Los carcinomas endobronquiales atípicos tienen peor pronóstico que los típicos; el mejor tratamiento es la resección quirúrgica dependiendo del área afectada. Presentamos un caso de paciente masculino de 47 años de edad, con un índice tabáquico de 9 y dislipidemia, acudió al Servicio con antecedentes de fiebre intermitente, tos con expectoración hialina, dolor escapular izquierdo y pérdida de peso de 5 Kg en los últimos seis meses. En los estudios de imagen se observó un tumor endobronquial en bronquio principal izquierdo a menos de 2 cm de la carina, ocluyendo el 100% del lumen; se realizó neumonectomía con posterior colocación de colgajo de tejido adiposo pericárdico al muñón bronquial. El paciente continúa con una evolución adecuada y sin evidencia de recurrencia. Las guías de la National Comprehensive Cancer Network sugieren realizar re-resección, sin embargo, en un caso como el nuestro, se debe reconsiderar para un abordaje conservador.
Atypical endobronchial carcinomas have a worst prognosis than the typical subtype; the best treatment is total surgical resection depending on the affected area. We present a 47-year-old male with a tobacco index of 9 and dyslipidemia, with a history of intermittent fever, cough with hyaline sputum, left scapular pain and 5 Kg weight loss in the past six months. Imaging studies revealed an endobronchial tumor in left main bronchi at less than 2 cm from the carina occluding 100% of its lumen; a pneumonectomy was performed with a pericardial adipose tissue flap placed on the bronchial stump. Pathology reported an R1 resection. Patient continues with adequate evolution and without macroscopic evidence of recurrence. National Comprehensive Cancer Network (NCCN) guidelines suggest a redo-surgery, nevertheless in a case as ours; consideration has to be made for a conservative approach.
• Introduction
Neuroendocrine neoplasms with predominant neuroendocrine differentiation, arise in most organs of the body.1,2 The lung is one of the most affected sites, classification is as follows; neuroendocrine carcinoma (NC) grade 1 allocated as low grade, NC grade 2 as intermediate grade and NC grade 3 as high grade, with its subtypes, small cell carcinoma and large cell NC.3 Well-differentiated NCs have been variably termed carcinoid tumor, neuroendocrine tumor or NC. Also functioning NCs are defined based on their clinical symptoms due to excess hormone secretion, however not all carcinoid tumors have a carcinoid syndrome associated4 NC of the lung present a spectrum of differentiation, from typical carcinoid tumors to small-cell NC. Intermediate degrees of differentiation and behavior define other neoplasms in this spectrum, atypical carcinoid tumors and large cell NC.5 Engelbreth-Holm first described a difference between typical and atypical carcinomas,6 later defined with histologic criteria by Arrigoni et al.7
Classified by the World Health Organization 1982 and amended various times.8 Treatment protocols also are in constant evolution and attention must be taken to adequately manage these patients. We present a case of successful pneumonectomy due to an atypical carcinoid endobronchial tumor, however, the surgical team underwent through management hardships in the postoperative period.
• Case presentation
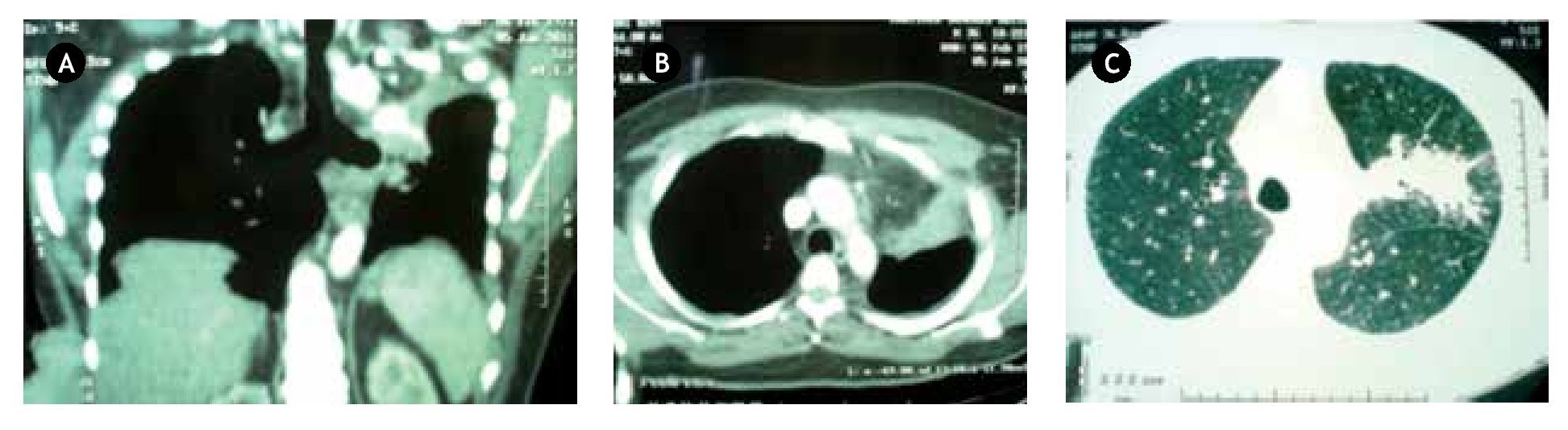
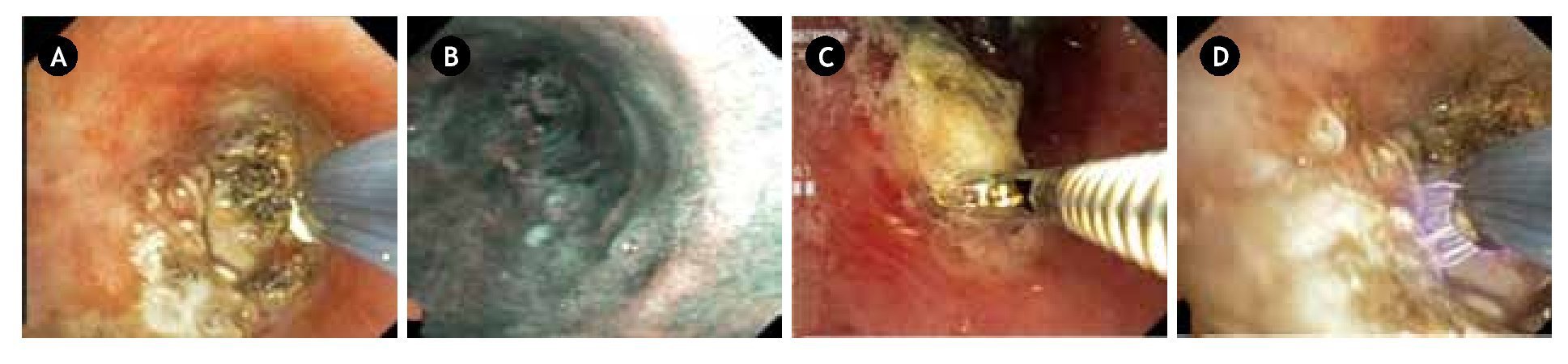
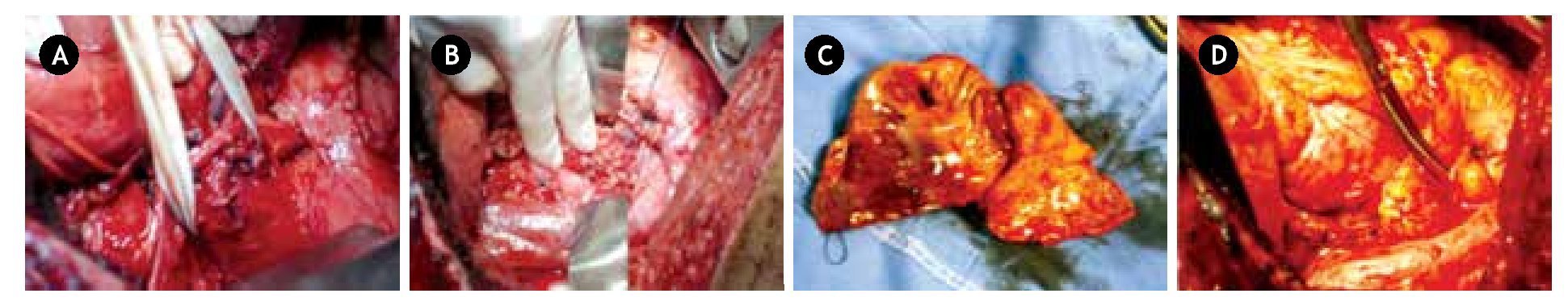
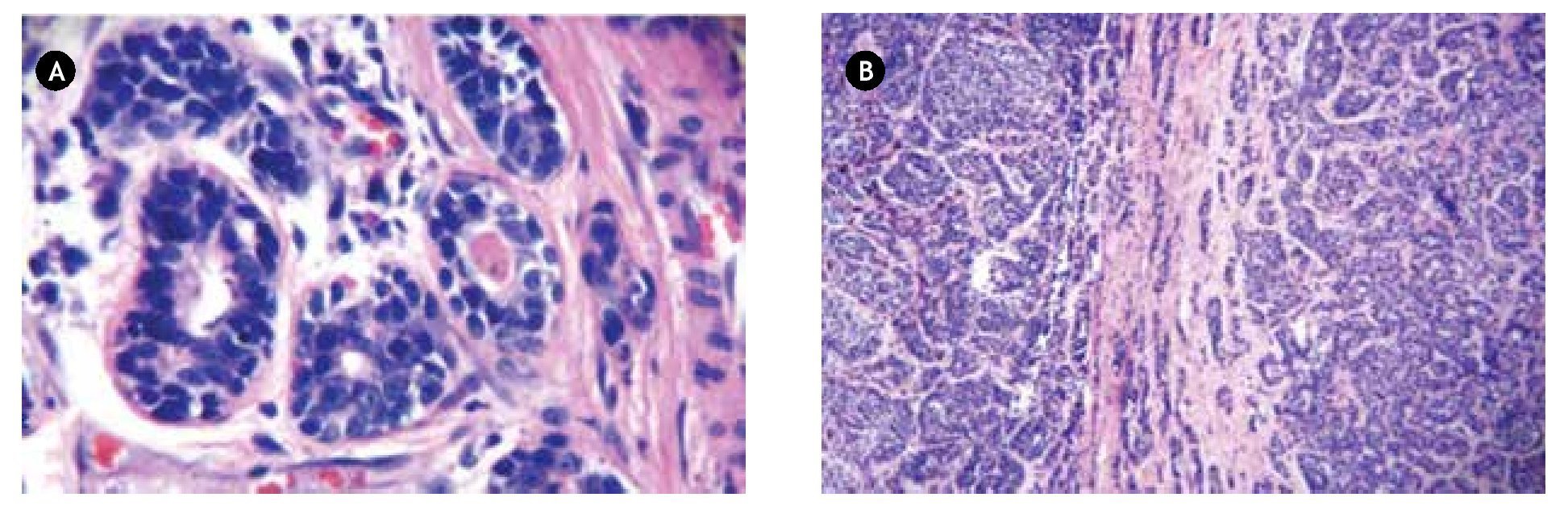
A 47-year-old male with a tobacco index of 9 and dyslipidemia, with a history of intermittent fever, cough with hyaline sputum, left scapular pain and 5 Kg weight loss in the past six months with diminished breath sounds in left thorax was admitted to our Service. Computed tomography revealed an image suggestive of an endobronchial tumor in left main bronchi with secondary atelectasis of the upper left lobe (Figure 1), bronchoscopy corroborated the diagnosis reporting a left main bronchus with a multinodular endobronchial tumor < 2 cm from the carina that occluded 100% of the lumen, narrow band imaging (NBI) with a dense vascular network, a biopsy reported carcinoid tumor and finally argon plasma was utilized in an attempt to permeabilize its lumen (Figure 2). A pneumonectomy was performed with a pericardial adipose tissue flap placed on the bronchial stump (Figure 3); transferred to the Respiratory Intensive Care Unit for resuscitation and a multidisciplinary rehabilitation program; a left clamped chest tube was left in place for posterior pleural fluid observation, once a serious drainage was confirmed 48 hours after surgery, the tube was removed. During the pathology review the complete airway occlusion was evident as to the presence of bronchiectasis and macroscopic N12 node invasion; immunochemistry tested positive for chromogranine, neuronal enolase, CKAE1 and CKAE3; pathology reported an atypical carcinoid tumor with R1 resection (Figure 4), positive N12 and negative N5, N6, N7, N9 and N10 nodes; thus staging the patient as IIIA. He continued treatment in the Oncology Department for adjuvant radiotherapy only, awaiting bronchoscopy control biopsy results, six months later, these were performed with the aid of NBI and were negative at the bronchial stump, also with thoracic tomographic studies that confirm absence of relapse and thus chemotherapy was not added to the therapeutical regimen, patient continues after two years in the Outpatient Cardiothoracic Clinic in adequate control and without recurrence.
Figure 1. Computed tomography of the chest in a A) coronal reconstruction demonstrating near total obstruction of the left main bronchial lumen. B) Axial mediastinal and C) pulmonary windows demonstrating the secondary athelectasis produced by the tumor.
Figure 2.A) Bronchoscopic view of the tumor, B) Narrow band imaging demonstrating the vascular bed of the bronchial lumen. C) During the biopsy and D) the use of argon plasma to permeabilize the airway.
Figure 3.A) During surgery the hilum is referred, B) the main bronchus is sutured after retrieval of the specimen C); finally a patch of pericardial fat is used to cover the stump D).
Figure 4.A) Neoplastic organoid lesion with clusters of scarce cytoplasm cells, in a salt and pepper pattern with granular chromatin within a large nucleus, H&E 100x. B) Pleural and vascular invasion of clustered neoplastic cells of the same characteristics in the lymph nodes, H&E 40x.
• Discussion
Atypical carcinoid tumors of the lung are uncommon, representing less than 5% with the typical sub-type, of all lung tumors.9 There exists scarce literature on the atypical subtype. Echegoyen-Carmona and colleagues reported a 10 year experience with seven cases, the largest series in Mexican literature.10 Our group has encountered these sporadic cases also without recurrence in both of them.11,12
In accordance with other authors, bronchogenic carcinoid is rarely associated to a carcinoid syndrome, present in only 5% of the cases.13 Our patient was diagnosed for other reasons, such as airway obstruction; the decision was made to pearmibilize the airway with argon plasma during the preoperative period; once the diagnosis of atypical carcinoma was made, a left pneumonectomy with adequate postoperative evolution guided our judgment weather to perform a redo-resection or continue in a conservative manner with radiotherapy. According to the International Society for the Study of Lung Cancer, residual tumor classification can be divided in: a) R0 for macroscopic and microscopic free margins, b) R1 for macroscopic free margins but microscopic persistence of tumor cells, and c) R2 for macroscopic persistence of tumor.14 From the histologic perspective atypical carcinoid tumors are characterized by high mitotic activity, nuclear atypia, 2 to 10 mytosis/mm3 or necrosis.15 Maroun et al. considers that surgical resection should always be considered when technically and clinically appropriate to accomplish cure, detumorization, and palliation of symptoms,16,17 while NCCN guidelines suggest a redo-resection in the case of a R1 pathology result , after analyzing the evidence, conflict aroused within our group weather to re-operate the patient with all the imminent risks vs. following closely his evolution through adjuvant treatment, control biopsies with the aid of bronchoscopy which resulted negative eased our concerns.
The reported survival at five years for atypical carcinoid tumors in the stage described is 79%,18 taking this into account, a close follow up is necessary in borderline cases such as ours, definitely randomized trials should be done to clarify the surgeon´s conduct to weather re-operate or be expectant.
• Conflict of interest
The authors declare no conflict of interest.
• Funding
None.
Correspondence:
Walid Leonardo Dajer Fadel.
Av. Cuauhtémoc N° 403, Edificio 12,
Apartamento 102, Col. Roma Sur, Del.
Cuauhtémoc, C.P. 06760, Mexico City, Mexico.
Telephone: (55) 4192 0582.
Email address: wadafa@hotmail.com.