As life expectancy increases worldwide, so does the incidence of age-related pathologies, among them onychomycosis (OM). This fungal infection of the nails may represent a potential risk of complications among elderly due to the presence of concomitant diseases that can complicate their treatment.
ObjectiveTo determine the frequency of onychomycosis among elderly patients over a period of 2 years at the General Hospital of Mexico “Dr Eduardo Liceaga”.
MethodsRetrospective, observational, descriptive study.
ResultsA total of 138 patients were diagnosed with onychomycosis. Of these, 43 (31.2%) reported no concomitant diseases. The most common comorbidities in the remaining patients was arterial hypertension in 50 patients (36.2%) and diabetes mellitus in 49 (35.5%); the most common clinical type of OM was total dystrophic (87 patients, 63%), with involvement of the hallux of both feet (48 patients, 34.8%). The average evolution was 12 years; 60 patients (42.3%) denied previous treatments, and 32 (22.5%) used OTC medicines. In 125 patients (90.6%), filaments, yeasts or arthroconidia were observed. On culture examination, Candida yeasts (24 patients, 46.2%), followed by Trichophyton rubrum (21 patients, 40.4%) were identified.
ConclusionsApproximately 9 out of 10 nail disorders in the elderly were onychomycosis; many of these patients may present with comorbidities such as hypertension or diabetes mellitus, which often complicate treatment outcomes, affecting quality of life. Elderly patients should receive adequate health education and monitoring. This will improve their quality of life.
La perspectiva de aumento en el tiempo de vida del ser humano en la actualidad permite que diversas enfermedades aumenten su frecuencia, de éstas las alteraciones en la lámina ungueal, principalmente las onicomicosis pueden representar un riesgo en los adultos mayores debido a las patologías concomitantes que pueden complicar su tratamiento.
ObjetivoPresentar un panorama actual de onicomicosis en pacientes adultos mayores de los casos atendidos en un periodo de 2 años en el Hospital General de México “Dr. Eduardo Liceaga”, durante la realización de las “Ferias de la salud”.
MétodosEstudio retrospectivo, observacional, descriptivo.
ResultadosDel total de pacientes adultos mayores revisados, en 138 se comprobó el diagnóstico de onicomicosis, de los cuales 43 (31.2%) no refirieron ninguna otra enfermedad y las principales comorbilidades presentes en los demás fueron hipertensión arterial 50 (36.2%) y diabetes mellitus 49 (35.5%), la variedad clínica más frecuente fue la onicomicosis distrófica total 87 (63%), con afección de la primera uña de ambos pies 48 (34.8%), el promedio de evolución fue de 12 años; respecto a los tratamientos utilizados la mayoría 60 (42.3%), negaba haber utilizado alguno, y en menor proporción se refería el uso de productos de venta libre 32 (22.5%). En los resultados de los estudios micológicos 125 (90.6%) se observaron filamentos, levaduras o artroconidios, los hongos identificados fueron levaduras de Candida. 24 (46.2%), seguidos de Trichophyton rubrum 21 (40.4%)
ConclusionesAproximadamente, 9/10 alteraciones ungueales en el adulto mayor son onicomicosis, muchos de éstos pueden presentar comorbilidades como hipertensión arterial o bien diabetes mellitus, lo cual dificulta el manejo terapéutico, el deterioro en la calidad de vida y el vivir más años suelen estar acompañados, es necesario educar a la población y una vigilancia médica más estricta, ello mejorará la calidad de vida de nuestra población en edades avanzadas.
The World Health Organization (WHO) classifies individuals in the 60–74 age range as elderly, in the 75–90 age range as old, and those aged over 90 as very old. All individuals over the age of 60 are considered elderly.1
As life expectancy increases worldwide, so does the number of age-related pathologies, including skin disease. Of these, onychodystrophy is the third most common condition seen by doctors, and among these nail disorders, onychomycosis can be fairly common.2,3
Onychomycosis is usually caused by dermatophytes, yeasts of the Candida genus, and some non-dermatophyte moulds. The clinical characteristics of this pathology include colour changes, peeling, thickening of the nail plate, and even onycholysis. However, changes may also be purely morphological in nature, and are not always associated with a fungal infection.4,5
Elderly patients often present with nail abnormalities associated with factors such as ageing, life-style and habits, or with diseases such as diabetes mellitus, in which incidence of onychomycosis is estimated at 13%.3
In the absence of a reliable diagnosis of onychomycosis, changes in the appearance of the nail plate are often incorrectly treated, or prompt patients to self-medicate. This leads to therapeutic failure and can even result in serious complications caused by interactions between drugs used to treat the nail condition and other concurrent medication taken by the patient for other diseases, for example the interaction between itraconazole or fluconazole and oral antidiabetic drugs.
Our aim in this study is to analyse cases of onychomycosis diagnosed in elderly individuals attending the ferias de salud, or outdoor health awareness-raising activities organised by the Dr. Eduardo Liceaga General Hospital of Mexico in 2013 and 2014. The cases discussed here will give an overview of the current status of this disease in the elderly population of Mexico.
Materials and methodsA total of 347 elderly patients were seen over a period of 2 years. During this time, 217 signs and symptoms of onychomycosis were detected, and details such as age, sex, concomitant diseases, clinical form of the nail disorder, evolution, and prior treatment were noted.
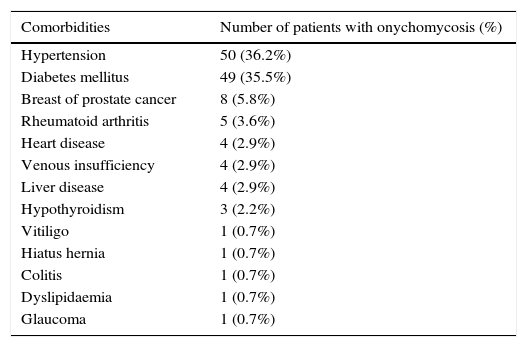
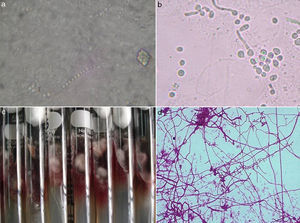
Patients verbally consented to doctors taking a scraping of affected nail plate for a KOH (10% potassium hydroxide) test. Samples were cultured using Sabouraud dextrose agar (SDA) alone or in combination with antibiotics (Micobiótico®) to isolate and identify the aetiological agents of the infection. Yeasts were identified by the specific production of pigments in colonies grown on CHROMagar Candida®, by isolation in cultures grown on corn meal agar with the addition of 1% Tween 80, and by their biochemical profile obtained from the AUXACOLOR® yeast identification system. Filamentous fungi isolates were identified by means of a morphological analysis of the culture obtained and microscopic observation.
Statistical analysisThe data collected were analysed descriptively using measures of central tendency and scatter and presented in the form of tables.
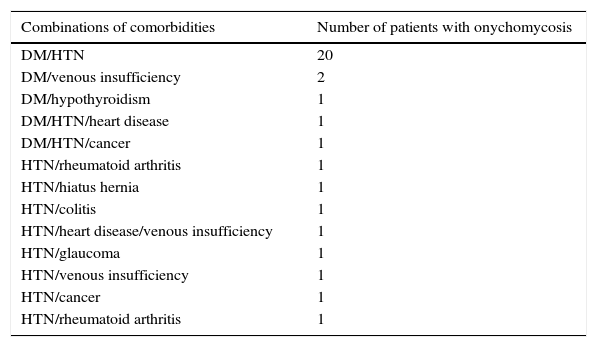
ResultsA total of 347 patients aged 60 years or over attended the 4 ferias de salud organised by the Hospital General of Mexico between 2013 and 2014. The average age was 67.9 years; 256 (74%) were women and 91 (26%) men. During check-ups, doctors detected 217 (63.3%) cases of suspected onychomycosis in 157 women (72.3%) and 60 men (27.7%). Fungal infection was confirmed in 138 of these cases: 88 (63.8%) women and 50 (36.2%) men. Of these, 43 (31.2%) patients denied concomitant disease. The comorbidities associated with this patient group are shown in Table 1, while Table 2 lists specific comorbid combinations.
Comorbidities in patients with onychomycosis.
| Comorbidities | Number of patients with onychomycosis (%) |
|---|---|
| Hypertension | 50 (36.2%) |
| Diabetes mellitus | 49 (35.5%) |
| Breast of prostate cancer | 8 (5.8%) |
| Rheumatoid arthritis | 5 (3.6%) |
| Heart disease | 4 (2.9%) |
| Venous insufficiency | 4 (2.9%) |
| Liver disease | 4 (2.9%) |
| Hypothyroidism | 3 (2.2%) |
| Vitiligo | 1 (0.7%) |
| Hiatus hernia | 1 (0.7%) |
| Colitis | 1 (0.7%) |
| Dyslipidaemia | 1 (0.7%) |
| Glaucoma | 1 (0.7%) |
Combinations of comorbidities in patients with onychomycosis.
| Combinations of comorbidities | Number of patients with onychomycosis |
|---|---|
| DM/HTN | 20 |
| DM/venous insufficiency | 2 |
| DM/hypothyroidism | 1 |
| DM/HTN/heart disease | 1 |
| DM/HTN/cancer | 1 |
| HTN/rheumatoid arthritis | 1 |
| HTN/hiatus hernia | 1 |
| HTN/colitis | 1 |
| HTN/heart disease/venous insufficiency | 1 |
| HTN/glaucoma | 1 |
| HTN/venous insufficiency | 1 |
| HTN/cancer | 1 |
| HTN/rheumatoid arthritis | 1 |
The most common clinical form of the disease was total dystrophic onychomycosis (TDO) in 87 patients (63%), followed by distal subungual onychomycosis (DSO) in 37 (26.9%). Other subtypes found were lateral subungual onychomycosis (LSO) in 4 patients (2.9%), distal onychomycosis in 4 (2.9%), superficial leuconychia in 4 (2.9%), yellow nails in 1 patient (0.7%), and 1 (0.7%) case of DSO and TDO involving several nails. The most common site of infection was the hallux of both feet in 48 patients (34.8%), followed by involvement of several nails on both feet in 46 patients (33.3%). In the remaining patients, infection was limited to the hallux of the left foot, in 23 (16.7%) or of the right foot, in 21 (15.2%) (Fig. 1).
The evolution of the disorder varied greatly, with patients reporting symptoms lasting from 1 month to 37 years. Mean evolution was 12 years.
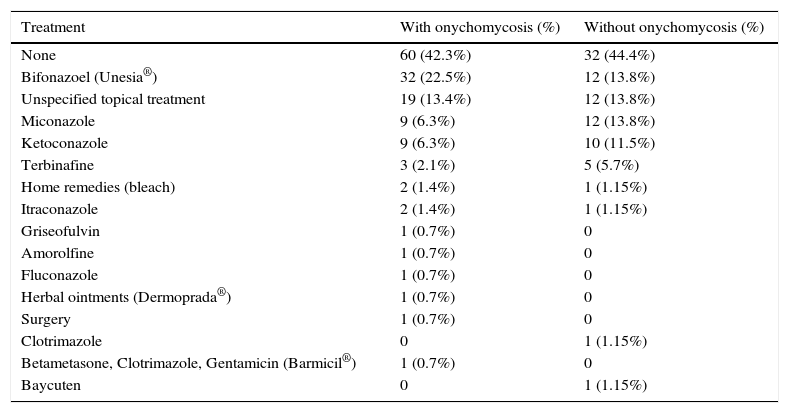
The treatment administered in each case is shown in Table 3.
Therapy prior to onychopathy.
| Treatment | With onychomycosis (%) | Without onychomycosis (%) |
|---|---|---|
| None | 60 (42.3%) | 32 (44.4%) |
| Bifonazoel (Unesia®) | 32 (22.5%) | 12 (13.8%) |
| Unspecified topical treatment | 19 (13.4%) | 12 (13.8%) |
| Miconazole | 9 (6.3%) | 12 (13.8%) |
| Ketoconazole | 9 (6.3%) | 10 (11.5%) |
| Terbinafine | 3 (2.1%) | 5 (5.7%) |
| Home remedies (bleach) | 2 (1.4%) | 1 (1.15%) |
| Itraconazole | 2 (1.4%) | 1 (1.15%) |
| Griseofulvin | 1 (0.7%) | 0 |
| Amorolfine | 1 (0.7%) | 0 |
| Fluconazole | 1 (0.7%) | 0 |
| Herbal ointments (Dermoprada®) | 1 (0.7%) | 0 |
| Surgery | 1 (0.7%) | 0 |
| Clotrimazole | 0 | 1 (1.15%) |
| Betametasone, Clotrimazole, Gentamicin (Barmicil®) | 1 (0.7%) | 0 |
| Baycuten | 0 | 1 (1.15%) |
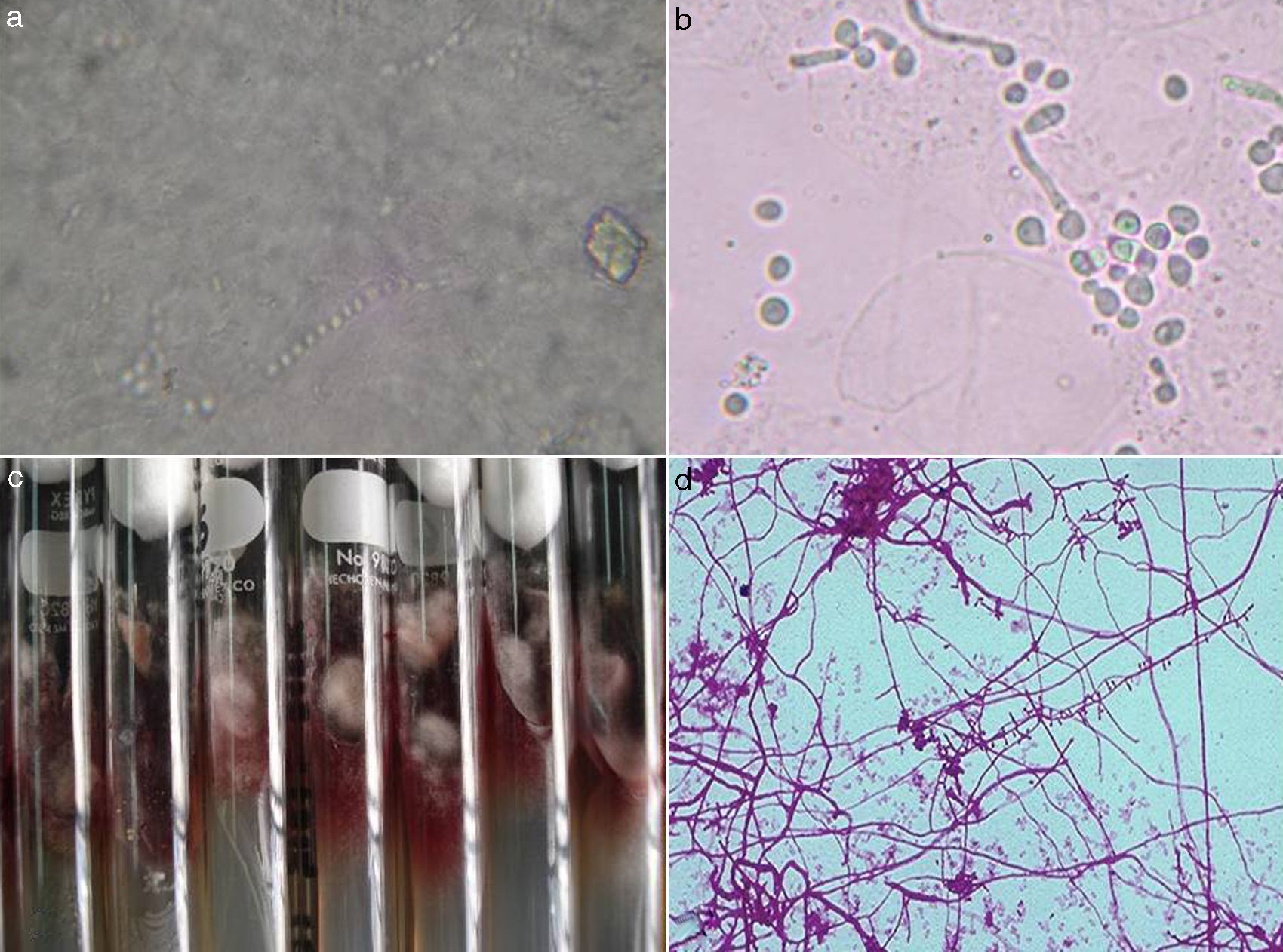
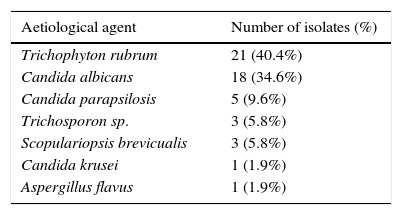
Filamentous fungi, yeasts or arthroconidia were identified in 125 (90.6%) studies. In 13 cases (9.4%), no structure was visible on microscopic examination, although a fungus associated with onychomycosis was isolated. In the case of cultures, in 51 (36.9%) a type of fungus associated with mycosis was isolated, and in 87 (63.1%) no fungi were grown. The aetiological agents are shown in Table 4. In one particular culture, both Trichophyton rubrum and Candida albicans were isolated (Fig. 2).
Aetiological agents isolated in patients with onychomycosis.
| Aetiological agent | Number of isolates (%) |
|---|---|
| Trichophyton rubrum | 21 (40.4%) |
| Candida albicans | 18 (34.6%) |
| Candida parapsilosis | 5 (9.6%) |
| Trichosporon sp. | 3 (5.8%) |
| Scopulariopsis brevicualis | 3 (5.8%) |
| Candida krusei | 1 (1.9%) |
| Aspergillus flavus | 1 (1.9%) |
Increased life expectancy in recent decades has led to population ageing6 and an increased prevalence of chronic and degenerative diseases that predispose elderly patients to comorbid conditions requiring different treatment. Nail disorders are among the many different conditions found in this population, and can develop into a serious health problem if diagnosed incorrectly, or not at all. Incorrect diagnosis will lead to therapeutic failure, and the treatment prescribed for fungal infections can interact with the drugs administered to treat the patient's comorbidities, causing complications or adverse events that can worsen these conditions.
In this study, we observed a clear preponderance of women over men (3:1 approximately). This could be due to selection bias, since participation in the ferias de salud organised by the General Hospital of Mexico is voluntary and patients are not randomised. As a result, we have observed that women show a greater interest seeking a diagnosis for ungual pathology than men, who either refuse the examination, or do not attend the feria. Of the total number of patients examined, 347 were elderly (aged 60 years or older), of whom 157 (45.2%) presented with ungual abnormalities consistent with onychomycosis. Diagnosis was confirmed in 138 (87.9%) cases. This suggests that diagnosis is confirmed in 9 out of every 10 elderly patients presenting with symptoms consistent with onychomycosis, a conclusion that is consistent with the findings of other studies.2,3,6–8
Most patients had no concomitant disease (31.2%). In those that did, hypertension (36.2%), diabetes mellitus (35.5%) and concurrent hypertension and diabetes (14.5%) were the most common. This finding is very similar to the results of a survey on onychomycosis in Mexico,9 in which diabetes mellitus (21%) and hypertension (16%) were the most common comorbidities among 12,637 patients from various cities in Mexico. This is an important factor in the choice of oral antifungal medication, due to the risk of interaction with the patient's regular medication: triazoles such as fluconazole and itraconazole, for example, cause more drug interactions than terbinafine. These interactions can include inhibition of the CYP3A4 enzyme, because several drugs, such as the latest antihistamines, HMG-CoA reductase inhibitors, and some benzodiazepines, are substrates for CYP3A. In other cases, co-administration with ciclosporin or quinidine should be monitored.7–10
Sixty patients (42.3%), denied taking any kind of medication or treatment for onychomycosis, 32 patients (22.5%) used over the counter products, and the 50 remaining patients (35.2%) used a variety of topical and/or systemic antifungal preparations alone or in combination with topical steroids. In these cases, they reported poor adherence due to forgetfulness or ignorance of which regimen they had been prescribed. This is an important factor in this patient population, who are often frail and depend to a greater or lesser extent on carers to perform their activities of daily living, including the administration of topical or system medication. Other authors have also drawn attention to this situation, suggesting that the social relationships of elderly patients are affected by their dependency, which greatly limits their independence, causing depression and undermining their quality of life.11,12
In these circumstances, it is understandable that they depend on others for their healthcare and are unaware of important information such as the type or presentation of their prescribed medication. Other factors to be considered are the psychological changes that take place with advanced age. Therefore, the co-existence of one or more organic diseases with onychomycosis, which is common in this patient population, can pose a serious health risk due to potential drug interactions with oral therapy such as anti-diabetic or hypertensive drugs, while the side effects of these interactions can complicate the symptoms of the concomitant organic disease. According to the findings of this study, around 20% of elderly patients presenting onychomycosis have comorbidities, and therefore are at risk for these complications. Incorrect management of these patients can undermine their quality of life and worsen their existing health problems.13
With respect to the clinical form and topography of the disease, TDO (63%) affecting the hallux of both feet was the most common presentation (34.8%). This was followed by DSO (26.9%) affecting several nails on both feet (33.3%). In these cases, some patients presented two clinical forms of the disease, nearly always involving the TDO/DSO combination. In most patients aged between 60 and 70 years, the disease involved the nail of the hallux of both feet, while in the 70–80 age group it often affected several nails on both feet. This suggests that the ungual changes observed are not only due to intrinsic factors such as age-related sedentarism, poor circulation, or friction against footwear caused by walking habits,14,15 but that onychomycosis plays an important role in these changes. In other words, in most cases, during the transition from elderly to old, the fungi causing the condition tend to infect other nails.7,8
Microscopic examination of samples taken from 125 patients (90.6%) showed parasitic fungi. In 13 cases (9.4%), these structures were not microscopically visible but the fungi were isolated in cultures. Fifty-one (36.9%) patients presented some type of fungal development, the most common being Candida (C. abicans, C. parapsilosis and C. krusei) yeasts, followed by T. rubrum, and to a lesser extent Trichosporon sp., Scopulariopsis brevicaulis and Aspergillus flavus. The wide variety of yeasts found in these patients could be related to their concomitant diseases: studies have shown that diabetes mellitus and combination therapy administered for other diseases could predispose these individuals to fungal infections. Onycholysis and the humid environment created by closed footwear, meanwhile, have been associated with the presence of non-dermatophytic filamentous fungal infections.4,11,14
The incorrect use of topical or systemic antifungal medication could explain why in some samples the fungi were invisible under microscopic examination or could not be isolated in synthetic media. Many of the patients in this study reported using these preparations without medical prescription or adequate monitoring, which can lead to therapeutic failure and interfere with laboratory studies. In these cases, it is best to instruct the patient to discontinue the antifungal medication for a time, and then repeat the test.
The widely accepted therapy of choice for onychomycosis11,16 is itraconazole 200mg/day/3–4 months, fluconazole 150mg/week/4–12 months, or terbinafine 250mg/day/3–4 months. In some patients, a combination of topical and systemic medication is indicated, such as amorolfine 5%, tioconazole 28% and bifonazole 40%.11 The choice of therapy will depend on the aetiological agent and the clinical condition of the patient. It is important to ascertain whether the patient is taking other medication for concomitant diseases due to the possibility of drug interaction that can cause adverse events or synergic effects that can undermine the health of these patients.17–19
ConclusionsNail plate abnormalities are relatively common in elderly individuals, and in 9 out of 10 cases are due to onychomycosis. The number of affected nails tends to increase with age, while the presence of common comorbidities such as hypertension or diabetes mellitus can complicate the therapeutic management of these patients. It is important to avoid drug interactions and consider the potential side effects of anti-fungal drugs, which can undermine the quality of life of patients with many years left to live. For this reason, it is important to educate patients and monitor their progress more closely whenever required. Taken together, these measures will help improve the quality of life of the elderly population of Mexico.
Conflict of interestThe authors declare that they have no conflict of interests.