Weight mismatch has been a controversial issue in the literature and there is also no agreement on the anthropometric parameter that best predicts outcome in such cases. The purpose of this study was to correlate anthropometric and echocardiographic variables to adequately select donors for cardiac transplant.
MethodsA total of 399 adult patients with normal echocardiograms were prospectively and consecutively included. Patients with coronary risk factors, systemic diseases and poor acoustic windows were excluded.
ResultsThe mean age of the population was 43±17 years and 39% were male. All anthropometric variables were associated in a linear, positive and statistically significant manner with each of the echocardiographic variables. Marked variations in weight were accompanied by lesser variations in end-diastolic diameter in both men and women.
End-diastolic diameter was greater in patients with normal weight compared to low-weight patients (4.46±0.83cm vs 4.09±0.68cm), p=0.013, and in overweight compared to normal weight patients (4.61±0.88cm vs 4.46±0.83cm), p=0.010, whereas there was no difference between obese and overweight patients (4.74±1.14cm vs 4.61±0.88cm), p=0.760.
ConclusionAlthough anthropometric variations are associated with changes in heart size, such changes are not echocardiographically relevant. This exploratory study opens the door to further investigations to define the donor-recipient anthropometric threshold for accepting an organ in cardiac transplantation.
Las disparidad antropométrica ha sido un tema controversial en el trasplante cardíaco. No hay acuerdo acerca de cuál es la medida antropométrica que mejor predice la evolución en estos casos. El propósito del estudio fue correlacionar las variables antropométricas con las ecocardiográficas para la selección de donantes en el trasplante cardiaco.
MétodosSe incluyeron prospectivamente 399 pacientes con ecocardiograma normal. Se excluyeron a pacientes con factores de riesgo coronarios y enfermedades sistémicas.
ResultadosLa edad media fue de 43 años y el 39% fueron hombres. Todas las variables antropométricas se asociaron en forma lineal, positiva y estadísticamente significativa con cada una de las variables ecocardiográficas. Grandes variaciones en el peso se acompañaron de variaciones menores en el diámetro de fin de diástole en ambos sexos.
El diámetro al final de la diástole fue mayor en los pacientes con normopeso respecto a aquellos con bajo peso (4.46±0.83cm vs 4.09±0.68cm), p=0.013 y en los pacientes con sobrepeso en relación a aquellos con normopeso (4.61±0.88cm vs 4.46±0.83cm), p=0.010; mientras que no hubo diferencias entre los pacientes con obesidad y sobrepeso (p=0.760).
ConclusiónLas variaciones antropométricas si bien se asocian a variaciones en el tamaño del corazón, estos cambios no son clínicamente relevantes. Este estudio exploratorio abre la puerta para investigaciones futuras para definir el umbral de aceptación de órganos respecto de la relación antropométrica entre donante y receptor.
The prevalence of heart failure in the United States is on the increase.1 Medical treatment has been shown to reduce mortality rates and re-admissions to hospital and in the more advanced forms, the treatment of choice is orthotopic heart transplant.2–9 There is a continuous rise in the number of patients on the waiting list, but no increase in the number of donors, so many patients die before having access to a transplant. Broadening donor acceptance criteria could be a strategy for changing this situation. The disparity in anthropometric variables has been a controversial issue in the literature. There are conflicting results when the donor's body size is smaller than the recipient. In these circumstances, some authors have reported a decrease in survival, while for others there is no difference.9,10 There is also a lack of agreement on the anthropometric measurement that best predicts the outcome in these cases.9–11 Moreover, the relationship between the various anthropometric variables and the echocardiographic variables that express the size of the heart is not fully understood. The purpose of this study was to correlate these variables for the appropriate selection of donors in cardiac transplantation.
MethodsStudy populationWe prospectively included 399 patients aged over 18 years with normal echocardiogram consecutively as they attended the echocardiography laboratory for various reasons in the period between January 2008 and June 2010. We excluded patients with coronary risk factors, systemic diseases and poor echocardiographic window. Normal echocardiogram was defined as the absence of structural or functional pathology at the time of evaluation.
Statistical analysisContinuous variables were expressed as the mean and standard deviation; categorical variables as percentages. The correlation of anthropometric variables with echocardiographic variables was performed using simple linear regression. A subgroup analysis was then performed to test differences in both genders regarding the relationship between anthropometric and echocardiographic variables, for which interaction terms were created. Differences in end-diastolic diameter (EDD) were explored by different categories of body mass index (BMI), using ANOVA with Bonferroni correction. The analysis was performed with STATA 11.1 and a value of p<0.05 was established as significant.
Definitions anthropometric and echocardiographic variablesThe following anthropometric variables were recorded: weight in kilograms; height in metres; body surface area (BSA) in square metres according to the formula: √height in centimetres*weight/3600; and BMI according to the formula: weight (in kilograms)/(height in centimetres)2.12 Additionally, BMI was divided into four categories (underweight: BMI<18.50kg/m2; normal weight: BMI between 18.50 and 24.99kg/m2; overweight: BMI between 25.00 and 29.99kg/m2; and obese: BMI>30kg/m2).13 The echocardiographic variables analysed were end-diastolic diameter (EDD), end-diastolic volume (EDV), anterior/posterior diameter of the left atrium (LA diameter), left atrium volume (LAV) and left ventricle mass (LV mass) according to the formula: LV mass=0.8*{1.04 [(EDD+posterior wall thickness+septal thickness)3−(EDD)3]}+0.6g.14 The echocardiographic measurements were performed according to the recommendations of the American Society of Echocardiography with a Philips iE33 unit.15
ResultsThe mean patient age was 43.20±17.26 years and 38.60% were male. The rest of the variables are shown in Table 1.
Baseline characteristics of the population n=399.
| Age (years) | 43±17 |
| Male (%) | 154 (39%) |
| Weight (kg) | 67.35±13.65 |
| Height (m) | 1.65±0.10 |
| Body surface area (m2) | 1.75±0.21 |
| BMI (kg/m2) | 24.39±3.81 |
| EDD (cm) | 4.51±0.45 |
| EDV (ml) | 70.96±22.57 |
| LA diameter (cm) | 3.54±0.40 |
| LAV (ml) | 35.91±11.75 |
| LV mass (g) | 160.67±42.37 |
Continuous values are expressed as mean and standard deviation. The categorical variables are expressed as percentages. BMI: body mass index; EDD: end-diastolic diameter; EDV: end-diastolic volume; LA diameter: anteroposterior diameter of the left atrium, LAV: left atrium volume; LV mass: left ventricle mass.
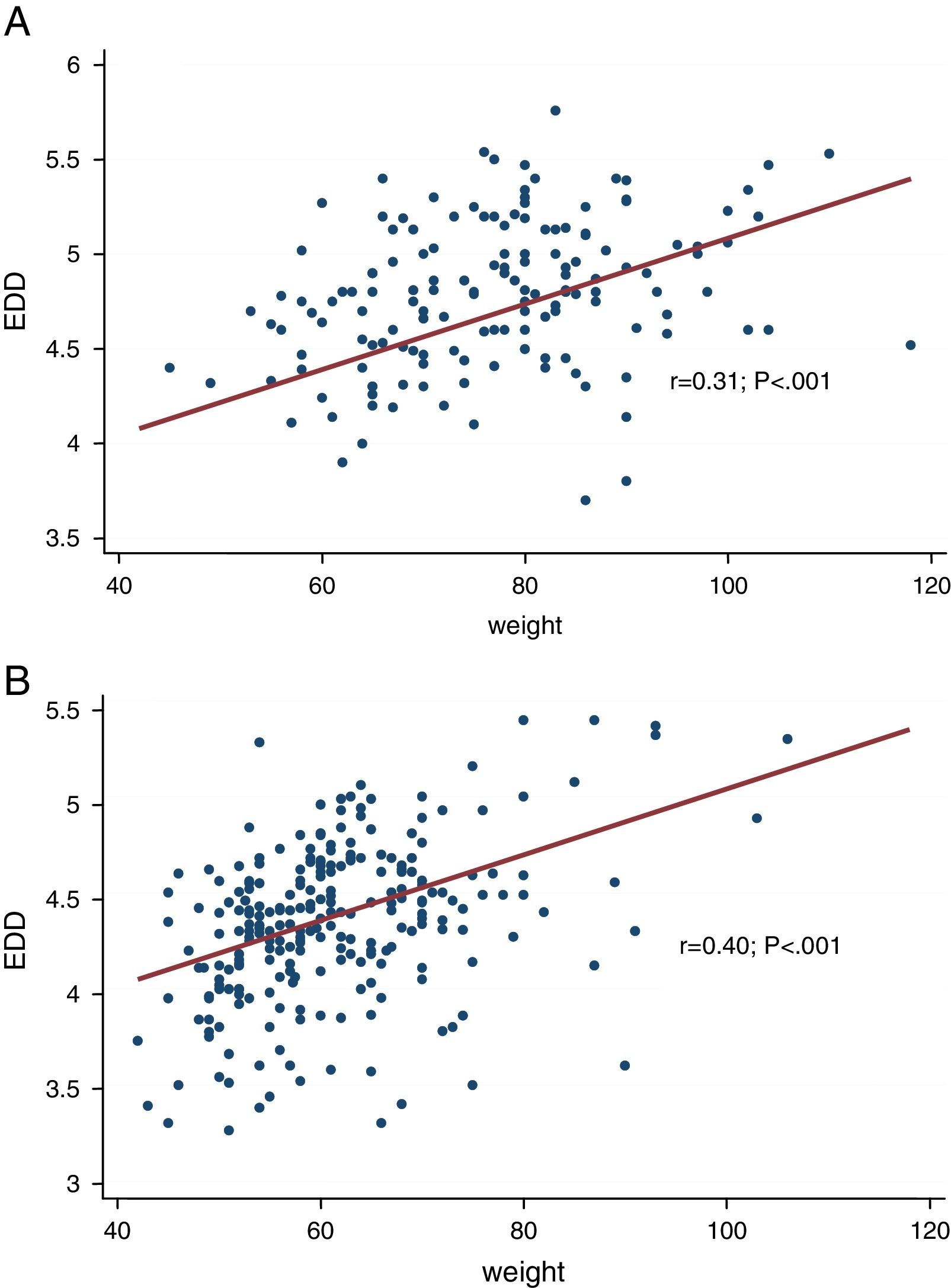
All the anthropometric variables had linear, positive and statistically significant association with each of the echocardiographic variables. Weight and BSA with LV mass were those with the strongest association (r=0.64, p<0.001 and r=0.65, p<0.001) respectively (see Table 2). When analysed by gender, in both males and females, height lost significant association with the atrial parameters and with mass (in the case of females). In each relationship, a gender difference was observed between the strength of association of each of the anthropometric variables with the echocardiographic variables, except in the case of weight and BSA with atrial parameters (p-interaction>0.05) (see Table 3). Fig. 1 shows the relationship between weight and EDD according to gender in graph form.
Correlation between anthropometric measurements and echocardiographic variables.
| EDD | EDV | LA diameter | LA volume | LV mass | |
|---|---|---|---|---|---|
| Weight | 0.52 | 0.49 | 0.48 | 0.39 | 0.64 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| BSA | 0.55 | 0.53 | 0.45 | 0.38 | 0.65 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Height | 0.48 | 0.50 | 0.21 | 0.22 | 0.48 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| BMI | 0.32 | 0.25 | 0.45 | 0.33 | 0.46 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Coefficient of correlation (r) between anthropometric and echocardiographic variables. P value. BSA: body surface area; BMI: body mass index; EDD: end-diastolic diameter; EDV: end-diastolic volume; LA diameter: anteroposterior diameter of the left atrium; LAV: left atrium volume; LV mass: left ventricle mass.
Correlation between anthropometric measurements and echocardiographic variables according to gender.
| EDD | EDV | AP diameter | LA volume | LV mass | |
|---|---|---|---|---|---|
| Weight | |||||
| Males | 0.31 | 0.28 | 0.44 | 0.34 | 0.45 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Females | 0.40 | 0.31 | 0.36 | 0.31 | 0.54 |
| p value | <0.001* | <0.001* | <0.001 | <0.001 | <0.001* |
| BSA | |||||
| Males | 0.33 | 0.29 | 0.41 | 0.32 | 0.44 |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Females | 0.42 | 0.36 | 0.32 | 0.30 | 0.53 |
| p value | <0.001* | <0.001* | <0.001 | <0.001 | <0.001* |
| Height | |||||
| Males | 0.27 | 0.22 | 0.13 | 0.15 | 0.27 |
| p value | <0.001 | <0.005 | 0.092 | 0.064 | <0.001 |
| Females | 0.22 | 0.29 | −0.07 | 0.02 | 0.11 |
| p value | <0.001* | <0.001* | 0.224* | 0.736* | 0.077* |
| BMI | |||||
| Males | 0.22 | 0.22 | 0.39 | 0.46 | 0.32 |
| p value | <0.005 | <0.050 | <0.001 | <0.001 | <0.001 |
| Females | 0.30 | 0.18 | 0.50 | 0.40 | 0.31 |
| p value | <0.001* | <0.005* | <0.001* | <0.001* | <0.001* |
Coefficient of correlation (r) and p value between anthropometric and echocardiographic variables according to gender.
When EDD was analysed by BMI category, it was observed that patients with normal weight had a significantly higher EDD than underweight patients (4.46±0.83cm vs 4.09±0.68cm), p=0.013; overweight patients had a significantly higher EDD than patients with normal weight (4.61±0.88cm vs 4.46±0.83cm), p=0.010; while there were no significant differences between obese patients and overweight patients (4.74±1.14cm vs 4.61±0.88cm), p=0.76 (Table 4).
Relationship between body mass index categories and end-diastolic diameter.
| Under weight 15/399 (3.76%) | Normal weight 223/399 (55.89%) | Over weight 128/399 (32.08%) | Obese 33/399 (8.27%) | |
|---|---|---|---|---|
| EDD (cm) | 4.09±0.68 | 4.46±0.83* | 4.61±0.88† | 4.74±1.14‡ |
BMI categories (underweight: BMI>18.50kg/m2; normal weight: BMI between 18.50 and 24.99kg/m2; overweight: BMI between 25.00 and 29.99kg/m2; and obese: BMI>30kg/m2). EDD: end-diastolic diameter expressed as mean and standard deviation. Comparisons between groups: (*) underweight: p=0.013; (†) normal weight: p=0.010; (‡) overweight: p=0.760; (‡) underweight: p=0.000; (†) underweight: p=0.000; ‡ normal weight: p=0.003.
This study showed a statistically significant association between anthropometric and echocardiographic variables. However in most cases the strength of association between the two was modest, except for the relationship between weight and BSA and LV mass (r=0.64, p<0.001 and r=0.65, p<0.001) respectively.
In practice, the parameters used for selecting a donor heart are usually weight as anthropometric measure and EDD as echocardiographic measurement. In this study, the correlation between the two parameters was modest, both in the population overall (r=0.52, p<0.001) and by gender (r=0.31, p<0.001 in males and r=0.40, p<0.001 in females). Even more interesting was the fact that in this sample, large variations in weight were accompanied by minor variations in the EDD. In this respect, a man of 76.75kg (mean of this population) corresponds to an EDD of 4.78cm, a man of 50.99kg (−2SD from this population) an EDD of 4.02cm and a man of 102.51kg (+2SD from this population) an EDD of 5.54cm. This represents a variability of over 100% in weight and 37% for the EDD. In women, the variability in weight was also over 100%, while for the EDD it was only 17%.
In other centres, BMI is chosen as anthropometric measurement for selecting a donor.16 When the EDD was analysed in the different categories of BMI, it was found that although overweight patients had a greater EDD than patients with normal weight (+0.36cm) and these in turn than those with low weight (+0.15cm), from a clinical point of view, these variations are clearly less than 20%. Moreover obese patients did not have greater EDD than overweight patients.
Relationship between anthropometrics and ventricular function: When we analysed stroke volume (SV) by BMI categories, we found that patients with normal weight had an SV 10ml higher than underweight patients, with a trend towards statistical significance (p=0.054), while overweight patients did not have a higher SV than patients with normal weight (p=1) and nor did obese patients compared to overweight patients (p=1). A single-centre study compared haemodynamic and echocardiographic variables in a group of patients in which small hearts were transplanted versus another group in which normal hearts were transplanted (donor/recipient weight ratio: recipient 0.53±0.06 vs 0.98±0.05). After the transplant, the first group had higher pulmonary pressures, higher filling pressures and lower stroke volume, with a compensatory increase in heart rate. All these parameters normalised at around 10 weeks while greater remodelling was observed resulting from an increase in left ventricular mass. This demonstrates the structural and functional adaptation of a small donor heart to the physiological conditions of a recipient of greater weight.17
Long-term outcome: A study conducted by the United Network for Organ Sharing (UNOS) on 15,284 patients showed that patients with donor/recipient weight ratio less than 0.8 did not have a significantly different 5-year survival than those with a ratio of 0.8–1.2 and those with a ratio >1.2 (p=0.26). However, in the subgroup with increased pulmonary resistance (>4 Wood units), survival was significantly lower (p=0.02).10 In contrast, the Taylor et al. study showed that the lower the BMI ratio between donor and recipient, the higher the mortality rate at 5 years in patients after heart transplantation.9
LimitationsOne limitation of the study lies in the fact that it shows the percentage of patients with extreme BMI was very low; only 3.76% of patients were underweight, while 8.27% were obese, and it is the extremes where major problems arise with respect to the anthropometric variables between donor and recipient. The study also did not include post-transplant haemodynamic variables or early and late clinical progress.
ConclusionAlthough anthropometric variations are associated with changes in heart size, such changes are not clinically relevant. This exploratory study opens the door to further investigations to define the donor–recipient anthropometric threshold for accepting an organ in cardiac transplantation.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflicts of interest.