Las bulas enfisematosas gigantes representan una forma rara de destrucción de la enfermedad enfisematosa, generalmente debido a tabaquismo o deficiencia de α-1-antitripsina; la presencia de esta patología es extremadamente rara en ausencia de dichos antecedentes. La indicación quirúrgica en estos casos se limita a sobreexpansión torácica, compromiso de la función pulmonar y evidencia de parénquima comprimido. Presentamos el caso de paciente femenino de 75 años de edad, sin antecedentes de tabaquismo y con α-1-antitripsina sérica normal, la cual desarrolló compromiso respiratorio, por lo que se le realizó una bulectomía para reducción pulmonar exitosa con consecuente mejora del estatus ventilatorio. Existen pocos reportes en la literatura de enfermedad bulosa gigante sin factores de riesgo previos, razón que estimuló nuestra presentación.
Giant emphysematous bullae represent a rare form of emphysematous lung destruction and occur usually due to smoking or α-1-antitrypsin deficiency; presence of this disease is extremely rare in absence of the aforementioned. Surgery is indicated when there is a chest over-expansion, pulmonary function compromise and evidence of a normal compressed lung. We present a 75-year-old female without a smoking history and normal serum α-1-antitrypsin who developed respiratory compromise, a successful bullectomy for lung reduction was performed, with consequent improvement of the ventilatory status. Few reports exist of giant bullous disease with no previous risk factors, reason that prompted our report.
• Introduction
Bullae may originate in a variety of clinical and pathogenic settings; the majority in smokers and α-1-antitrypsin deficiency patients, rarely, other causes are presented as the originators of this devastating disease. The pulmonary insult causes a decreased mass of functioning lung tissue and thus reduces the amount of gas exchange that can take place, as it progresses, elastic recoil is lost, with consequent volume expansion, leading to a hyperextended chest with flattened diaphragms, widened intercostal spaces, and horizontal ribs, culminating in decrease of the mechanical advantages of normal breathing and augmenting the breathing work and dyspnea.1 The scenario of a patient without these two preconditioning factors makes this report interesting; we could only find one reported case in the literature.2 The diagnostic work-up, surgical approach and post-operative evolution are discussed.
• Case presentation
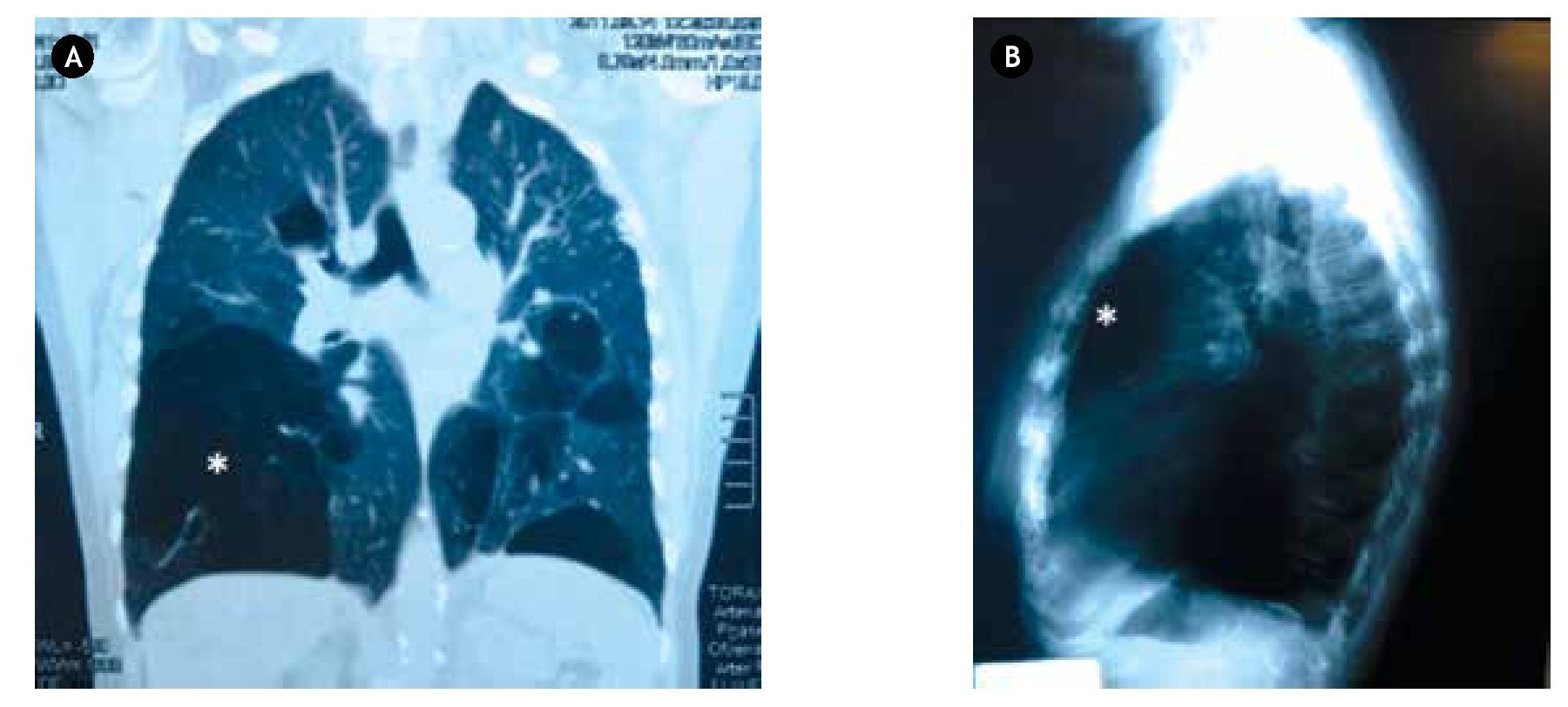
A 75-year-old non-smoker female, with a history of systemic arterial hypertension and biliary lithiasis, arrived at our department referred due to an incidental radiographic finding of an asymptomatic bullous disease five years before, which progressed to incapacitating dyspnea. A new simple control radiographic study was performed, suggesting the presence of right giant bullae with associated horizontalized and increased intercostal space distance that produced a mediastinal shift to the left. Computed tomography demonstrated giant bullae in the right middle lobe and other disseminated small ones in left lung parenchyma (Figure 1). Spirometry revealed a severe restrictive pattern, arterial gases with persistent hypoxemia of 82%, the forced expiratory volume in one second over vital capacity was 49.7%. A serum determination of α-1-antitrypsin resulted within the normal range.
Figure 1. A) Coronal reconstruction CT demonstrating the giant bullae (*) occupying > 50% of the right inferior thoracic cavity. B) Lateral chest X-ray showing an anterior hyper-clarity suggestive of the giant bullae.
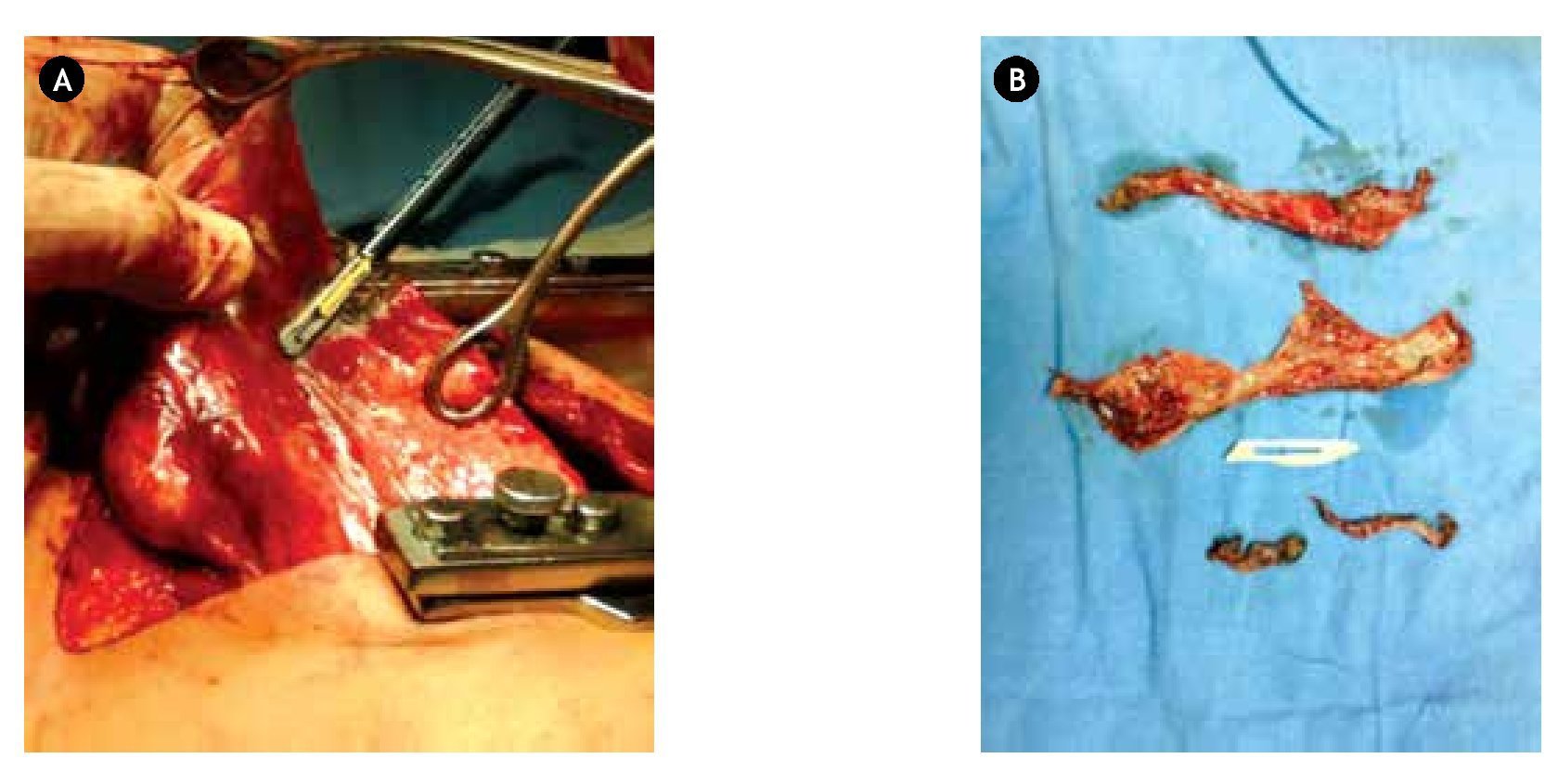
During a right muscle-sparing thoracotomy, type II giant bullae was observed; a resection of its wall was performed with an EnSeal® tissue-sealing device, leaving a 1 cm margin; the internal surface of the lesion was sutured together closing the pulmonary parenchyma with a continuous polyglycolic acid suture (Figure 2). Two chest tubes where left in place in the postero-apical and antero-apical positions, retrieved five days later due to a satisfactory progress. Histology reported panacinar emphysema. The patient´s symptoms markedly improved and she continues to while attending the Outpatient Clinic with good follow-up control 18 months after surgery.
Figure 2. A) Bullae resection leaving a 1 cm margin. B) Resected contracted tissue, approximately 1/4 smaller that it's in situ state.
• Discussion
Bilateral bullous emphysema (BBE) and heterogeneous diffuse emphysema are two forms of clinical presentation of this disease. The BBE which corresponds to our case, characterizes itself by inferior lobe compression and atelectasis when more than 50% of the lung volume is occupied, in our patient´s symptoms, the incapacitating dyspnea raised preoccupation due to the possibility of bullae rupture followed by tension pneumothorax, infection or abscess formation.3,4 The progressive course of the limiting pulmonary function, which is one of the absolute indications for surgery, was taken into account in the decision making process to perform the procedure. The two most important described predisposing factors to the formation of giant bullae are smoking and α-1-antitrypsin deficiency,5 both of which were discarded in the preoperative studies, reason that prompted our report, since up to this moment we still have not found a cause for the patient´s disease. Pharmacologic therapy has proven unhelpful to provide relief in these cases; nevertheless surgical treatment remains the same. Preoperatively, surgical complications were entertained as a possible reason not to perform the resection, fortunately, these never emerged. Work-up is of the outmost importance to adequately choose a good candidate for this technique, our patient met adequate criteria for this surgery, and a resection of the largest bullae could be done without complications.
The most common symptoms that lead to the selection of a patient for bullectomy are, as described before, dyspnea, pain and spontaneous pneumothorax; other are rare but include bleeding and infection within the bullae.
Conservative management of this disease could lead to enlargement of the bullae causing worsening dyspnea, but the lack of large series of patients treated without surgery makes prediction of expansion unreliable. Asymptomatic patients that present bullae that occupy more than one half of the pleural cavity should be considered good surgical candidates. Our patient had this feature added to the fact of worsening dyspnea.
Suggested surgical approaches are through a muscle-spar ing thoracotomy or v ideo-assisted thoracoscopy, depending on the transitional tissue´s clarity; small bullae with an adequate pedicle could be excised with a stapling device, which was not our case. The main complications in the perioperative period are prolonged air leak, atrial fibrillation, postoperative mechanical ventilation and pneumonia.6 Post-operative air-leak is the single most common complication encountered, present in 53% of patients; when these extend for more than seven days a corrective surgery should be considered, with the use of buttressed stapled lines, pleural tent, pleurectomy, biological glues or ambulatory Heimlich valves, which have reported mortality of 2.3%.7
In conclusion, preoperative evaluation is of the outmost importance in these cases, due to the clear perioperative risks encountered by a surgical approach; adequate evaluation weighting the benefits vs. the deleterious possible results should be made; with an experienced team of physicians that could respond accordingly in a facility with an important flow of respiratory disease patients.
• Conflict of interest
The authors declare no conflict of interest.
• Funding
None.
Correspondence:
Walid Leonardo Dajer Fadel.
Av. Cuauhtémoc N° 403, Edificio 12,
Apartamento 102, Col. Roma Sur, Del. Cuauhtémoc,
C.P. 06760, Mexico City, Mexico. Telephone: (52) 55 4192 0582.
E-mail: wadafa@hotmail.com