Thoracoscopy in non-intubated patients is a minimally invasive procedure that allows for performing thoracic procedures without the need for orotracheal intubation. In this article, we describe the case of a patient with renal failure who needed haemodialysis. A Mahurkar catheter was used and, unfortunately, the tip of it was inside the pleural cavity. We decided to remove the catheter by means of a thoracoscopy since there was a possibility of haemorrhage that would need to be controlled. We considered it important to report this case because nowadays it is feasible to perform thoracic surgery without intubation, including complex procedures such as pulmonary biopsy or lobectomy, in carefully selected patients. It is important to mention that it is not possible to use this technique in all cases, but only in carefully selected cases.
La toracoscopia con paciente no intubado es una técnica de cirugía torácica de mínima invasión que permite hacer procedimientos torácicos sin necesidad de intubación orotraqueal. Se reporta el caso de un paciente con insuficiencia renal y necesidad de hemodiálisis, a quien se le había colocado un catéter de Mahurkar que desafortunadamente se encontraba en el la cavidad pleural. Decidimos retirar el catéter con visión toracoscópica ante la posibilidad de sangrado, que ameritara intervención y lograr hemostasia. Consideramos importante reportar este caso ya que es factible no intubar pacientes para la realización de toracoscopia en pacientes bien seleccionados y con procedimientos complejos, tal como biopsias pulmonares o lobectomía. Es importante mencionar que no todos los casos pueden hacerse con ésta técnica, mas que en casos bien seleccionados.
Thoracoscopy in non-intubated patients is a minimally invasive procedure that allows for performing thoracic procedures without the need of orotracheal intubation. Thoracoscopy is usually performed using a selective intubation cannula that deflates the lung by blocking the passage of air to the lung being operated on. In this procedure, patients must be under general anaesthesia and muscle relaxation, to achieve a loss of automatic breathing. Operating on a patient's chest without an orotracheal intubation cannula is a procedure that has not been performed at Hospital General de México. There are reports in the literature of these procedures being used to be able to perform a thoracoscopic lobectomy with a single port in non-intubated patients.
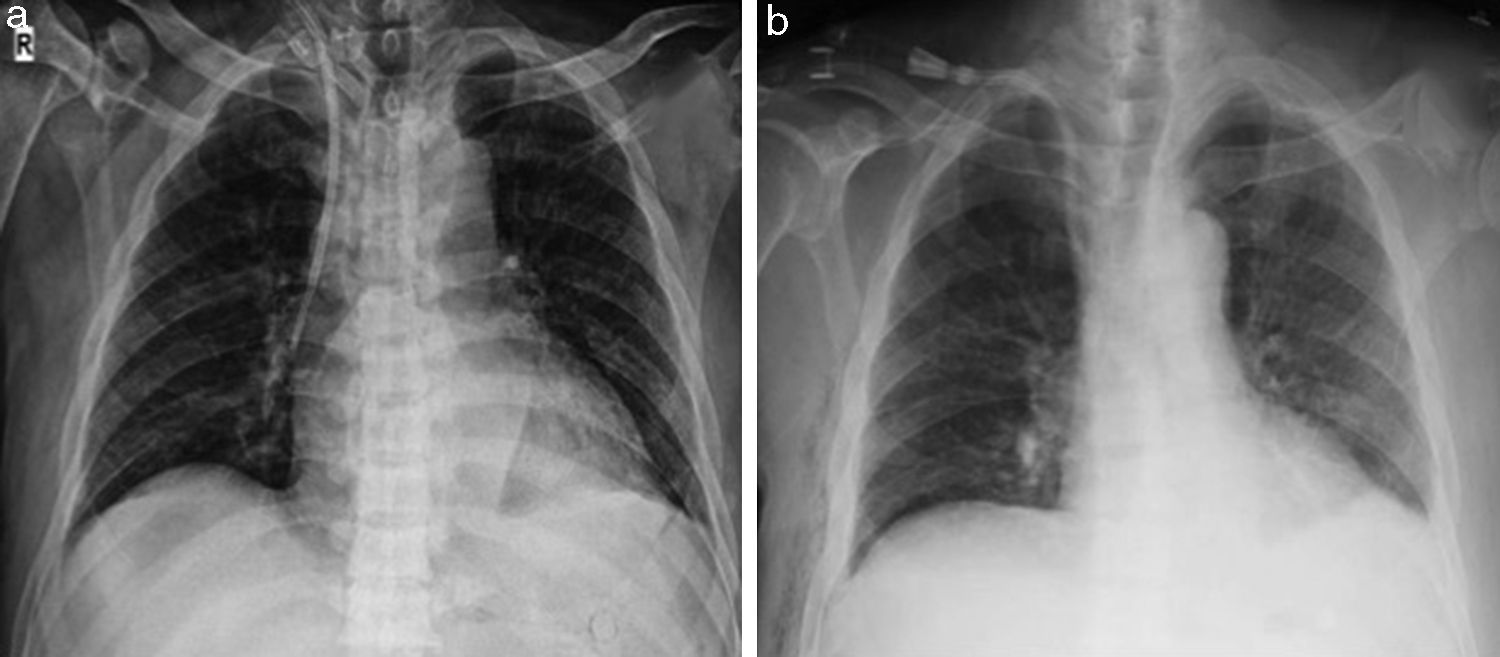
Case reportIn this article, we describe the case of a 62-year-old male patient diagnosed with renal failure who needed haemodialysis. A Mahurkar catheter was used, and the radiographic control showed that the tip of it was inside the pleural cavity (Fig. 3). This meant that there was a risk of haemothorax on removing the catheter, and the thoracic surgery department was consulted, where the patient was scheduled to have it removed with a direct view of the mediastinum using thoracoscopy.
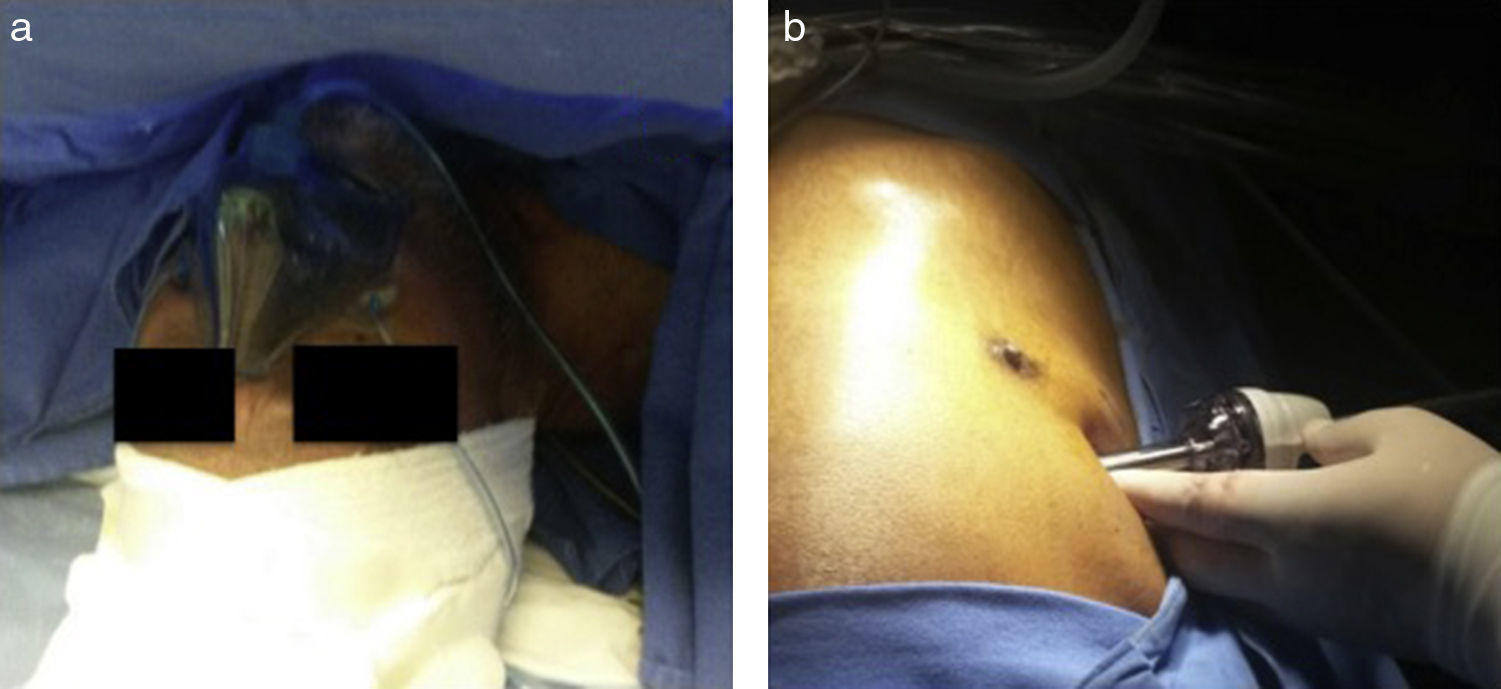
The procedure was carried out in the operating room. The patient was in a supine position, and was given an anxiolytic (midazolam 1mg), sedoanalgesia (IV remifentanil 0.12mcg/kg/min) and propofol (60–90mcg/kg/min). To control protective reflexes, IV lidocaine (1mg/kg) was administered after the patient had a coughing episode on inserting the trocar, with no new episodes during the transoperative period. Furthermore, local anaesthesia was used in the fourth, fifth and sixth intercostal spaces, each with 5ml of a solution of 9ml of 7.5% ropivacaine, 9ml of 2% xylocaine and 2ml of sodium bicarbonate.
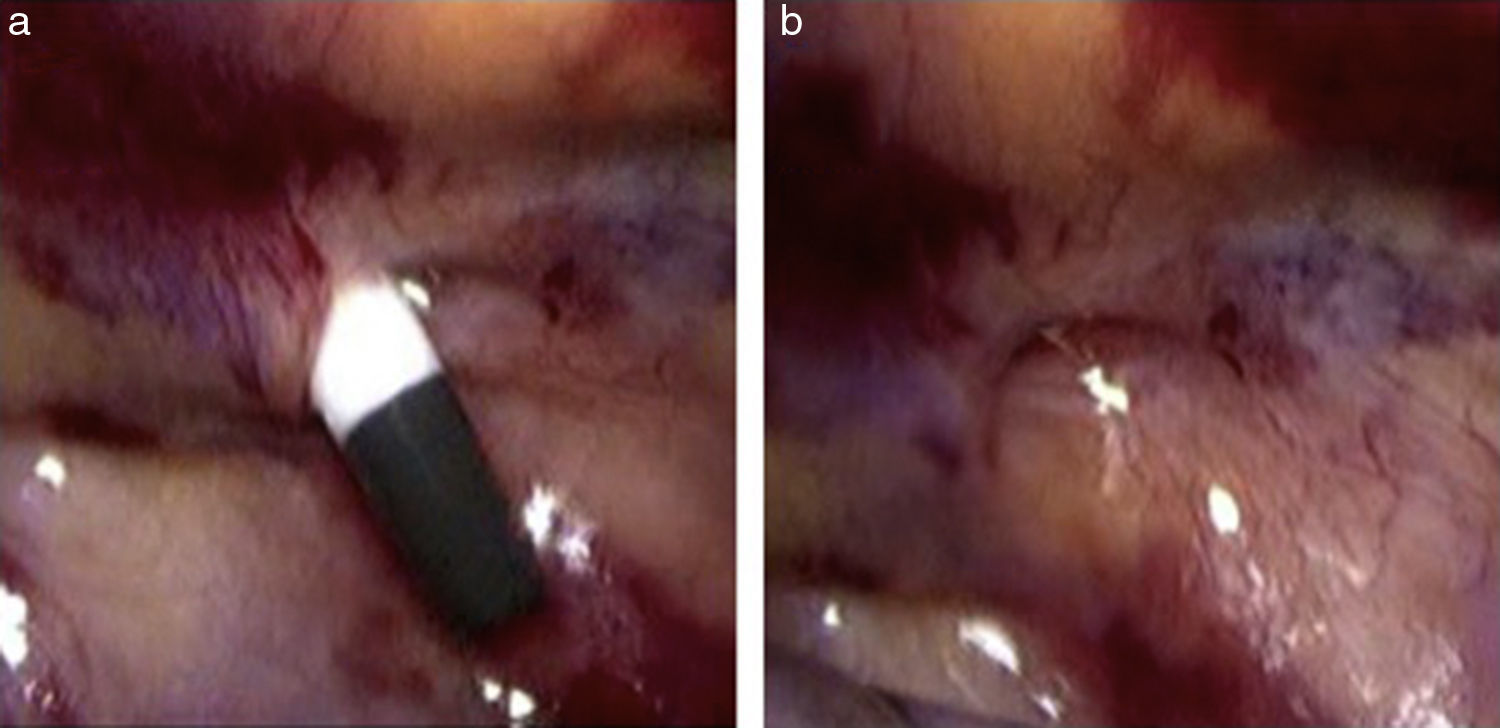
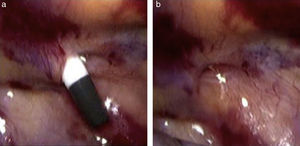
A 10mm incision was made at the fifth intercostal space, mid-axillary line, deepened by planes using blunt dissection with Kelly forceps and dissecting the intercostal muscles digitally to pierce the pleura. Subsequently, an optical trocar with a 10-mm 0-degree lens was inserted, observing inside the pleural cavity and mediastinum (Fig. 1). CO2 (8mmHg) was insufflated to deflate the lung, causing coughing immediately and subcutaneous emphysema, which was stopped with the administration of IV xylocaine, as noted above. The Mahurkar catheter was removed carefully, with no active bleeding (Fig. 2), thereby finishing the surgical procedure. The lens was removed and a thin chest tube was inserted through the trocar, placing the end of the tube into a container of water to evacuate the pneumothorax. When the bubbling stopped, the tube was removed and the wound was sutured, without a water seal. Lastly, the anaesthesiologist inserted another ultrasound-guided Mahurkar catheter, to start the haemodialysis which the patient needed.
It should be noted that the patient's spontaneous breathing was maintained at all times with a face mask with O2 at 8L per minute and FiO2 at 50% (Fig. 1). His baseline vital signs were BP 94/53mmHg, HR 87 beats per minute, BR 16 breaths per minute, O2 sat. 98% (pulse oximetry); at discharge they were BP 94/60, HR 86 beats per minute, BR 17 breaths per minute and O2 sat. 96%. We do not have baseline, transoperative or final blood gases; however, in subsequent studies we will take these into account as important variables.
DiscussionThoracoscopic procedures on non-intubated patients are technically feasible and as safe as procedures with intubation in well-selected patients. Studies have shown that it is feasible to perform thoracoscopic lobectomy in carefully selected patients in order to treat lung cancer in its early stages.1
Thoracic surgery on intubated patients is not a new idea. It was developed in the early twentieth century and was successful for many years, even in the most complex thoracic cases such as oesophagectomies, up to the development of the double-lumen endotracheal tube in the 1950s.2
Despite the new techniques, a number of patients cannot be operated on due to various comorbidities, such as elderly patients or patients with advanced respiratory disease.3
Interestingly, the most worrisome “complication” in the past, i.e. intraoperative pneumothorax, is now the main advantage when carrying out this procedure.3 Rather than being considered a medical emergency, this process is tolerated by most patients, even those with impaired lung function.3
Studies have shown that it is technically feasible to perform thoracoscopic surgery on patients without using intubation, but using internal intercostal nerve block, vagal nerve block and procedural sedation instead in mediastinal surgeries, pleural tumours and lung surgery in eligible patients.4 This is why we have introduced this type of procedure in the Thoracic Surgery and Interventional Pulmonology Department.
This patient, who had kidney disease, was at an elevated risk of bleeding on removing the Mahurkar catheter, which had to be done slowly, as well as on inserting the other catheter, a risk which would make it impossible to do haemodialysis. The catheter was withdrawn with a direct view of the mediastinum, in case haemostasis was needed, and all the necessary instruments and equipment were on hand. Another important detail is that no water seal was used, since the pneumothorax was immediately evacuated with a chest tube that was removed when the pneumothorax was stopped.
We think that by perfecting the technique used on this patient we may be able to perform other procedures, such as lung biopsies, lobectomies, sympathectomies and thymectomies, on patients without using intubation.
Conclusions- 1.
It is technically feasible to perform thoracoscopic surgery on well-selected patients without using intubation.
- 2.
By starting such procedures at centres that perform thoracic surgery, patients in whom general anaesthetic is contraindicated may be treated.
- 3.
Other procedures, such as lung biopsies, lobectomies or sympathectomies, can be performed on patients without using intubation.
- 4.
It is necessary to control coughing episodes; in our patient the administration of IV xylocaine was sufficient to achieve this.
The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo external funding was used in this case.
Conflict of interestThe authors declare that they have no conflict of interests.
We would like to thank Dr. Carlos Núñez Pérez Redondo, Head of the Pulmonology Unit, for his support for these types of procedures at Hospital General de México.