (0.0052–2.39, p=0.16) for the low FODMAP diet (Table 7).
Univariate analysis of factors predictive of grade 3 gastrointestinal toxicity.
| Odds ratio (95% CI) | p | |
|---|---|---|
| Cervical cancer | 2.18 (0.17–27) | 0.54 |
| Endometrial | 0.45 (0.03–5.78) | 0.54 |
| Stage 1 | 0.83 (0.03–19.97) | 0.91 |
| Stage 2 | 0.77 (0.06–9.88) | 0.84 |
| Stage 3 | 2.8 (0.222–35.28) | 0.42 |
| FODMAP diet | 0.11 (0.0052–2.39) | 0.16 |
| NOM diet | 9 (0.41–194) | 0.16 |
| ECOG score of 0 | 0.48 (0.02–10) | 0.64 |
| ECOG score of 1 | 0.26 (0.02–3.4) | 0.3 |
| ECOG score of 2 | 13.33 (0.9–196) | 0.05 |
| Comorbid | 1.41 (0.1–18.5) | 0.79 |
| Chemotherapy | 0.7 (0.05–9.2) | 0.79 |
| Colostomy bag V45 >195cc | 0.46 (0.01–13) | 0.65 |
| Rectum V40 >60% | 0.09 (0.004–2.07) | 0.13 |
| Surgery on primary tumour | 0.93 (0.07–11) | 0.96 |
| RT dose 50.4Gy | 4.51 (0.21–99.2) | 0.33 |
| RT dose 50Gy | 0.21 (0.10–4.7) | 0.33 |
The incidence of gastrointestinal toxicity in patients treated with pelvic teletherapy was previously reported as 70–90% in grades 1–2, and 3–9% in grades 3 and 4. Our study found a similar incidence of grade 1 and 2 toxicity—77% and 85% for the low FODMAP diet group and the NOM group, respectively—with no significant difference between the two groups.
The incidence of grade 3 gastrointestinal toxicity was lower than that reported in the literature in the low FODMAP diet group and higher in the NOM diet group; 3 events occurred, corresponding to 11% of all patients and 23% of patients in this group. A likely explanation for the high incidence of grade 3 toxicity in the NOM diet group is the sample size.
The main gastrointestinal signs and symptoms presented by patients were nausea, vomiting and diarrhoea. All had a higher incidence in the NOM diet group, with no significant difference.
The greater incidence of gastrointestinal symptoms in the NOM diet group was accompanied by greater average weight loss in these patients (2.43kg vs 3.12kg) and a greater average decline in performance status based on ECOG score at the end of treatment (0.61 SD 0.5 vs 0.23 SD 0.43). This difference was statistically significant (p 0.049). Patients with cervical cancer assigned to this group had more symptoms at the end of treatment according to the CX-24 specific quality of life questionnaire compared to patients who underwent nutritional intervention with the low FODMAP diet (1.41 vs 1.85, p 0.01). No differences in other aspects of quality of life were observed.
For this reason, although no statistically significant decrease in gastrointestinal toxicity was achieved with the low FODMAP diet, the severity of gastrointestinal toxicity was lower in this patient group, and was accompanied by superiority in some aspects of quality of life in patients with cervical cancer, as well as lower functional decline at the end of treatment.
Moreover, the high rate of excellent adherence to the low FODMAP diet (85%) places it as a tool that may be used alone or in combination with other measures taken to decrease gastrointestinal toxicity. Furthermore, it may be implemented at any centre, as it does not require any specific resources or infrastructure.
ConclusionIn conclusion, implementing a low FODMAP diet during treatment with pelvic teletherapy is a low-cost, high-adherence measure that decreases the decline in performance status and symptoms at the end of treatment in patients with cervical cancer. Long-term patient follow-up must be performed to evaluate its impact on chronic toxicity, and a study on a larger number of patients designed to decrease severe toxicity during teletherapy (grade 3–4) must be conducted to determine its role in this scenario.
FundingNo external funding was received to prepare this article.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestAll authors declare that they have no conflicts of interest.