Chronic low back pain is the most common reason for seeking medical care for the musculoskeletal system. It is believed that 70–80% of people will experience low back pain at some point in their lives. It is a major cause of work absenteeism. Facet syndrome (FS) has been identified as a cause of chronic low back pain. Drug treatment combined with rehabilitation is often started. When significant pain relief is not achieved in a short period of time, a more selective, minimally invasive treatment, such as percutaneous lumbar facet radiofrequency (RF) thermocoagulation, can be chosen to achieve a more satisfactory outcome.
El dolor lumbar crónico constituye la causa más frecuente de consulta médica del aparato locomotor, se considera que el 70 a 80% de la población sufrirá dolor lumbar en algún momento de la vida. Es una causa importante de absentismo laboral. Como una causa del dolor lumbar crónico se identifico al síndrome facetario (SF). Frecuentemente, el tratamiento se inicia de manera farmacológica asociado a rehabilitación. Cuando no se obtiene un gran alivio del dolor a corto plazo, se puede optar por un tratamiento más selectivo, mínimamente invasivo, como es la termocoagulación percutánea facetaria lumbar por radiofrecuencia (RF), logrando un resultado más satisfactorio.
Low back pain is the most common reason for seeking medical care for a musculoskeletal disease in both the working and the non-working population. It is the most common cause of activity limitation in patients over 45 years of age, the third most common reason for surgery and the fifth most common cause of hospitalisation.1 Around 70–80% of people will experience low back pain, with the significant social, economic and occupational repercussions that it entails, at some point in their lives. Around 10–15% of cases of illness-related work absenteeism are directly related to low back pain. It accounts for 25% of retirements. Jobs that involve lifting weights and engaging in vigorous physical activity, factors traditionally identified as causes of back pain, have been steadily decreasing. However, the number of people who suffer from low back pain has not decreased.2
Schmörl and Junghanns introduced the concept of mobile lumbar segment in 1968 to refer to the junction between two lumbar vertebrae formed by the intervertebral disc, intervertebral ligaments, articular facets and muscles of the lumbar spine.3 Therefore, low back pain may arise from several structures such as the discs, ligaments, musculature and sacroiliac joints and from articular facet degeneration. In 1911, Goldwaith postulated that the “peculiarities of the facet joints” are responsible for instability and lumbar pain.4 In 1933, Ghormley coined the term “facet syndrome” (FS) as an agent responsible for low back pain.5
Radiofrequency (RF) facet joint denervation is a minimally invasive technique in use since the 1970s. Its principle is based on controlled damage to nerve fibres that transmit pain through heat.6 Shealy described the procedure in 1976.7 Basically, an electrode is applied to the proximal portion of the posterior ramus, where it emerges between the facet and the transverse apophysis, thereby creating a lesion in the posterior ramus that stops the transmission of pain originating from its region of innervation.8
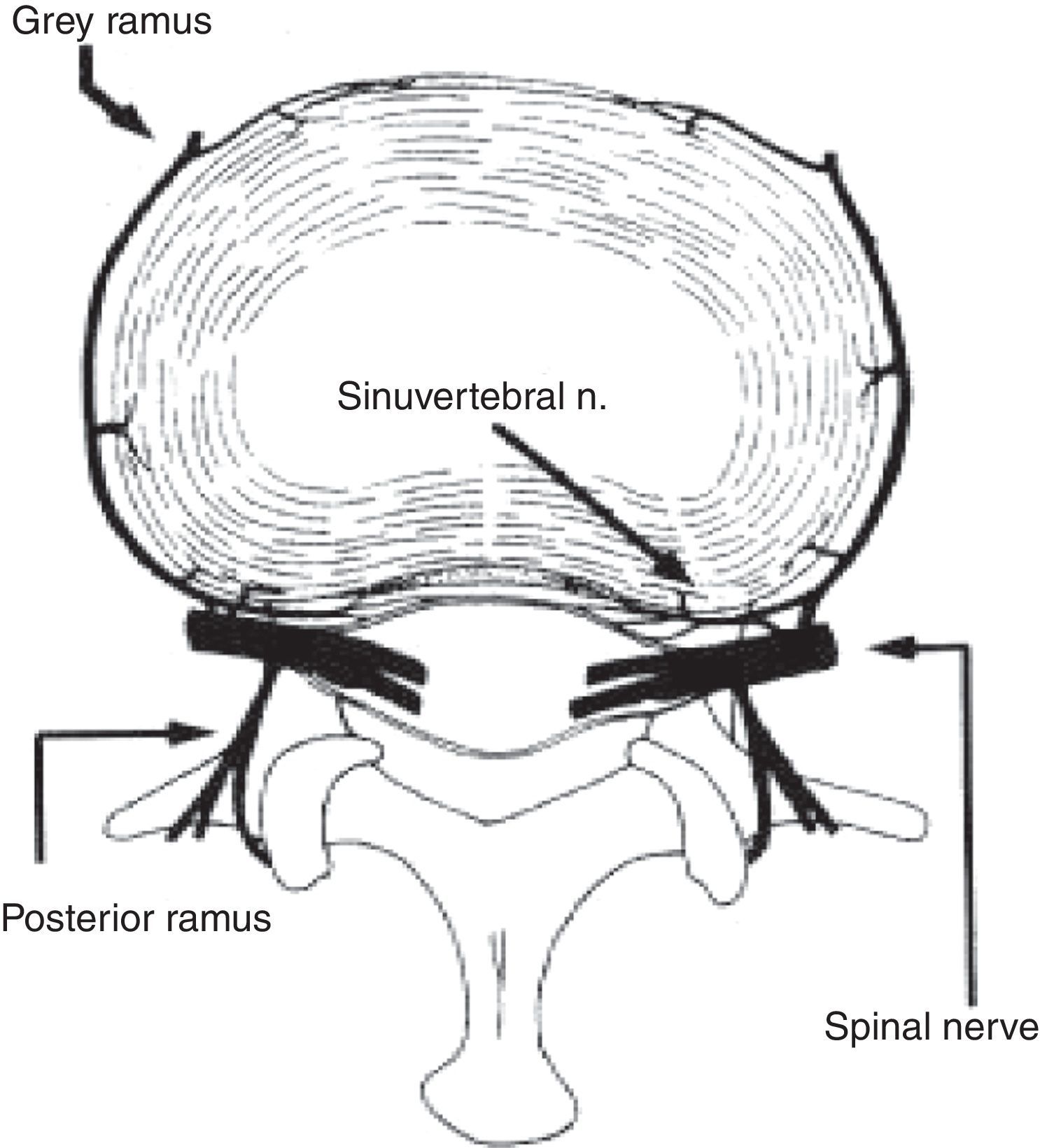
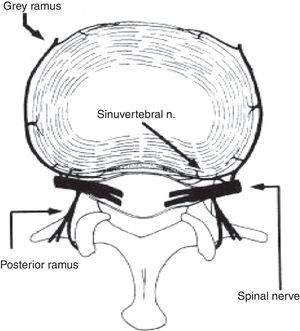
AnatomyFacet joints are synovial, with articular cartilage, a synovial membrane and a fibrous joint capsule.9 In 1850, Luschka described the existence of posterior and accessory innervation.10 In 1980, Bogduk created a simple model of the different rami of the spinal nerve that innervate each lumbar segment.11,12
The facets are innervated by the medial ramus of the dorsal division of the spinal root; the interspinous ligament and the multifidus muscle share this innervation. Each facet joint is innervated by the medial ramus of both the corresponding level and the superior level13 (Fig. 1).
The transmission of painful abnormalities by the posterior ramus, and by the sinuvertebral nerve as it is integrated in the spinal nerve, may be perceived as local pain and/or referred pain. It is not easy to distinguish referred pain from radicular pain.14 Degenerative changes that occur naturally in the disc and interapophyseal joints are integrated and related to the concept of instability and facet syndrome.15
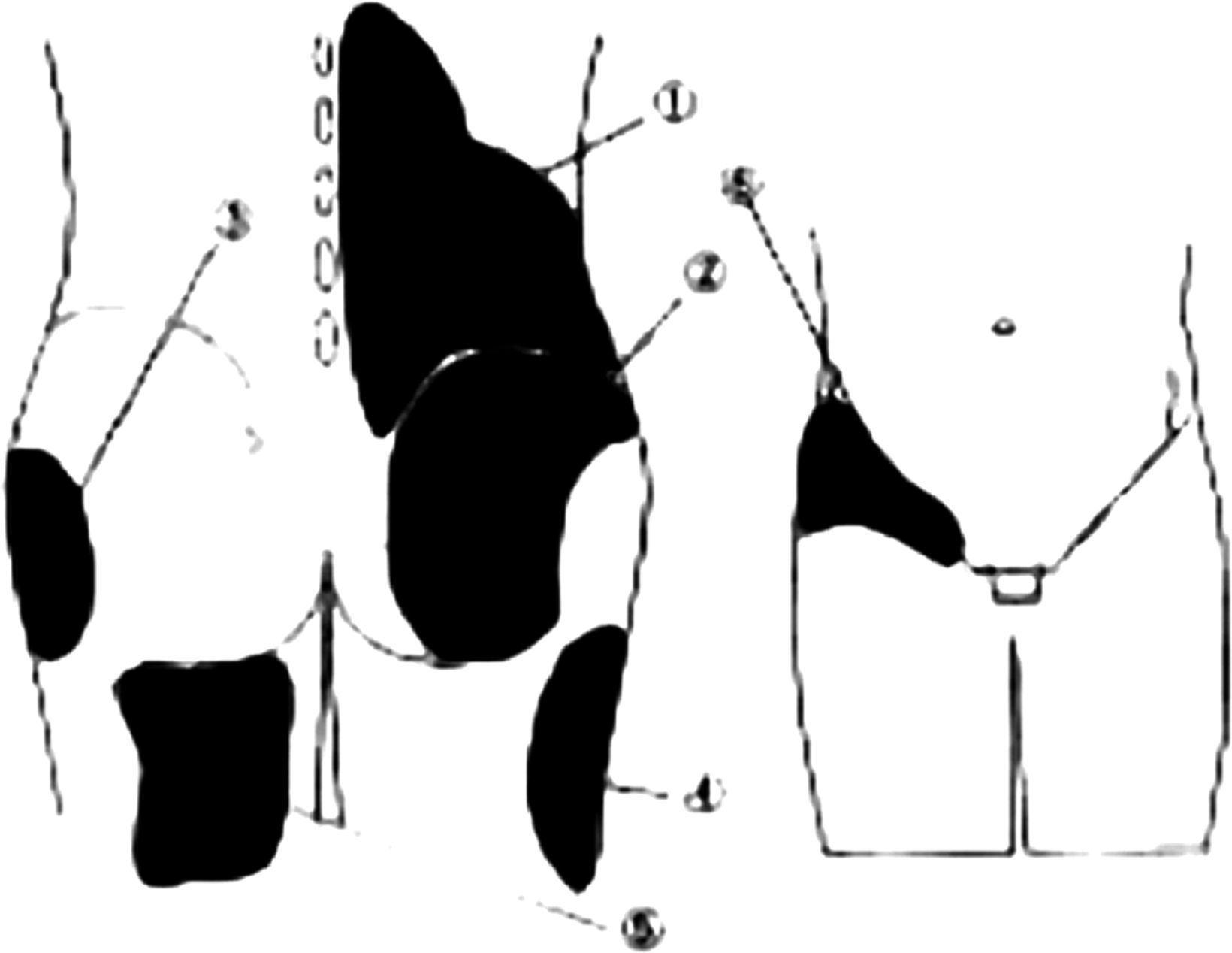
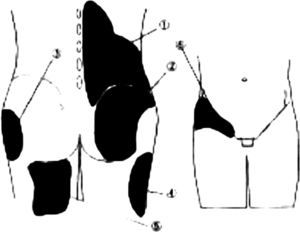
Facet syndrome (FS)FS is used to indicate to patients that they are suffering from mainly low back pain in the vertebral articular facets. Patients report it as a deep, constant pain in the lumbar region whose location is difficult to pinpoint. It increases with standing and prolonged sitting, and sitting up or taking a few steps tends to bring momentary relief. There is the absence of radicular radiation in pain from the facet joints and the presence of referred pain. Fukui et al.16 studied the distribution pattern of referred pain; for purposes of simplification they divided it into six categories: (1) Lumbar region, (2) Gluteal region, (3) Trochanter, (4) Lateral thigh, (5) Posterior thigh, (6) Inguinal region (Fig. 2).
Areas of referred pain. Image representative of the most affected areas. (1) Vertebral and paravertebral low back up to anterior–superior iliac spine. (2) Region of the gluteus maximus and minimus. (3) Lateral region of the gluteus. (4) Posterior and lateral surface of the thigh. (5) Medial region of the posterior surface of the thigh. (6) Region of anterior inguinal fold, anterior iliac spine up to pubic symphysis.
The facet provocation sign, reported by Acevedo,17 provides a sensitivity of 95% and a specificity of 90%, thereby achieving sufficient parameters to be considered to be significant in examining patients with suspected facet disease or FS. The response to anaesthetic facet block and its link to low back pain have been researched by various authors such as Jackson et al.18 The facet block technique consists of fluoroscopy-guided injection of a local anaesthetic around the corresponding facet joint(s). A positive response is considered to have been achieved when lumbar symptoms temporarily disappear or improve. Perhaps the best marker of low back pain from the facet joints is found on suitably combining a determination of signs and symptoms, examination findings, imaging tests and an anaesthetic facet block; this may then offer a greater likelihood of pain relief through percutaneous lumbar facet RF denervation.18
According to imaging findings in magnetic resonance imaging (MRI), degenerative facet changes may be classified as: Grade I with normal joints; Grade II with a decrease in interarticular space or small bone spur formation; Grade III joint sclerosis or moderate bone spur formation; Grade IV marked bone spur formation.19 Another radiological finding that has been linked as a causal factor is a facet synovial cyst.20 Imaging studies (X-rays, tomography, MRI and scintigraphy) are capable of detecting degenerative facet and/or disc changes, but often have limited clinical correlation.13 Therefore, the absence of radiological facet joint anomalies does not rule out a clinical diagnosis of lumbar FS.21
Radiofrequency (RF)In 1931, Kirschner introduced diathermocoagulation of the trigeminal ganglion in the treatment of trigeminal neuralgia. Shealy introduced the first clinical application of RF in lumbar pain in 1976 with a lesion of the posterior ramus.22
RF aims to induce a thermal lesion in the tissues through emission of electromagnetic energy. The patient is part of a closed circuit that includes a RF generator, a needle (electrode) and a dispersive electrode. A field of alternating electrical energy is created within the patient's tissue. Given the high resistance relative to the tissue, in comparison with the metal electrode, ionic agitation is caused, which creates friction at the molecular level, which leads to an increase in intracellular temperature, which produces heat, located interstitially at temperatures greater than 60°C (60–80°C); cell proteins denature and coagulate quickly.23
Lesion characteristics- (1)
Temperature: the higher the temperature, the greater the lesion. Nerve temperature greater than 45°C=lesion.
- (2)
Time to reach thermal equilibrium: normally thermal equilibrium is reached in 60s (60–90s). The extent of the lesion grows exponentially but remains independent in time after 30s.24
- (3)
Electrode configuration and size: lesion size varies depending on the thickness and length of the active tip.
- (4)
Tissue characteristics: These vary depending on the electrical resistance of the tissue.
There are two types of lesion due to radiofrequency:
- (1)
Conventional radiofrequency tries to interrupt sensory conduction. A lesion is created using heat from 60°C to 90°C, and is mainly used for a cervical and lumbar facet joint block and a sympathetic block.23
- (2)
Pulsed radiofrequency, at a lower temperature (40–60°C), tries to partially interrupt nerve conduction. It is used on the dorsal root ganglion in the metameric segment of the pain and for a peripheral nerve lesion.23
This is performed in the operating theatre or catheterisation laboratory using an imaging intensifier for direct radiological visualisation of the position of the electrode during the procedure. Local anaesthesia and mild sedation are used, allowing for patient cooperation.
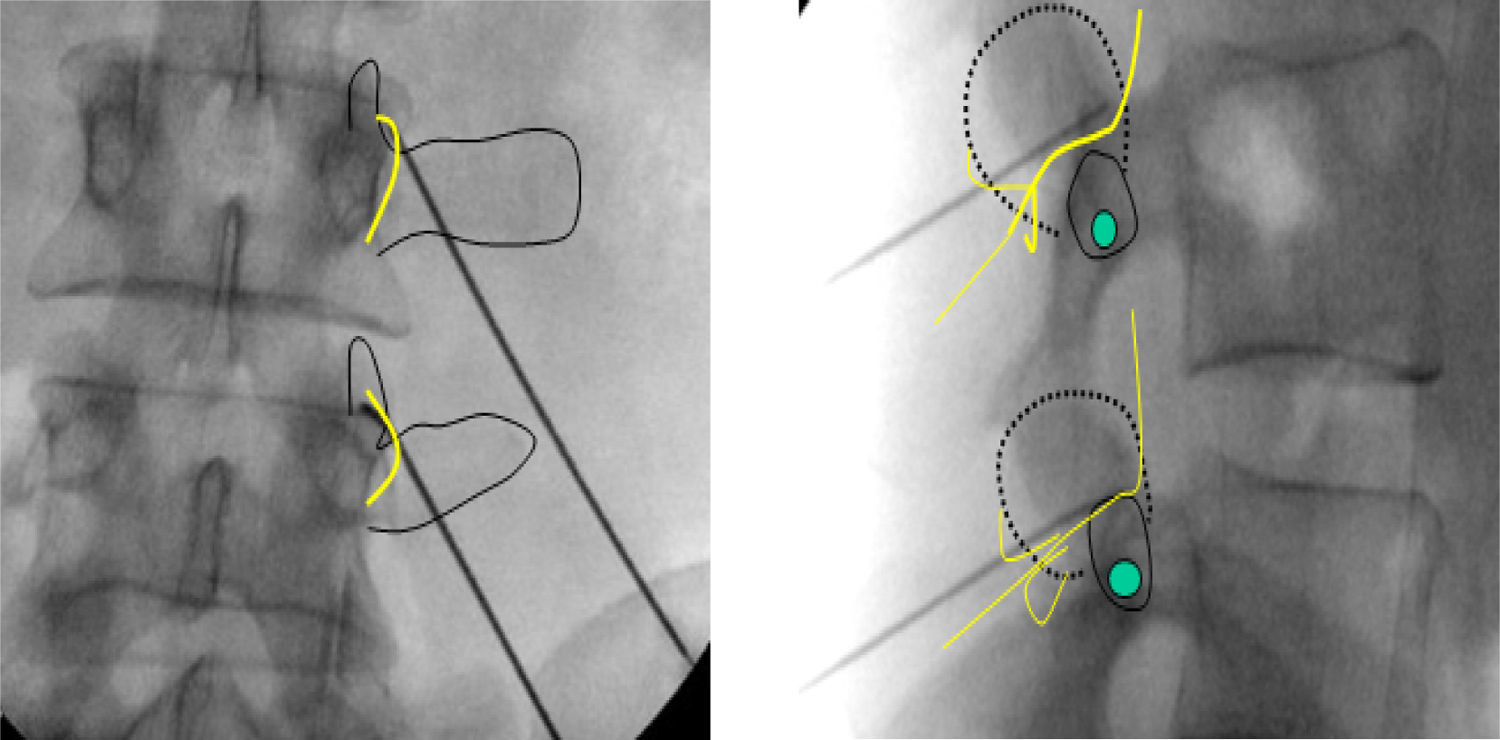
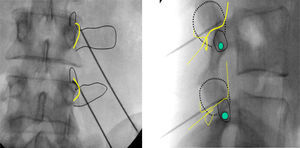
A small incision with a scalpel of 0.5cm or less must be used to overcome skin resistance with the electrode. The electrode is inserted at a 45° angle and the electrodes are placed with fluoroscopic monitoring using an anterior–posterior projection. The location of the electrodes in relation to the intervertebral foramen and therefore to the anterior ramus is confirmed using a lateral projection25 (Fig. 3). The electrodes must be parallel to the nerve ramus. They must be inserted obliquely from the tail to the head. The joint facet is imagined to be divided into 4 equal quarters with a bisecting horizontal line and a bisecting vertical line, so that the tip of the electrode is located in the central two quarters of the superior articular process, and at L5 in the posterior and central third of the superior articular process of S1.25
Fluoroscopic monitoring in AP and lateral projection during electrode insertion and relationship to the posterior ramus. AP lumbar X-ray. Yellow line: superior articular facet; thin black lines: transverse apophyses and upper part of superior facet in articulation with inferior facet of superior vertebra; thick black line: thermocoagulation electrode. Lateral X-ray. Green spot marks area to be lesioned with electrocauterisation, level of passage of the nerve, with exit through intervertebral foramen.
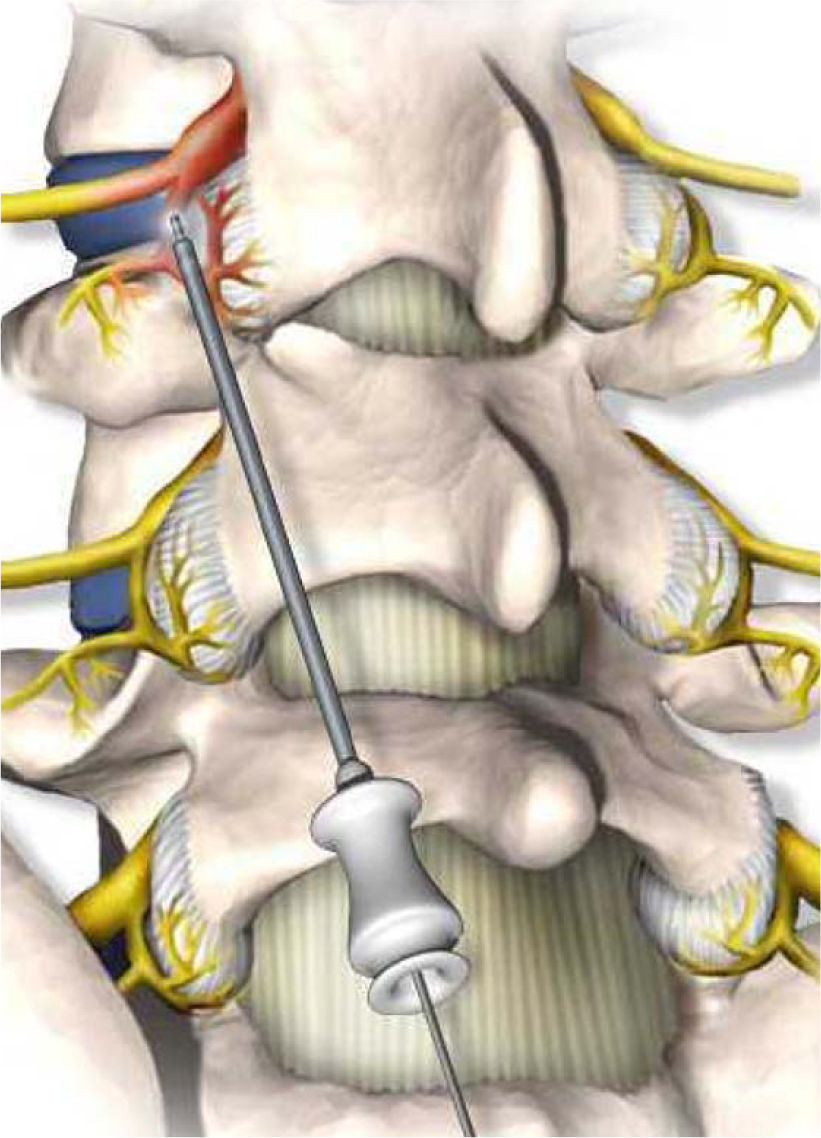
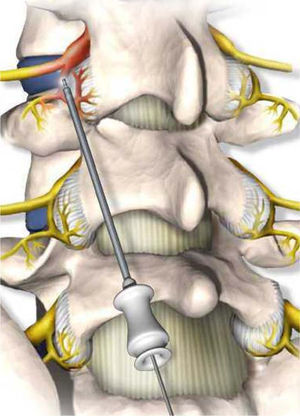
Before the lesion is caused by RF, sensory stimulation is used to confirm that there is no motor stimulation up to 2 volts (V). In many cases, sensory stimulation reproduces the patient's pain. This is a sign of a good prognosis for the outcome. Once anterior verification has been done, facet denervation can be performed using thermocoagulation with an electrode at 80°C for 90s.26 The heat generated to cause the lesion is limited to an approximate volume of a sphere with a diameter of 0.5–1cm (Fig. 4). With time, destruction by coagulation of the nerve fibres of the posterior ramus in the coagulated area causes an area of fibrosis and atrophy due to denervation of the musculature.
DiscussionThe difficulty of assessing the results of facet thermocoagulation derives from the type of patient, who tends to have a chronic condition with associated psychological, social and occupational factors. The selection of these patients must be rigorous: patients with pure signs and symptoms of FS must be selected, and patients who have even had prior surgeries—which could confuse the treating physician by masking the process of FS such that the physician changes the treatment to more invasive procedures with sub-optimal outcomes—must not be excluded.
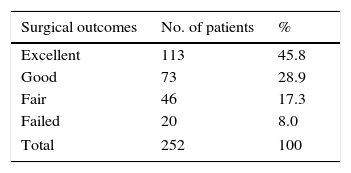
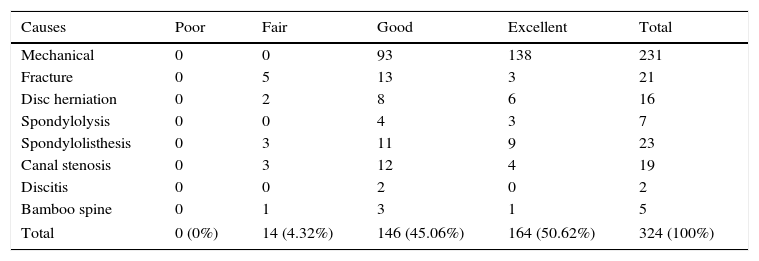
The most recently published studies have indicated a rate of good outcomes around 70–80%, with symptomatic improvement remaining around 71% for more than six months and with an average of 2 years with no signs or symptoms of FS. The mean duration of relief following facet thermocoagulation is 10.5 months (range of 4–19 months).27 A study conducted by Martinez-Suarez et al.28 evaluated 252 patients and achieved very encouraging outcomes, with 74.7% of patients experiencing symptomatic improvement (Table 1). Moreover, Cho et al.29 studied 324 patients and demonstrated with the results obtained that improvement was achieved in up to 90% of them, with 45.1% achieving “good” outcomes and 50.5% achieving “excellent” outcomes. They also showed the most common cause of FS (Table 2).
Distribution of patients according to radiofrequency surgery outcome in facet syndrome.
| Surgical outcomes | No. of patients | % |
|---|---|---|
| Excellent | 113 | 45.8 |
| Good | 73 | 28.9 |
| Fair | 46 | 17.3 |
| Failed | 20 | 8.0 |
| Total | 252 | 100 |
Ref. 28.
Outcomes in accordance with causes of low back pain.
| Causes | Poor | Fair | Good | Excellent | Total |
|---|---|---|---|---|---|
| Mechanical | 0 | 0 | 93 | 138 | 231 |
| Fracture | 0 | 5 | 13 | 3 | 21 |
| Disc herniation | 0 | 2 | 8 | 6 | 16 |
| Spondylolysis | 0 | 0 | 4 | 3 | 7 |
| Spondylolisthesis | 0 | 3 | 11 | 9 | 23 |
| Canal stenosis | 0 | 3 | 12 | 4 | 19 |
| Discitis | 0 | 0 | 2 | 0 | 2 |
| Bamboo spine | 0 | 1 | 3 | 1 | 5 |
| Total | 0 (0%) | 14 (4.32%) | 146 (45.06%) | 164 (50.62%) | 324 (100%) |
Ref. 29.
The published outcomes of lumbar facet thermocoagulation vary widely, from 9% to 83%.30 The reasons for this wide range of outcomes are variable. The patient's anatomy must be known; other processes of joint or surgery-related disease, which determine or mask FS, must be ruled out; and the fact that the regeneration of medial roots and Luschka joints occurs in the middle term at 10–12 months must be taken into account, as they will influence these outcomes. Facet thermocoagulation thus performed can be repeated several times, as it is a symptomatic treatment, provided that the same criteria that apply to facet pain are used. Both the duration of symptomatic relief and the rate of good outcomes remain constant in each repeated procedure. In patients with short-term failure or recurrence of pain following two or more procedures, there is the option of an arthrodesis as a definitive treatment, which seems to be a more reasonable form of treatment for this type of disease.
ConclusionsFacet thermocoagulation is a minimally invasive procedure aimed at symptomatic treatment of chronic low back pain from the facet joints. It is an effective tool for the treatment of low back pain despite the lack of more homogeneous outcomes in the medical literature. Proper patient selection is precisely the most complex part of the process, owing to the diagnostic difficulty of identifying FS as the cause of low back pain, given that it may be mistaken for radicular pain or chronic inflammatory muscle processes that may simulate the symptoms of FS. The accompanying morbidity is very low and the surgical technique as such does not present any major difficulties or complications. In our opinion, facet thermocoagulation must be considered, even with its limitations, as a valid alternative for chronic lumbar pain on any unit specialised in diseases of the spinal column, and as an option prior to arthrodesis in patients who have improved following an anaesthetic facet block.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.