Cadaveric models offer a realistic surgical procedure simulation platform in the operating theatre, which facilitate the learning of new techniques without inherent risks for the patient. The objective of this study is to report our experience using the TaTME (transanal-total mesorectal excision) approach in a cadaveric model in the Clinical Simulation Department of the Tecnológico de Monterrey School of Medicine, at the Monterrey Campus. A total of 5 laparoscopic abdominal and TaTME procedures were conducted simultaneously using the GelPOINT Path platform® (Applied Medical, Rancho Santa Margarita, CA, USA). The average time for the abdominal procedure was 71min, while the transanal procedure lasted 74min. In 4 of the cadavers, a total mesorectal excision was achieved, with a near total mesorectal excision in the remaining cadaver. A conventional transabdominal procedure had to be conducted on one of the cadavers due to technical difficulties experienced in tissue manipulation. We conclude that the cadaveric model offers a suitable platform for learning new surgical techniques, with high a degree of similarity to the surgical procedures performed on living patients. A key factor is the tissue consistency of the cadaver for adequate manipulation.
Los modelos cadavéricos ofrecen una plataforma muy cercana a la realización de un procedimiento real en los quirófanos, lo que facilita el aprendizaje de nuevas técnicas sin poner en riesgo a un paciente. El objetivo de este estudio es reportar nuestra experiencia en la realización del abordaje TaTME (Transanal-Total Mesorectal Excision) en modelo cadavérico en el Departamento de Simulación Clínica de la Escuela de Medicina del Tecnológico de Monterrey, Campus Monterrey. Se realizaron un total de 5 procedimientos, con abordaje transabdominal laparoscópico, y escisión mesorectal total transanal (TaTME) simultáneos, con la plataforma GelPoint PathMR (Applied Medical, Rancho Santa Margarita, CA, EUA). El tiempo promedio del procedimiento abdominal fue de 71 minutos, y del procedimiento transanal fue de 74 minutos. En los 5 cadáveres se obtuvo una escisión mesorectal completa macroscópica. En uno de los cadáveres se requirió realizar el abordaje abdominal de forma convencional debido a dificultades técnicas para la disección. Consideramos que el uso del modelo cadavérico en el aprendizaje de nuevas técnicas quirúrgicas ofrece una plataforma adecuada con gran similitud a los procedimientos que se realizan en los pacientes, sin poner en riesgo la integridad de las personas. Un punto clave es el estado de los tejidos de los cadáveres que permita la manipulación adecuada.
Many surgical procedures have been performed as part of experimental laparoscopic training, mostly on animals. To our knowledge, in our field there is no practical training course for colorectal laparoscopic surgery that follows a cadaveric model.
The value of surgical training courses on human cadavers has been studied in other countries. Various conventional and laparoscopic surgical procedures have been performed using this type of model. In recent years, the TaTME approach has become more widespread in numerous countries as an additional rectal surgery approach to treat neoplastic or inflammatory diseases.
History of the TaTME approachTotal mesorectal excision is currently considered to be the surgical approach of choice for the treatment of rectal cancer. Traditionally, open surgery was performed, but current studies like the COREAN trial and the COLOR II trial have shown that there are no statistically significant differences between open surgery and laparoscopic surgery groups in terms of the mesorectal excision of mid-rectal and proximal rectal tumours, while the laparoscopic approach was found to be superior in patients with lower rectal cancer. However, the main limitation of the purely laparoscopic approach is its inadequate reach in obese patients, patients with a narrow pelvis or patients undergoing conservative sphincter procedures.1
Although reports of transanal endoscopic microsurgery date back to 1985 by Bues,1,2 the first laparoscopic-assisted transanal total mesorectal excision was reported by Sylla et al. in 2010,10 in a patient with a rectal tumour 8cm from the anal margin. Since then, numerous case series have been reported using these approaches, the largest of which were the 30-patient series by Rouanet (2013)3 and the 20-patient series by Lacy (2013). In the Rouanet series, 29 of the 30 patients with lower rectal cancer had received neoadjuvant therapy, reporting a 6% conversion rate, no short-term mortality and 30% morbidity. R0 resection was achieved in 87% of patients and the mean 12-month and 24-month survival rates were 96.6% and 80.5%, respectively. The 12-month and 24-month disease-free survival rates were 93% and 88.9%, respectively. The authors reported a selection bias in favour of high-risk patients, advising caution before generalising this approach.3
ObjectiveThe objective of this descriptive study is to report on a series of cases, as well as our experience in the implementation of laparoscopic transabdominal TaTME in a cadaveric model.
Material and methodsFive human cadavers donated by the School of Medicine and Health Sciences of the Monterrey Institute of Technology and Higher Education (ITESM) were used. The cadavers were prepared using the Thiel embalming technique. Infectious/contagious disease was ruled out in the diagnosis and cause of death of all the cadavers. Two experienced colorectal surgeons supervised five colorectal procedures, each employing the TaTME (transabdominal-transanal) approach. Four of the operations were laparoscopic, while the fifth was conventional. Of the five anastomoses performed, four were manual and one mechanical. GelPOINT Path (Applied Medical, Rancho Santa Margarita, CA, USA) was used for transanal access. The procedures were conducted at the “Centro de Habilidades y Destrezas Médico-Quirúrgicas” (Centre for Medical-Surgical Skills and Proficiency) at facilities covering approx. 70 m2 intended for the conduct of surgery simulations, experimental techniques and virtual laparoscopic simulators, as well as more basic surgical training.
Two sets of laparoscopic equipment were used simultaneously; one for the transabdominal approach and the other for the transanal approach.
The cadavers were placed in a modified lithotomy and slight Trendelenburg position, similar to TaTME surgery conducted on live patients (Fig. 1). In the four laparoscopic abdominal procedures, the following ports were inserted: an 11mm umbilical port for the camera, an 11mm port in the left flank and a 5mm instrument port in the left hypochondrium. For dissection, the Enseal (Ethicon endosurgery, Johnson & Johnson, Somerville NJ, USA) and LigaSure (Covidien-Medtronic, Minneapolis, MN, USA) energy-based devices were used.
A standard low anterior resection was performed for the abdominal approach, initiating anterior mobilisation of the mesorectum, followed by the lateral portions and finally the posterior portion. As mentioned above, the ports were placed in the same way as they would be in a live patient.
At the same time, a second team performed the transanal procedure as follows: a Lone Star anal retractor was placed, the anal canal was closed using a purse-string suture and the rectal mucosa was circumferentially scored to mark the next dissection site. The GelPOINT Path port (Applied Medical, Rancho Santa Margarita, CA, USA) was then inserted and the insufflation tube placed in the gas expulsion site, facilitating gas expulsion through the insufflation port. As we used pulsed insufflation rather than continuous-flow insufflation, this inversion of the pneumorectum entry and exit sites facilitated more consistent and slightly better regulated insufflation. A distal and proximal circumferential dissection was then conducted through the intersphincteric plane and the perirectal fat was identified and circumferentially dissected until contact was made with the abdominal laparoscope. The same structures as those in a live patient were identified and preserved (prostate, seminal vesicles, etc.).
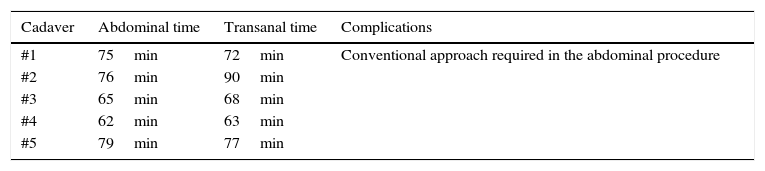
ResultsThe five procedures were completed without any complications. The surgeons performing the procedures did note, however, that the tissue was slightly harder to manipulate than live tissue, which is more flexible. Although the specimens were not sent for histopathological study, total mesorectal excision was achieved on a macroscopic level in all cases (Fig. 2). The average transabdominal and transanal procedure times were 71min and 74min, respectively, both of which are lower than the usual times reported in medical literature for procedures on living patients. This is clearly due to the lack of bleeding and the reduced risk of potential injury to adjacent structures. Table 1 summarises the surgical times for each cadaver.
DiscussionSome studies, most of which are small, have reported the use of cadavers to practice colorectal surgical techniques. However, very few laparoscopic colorectal procedures have been reported using a cadaveric model, although this practice is common at certain healthcare institutions. The lack of availability and high cost of cadavers, coupled with the lack of active bleeding and the stiffer, less flexible tissue, are the main limitations to the use of this approach. However, it could be established as a standard practice to simulate laparoscopic colorectal procedures in an initial training setting. Universal safety measures should be maintained as the potential risk of exposure to a biological material may vary based on the preparation technique employed. There continues to be a risk of infectious or contagious disease transmission with the use of cadavers in medicinal practice. There is a particular risk of prion infection from the manipulation of central nervous system tissue as the preparation techniques employed are less effective at eradicating prions than other pathogens. It is therefore advisable to use cadavers that did not die or suffer from chronic or non-chronic infectious diseases, and to adopt the appropriate safety measures for tissue handling.5
Individual studies such as that conducted by Levine in Kentucky, USA, report the use of cadavers as an instrument to transfer skills acquired in the digital laparoscopic simulator, specifically laparoscopic suturing.4 Moreover, He and Mou reported the conduct of a renal transplant using an extraperitoneal approach, concluding that training on human cadavers is a viable approach.6
In 2010, Asano7 reported a two-day practical course on human cadavers in which colonic resections were practised. There were 39 participants, the mean of which had 10 years’ practical surgical experience. The participants completed a questionnaire at the beginning and end of the training, as well as six months later. The participants considered themselves to be better prepared to conduct this type of surgery. In the questionnaire completed six months after the course, 10 of the 16 questionnaire respondents (who had not performed laparoscopic colon surgery before) went on to conduct at least one laparoscopic colorectal surgical procedure.
A systematic review by Gilbody8 revealed significant findings concerning training based on a cadaveric model. Eight articles met the inclusion criteria and only two included laparoscopic procedures. However, none assessed the implementation of the clinical skill after training. The main benefit reported by the medical staff who received the training was a subjective improvement in spatial perception of the anatomy. The main limitation reported was the relatively rapid decomposition of the cadavers, leading to a foul smell and the absence of bleeding, which is a challenge to overcome in living tissue.
More recently, White9 reported a cadaver-based training programme for laparoscopic liver resections. The authors concluded that a dedicated laparoscopic liver resection facility is an excellent training method that also has the potential to provide certification within this surgical technique.
By applying video-assisted transanal surgery models to porcine and human cadaveric models, the Massachusetts General Hospital NOTES (Natural Orifice Translumenal Endoscopic Surgery) group demonstrated the viability of endoscopic full-thickness dissections of the rectum and even the possibility of extending the dissection to the perirectal fat in order to achieve complete circumferential mobilisation of the rectum.9 Furthermore, the Atallah group in Florida developed a technique known as TAMIS (TransAnal Minimally Invasive Surgery), which is a hybrid between transanal endoscopic microsurgery (TEM) and single-port laparoscopy. For this technique, a single-incision laparoscopic surgery port (SILS Port, Covidien) was inserted into the anal canal by applying steady manual pressure. Once seated in position, pneumorectum was established, enabling the insertion of ordinary laparoscopic instruments. This first report included six patients, in which a significant reduction in operating time was observed versus traditional TEM surgery (86min vs 120–140min), alleging that this was mainly due to the ease of the approach.2
A systematic review by Gilbody8 revealed significant findings concerning training based on a cadaveric model. The author reported the high cost of cadaver use for simulation in the United Kingdom, which was a secondary factor to the low number of cadavers donated (674 cadavers for all the medical schools of the United Kingdom in 2005). As a result, the author's intention was to report those training courses for which the use of human cadavers offered a significant benefit. Of the 38 articles found in medical literature, eight met the inclusion criteria, with articles pertaining to surgical training being exclusively selected. Only two of the eight publications found by the authors included laparoscopic procedures, while none assessed the implementation of the clinical skill after training. The procedures reported in Supe's publication (2005) were: cholecystectomy, appendectomy, splenectomy, intestinal explorations, mesenteric lymph node biopsy and varicocele-vein occlusion. Giger (2008) studied the use of advanced colon, hernia, bariatric and vascular surgery laparoscopic techniques (see below).7
The fact that these two studies failed to assess skill acquisition after the training course is a significant hindrance to assessing the benefits of cadaver-based training in laparoscopic procedures. The main benefit reported by the medical staff who received the training was a subjective improvement in spatial perception of the anatomy. The main limitation reported was the relatively rapid decomposition of the cadavers, leading to a foul smell (in both publications the Thiel embalming technique was used) and the absence of bleeding, which is a challenge to overcome in living tissue. The author concluded that the overall perception of the participants who attended the cadaveric training was positive, but that larger studies were needed, specifically studies that focus on the transfer of skills learnt through cadaver-based training to the operating theatre, and the identification of the procedure that benefits most from this expensive training model.7
In the cadaver-based training programme for laparoscopic liver resections reported by White, the participants were asked to assess the course by means of a questionnaire upon completion of the two-day course given by experienced surgeons. This study focussed specifically on participant feedback, who were asked to assess content, structure, results, resources, facility and value for money (0=poor, 6=excellent). 43% of the participants graded the course as excellent, 32% very good (score 5) and 25% good (score 4). The authors concluded that a dedicated laparoscopic liver resection facility is an excellent training method that also has the potential to provide certification within this surgical technique.8
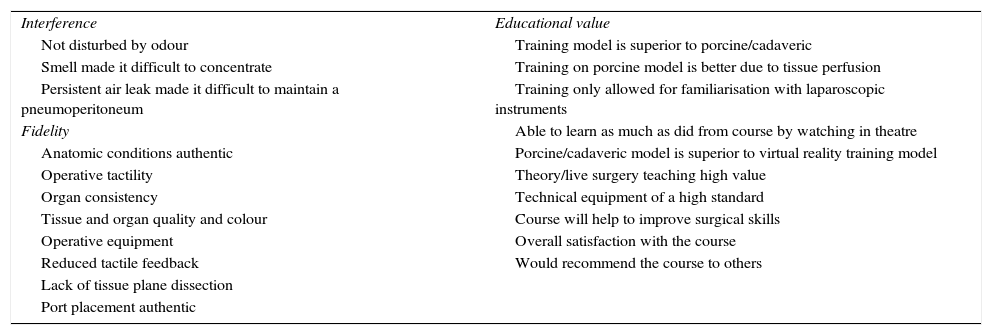
The colorectal training programme of the National Training Programme Education Centre of Imperial College London uses anaesthetised pigs and fresh cadavers for practical colorectal surgery training sessions after theoretical training. At this centre, the following procedures are practised: right, left and transverse colectomies, Hartmann's procedure (and the reversal thereof), sigmoidectomy with and without splenic flexure mobilisation and low and abdominoperineal anterior resection. The participants at this site were asked to fill in a questionnaire to assess a total of 21 parameters concerning interference (by factors of the model used), the fidelity of the model used and its educational value. Over a 12-month period, 10 cadaver-based and 3 porcine-based training sessions were conducted. The questionnaires completed by the participants revealed that the porcine model was superior in terms of the quality of tissues and organs, less air leak and lack of disturbance due to odour, whereas the cadaveric model was superior in terms of anatomy, as a training model and for realistic port placement. Tissue perfusion or bleeding in the cadaveric model did not significantly improve training. Table 2 details the parameters assessed during these courses.11
Parameters assessed during the Imperial College course.
| Interference | Educational value |
| Not disturbed by odour | Training model is superior to porcine/cadaveric |
| Smell made it difficult to concentrate | Training on porcine model is better due to tissue perfusion |
| Persistent air leak made it difficult to maintain a pneumoperitoneum | Training only allowed for familiarisation with laparoscopic instruments |
| Fidelity | Able to learn as much as did from course by watching in theatre |
| Anatomic conditions authentic | Porcine/cadaveric model is superior to virtual reality training model |
| Operative tactility | Theory/live surgery teaching high value |
| Organ consistency | Technical equipment of a high standard |
| Tissue and organ quality and colour | Course will help to improve surgical skills |
| Operative equipment | Overall satisfaction with the course |
| Reduced tactile feedback | Would recommend the course to others |
| Lack of tissue plane dissection | |
| Port placement authentic |
Despite operating on cadavers, the procedures conducted using this equipment were largely completed without any complications and with an acceptable operating time for the procedure. The average cost of a cadaver is high (around 14,000 pesos) and they must be specially prepared to ensure a tissue consistency that is compatible with the use of laparoscopic techniques. Facilities and instruments designed specifically for this purpose are also required. These factors have almost certainly restricted the wider deployment of this type of cadaver-based training.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.
We would like to thank Mr Sergio Omar Rodríguez Navarro (engineer) and Mr Javier Hernández Juárez for their assistance in conducting the simulation.