Arousal disorders (AD) are sleep disorders that primarily involve behaviour typical of being awake (e.g. talking, walking, handling objects, yelling or crying). They present during partial arousal typically during slow wave sleep (SWS). By definition it has been suggested that parasomnias do not cause changes in sleep architecture or insomnia symptoms or daytime drowsiness.
MethodA comparative and retrospective study was conducted to study the sleep architecture of a group of paediatric patients with clinical and polysomnographic diagnosis of arousal disorders (ADG), paired by age and gender with a group of healthy children (HCG). The research was conducted at the Sleep Disorders Clinic of the Faculty of Medicine of the Universidad Nacional Autónoma de Mexico. The Student's t test for independent samples was used to compare sleep architecture and a value of p<0.05 was used to determine significance.
ResultsThere was a significant increase in rapid eye movement sleep (REM) and REM sleep latency and a significant reduction in light sleep (stages N1 and N2) in the ADG compared to the (HCG).
ConclusionsIt has been reported that AD first manifests during the pre-school years and that the frequency of events gradually decreases and abate completely during adolescence, which is why AD is believed to be the manifestation of an immature central nervous system (CNS). It may be that the sleep architecture characteristics shown by patients in the ADG would correspond to CNS immaturity in healthy but younger children.
Las Parasomnias de Activación (PA) son trastornos del dormir que principalmente consisten en la presencia de conducta propia de la vigilia (por ejemplo hablar, caminar, manipular objetos, gritar o llorar) durante despertares parciales observados dentro del sueño de ondas lentas (SOL). Por definición se ha planteado que las parasomnias no provocan cambios en la arquitectura del sueño ni síntomas de insomnio o somnolencia diurna.
MétodoEs un estudio retrospectivo y comparativo, el objetivo fue estudiar la arquitectura del sueño de un grupo de pacientes pediátricos con diagnóstico clínico y polisomnográfico de parasomnias de activación (GPA), pareados por edad y sexo con un grupo de niños sanos (GNS). La investigación se llevó a cabo en la Clínica de Trastornos del Sueño de la Facultad de Medicina, de la Universidad Nacional Autónoma de México. La comparación de la arquitectura del sueño se hizo con la prueba t de Student para muestras independientes y se usó un valor de p< 0.05 para determinar la significancia.
ResultadosRespecto al GNS, en el GPA se observó un incremento significativo del sueño de movimientos oculares rápidos (SMOR) y de la latencia al sueño MOR; junto con una disminución significativa del sueño ligero (fases N1y N2).
ConclusionesSe ha descrito que la edad de inicio de las PA corresponde con la etapa pre-escolar y que la frecuencia de los eventos disminuye gradualmente hasta que remiten durante la adolescencia; por lo que se ha planteado que las PA podrían ser manifestaciones de un sistema nervioso central (SNC)inmaduro. Posiblemente las características en la arquitectura del sueño en el GPA, pueden corresponder a una inmadurez del sistema nervioso central en niños sanos, pero de menor edad.
Parasomnias are defined as sleep disorders that present during slow wave sleep (SWS) or rapid eye movement sleep (REMS), or during arousal from sleep or while falling asleep.1 They are characterised by behaviours (such as sleepwalking), physiological events (e.g., sleep wetting) or emotions (such as nightmares) and are closely related to the stages of sleep.2
The pathophysiology remains unknown, but they have been reported as a benign disorder in which there may be a CNS immaturity process; the CNS regulates the normal process of waking up from non-REM sleep.3
Parasomnias are currently divided into four groups: arousal disorders (AD), sleep-wake transition disorders, REM sleep parasomnias and other parasomnias.4
The prevalence of AD ranges from 3% to 4%, the age of onset is during childhood and most cases subside during adolescence.5
AD are partial arousals that present during SWS and therefore occur during the first half of the night.6 Some triggering factors have been reported, including fever,7 sleep deprivation and consumption of drugs, alcohol, sedatives, hypnotics8 and antihistamines, among others.9
There are three types of AD: confusional arousals, sleepwalking and sleep terrors. Even though it has been reported that there are no alterations in the macro-architecture of sleep in patients with these diagnoses,10,11 other studies have described alterations during the first sleep cycle such as low voltage EEG (electroencephalography) and electroencephalographic arousals (EA) with no behavioural correlation.12
It has also been reported that paediatric patients with AD present symptoms of insomnia such as resistance to go to bed, increased sleep onset latency and night-time arousals together with a decrease in the length of sleep13; in addition to behaviour and mood problems, learning difficulties, cognitive impairment, growth deficit and developmental deficit.14–16
Furthermore, comorbid sleep disorders may be triggering factors for AD; for example, the presence of periodic limb movement disorder or obstructive sleep apnea has been reported in paediatric patients with arousal disorders.17–19
Additionally, it has been published that the arousals occur primarily during SWS, which causes a reduction in sleep quality.20,21
As there are no conclusive data in the literature regarding the possible alterations in the sleep architecture of patients with AD, this study compared a group of children with AD (ADG) with a group of healthy children (HCG) to identify differences in sleep architecture (SA) between the groups.
MethodThis was a retrospective, cross-sectional, observational comparative study.
It included a sample of 46 children with polysomnographic diagnosis (PSG) of AD, with an average age of 11.8 years±0.51 standard error (SE), 58% male; they were compared with the HCG comprising 43 children (paired by age and gender) with an average age of 12.7 years±0.20 SE, 60% male. The pairing was stratified.
Patients in the ADG were diagnosed at the sleep disorder clinic of the Faculty of Medicine of the Universidad Nacional Autónoma de México (UNAM) between February 2009 and September 2014.
The diagnosis of parasomnias was made by doctors and psychologists certified in sleep medicine by way of a structured clinical interview, based on the diagnostic criteria for non-REM sleep arousal disorders4 as described below:
- 1.
Recurrent episodes of incomplete arousal during sleep.
- 2.
Inappropriate or lack of response to the efforts of others to interrupt or guide the person during the event.
- 3.
Associated cognition absent or oneiric imagination.
- 4.
Partial or total amnesia of the event.
- 5.
The alteration cannot be explained by another sleep disorder, mental disorder or medical condition or substance use.
Clinical diagnosis was confirmed by PSG recording with video recording.
Initially, there were 58 children in the ADG; however, due to the presence of other comorbid sleep disorders, electroencephalographic abnormalities or the presence of other types of parasomnia, 12 patients were excluded.
The HCG included family members of staff at the Sleep Disorder Clinic of the Faculty of Medicine of the UNAM. These children were reviewed by the same group of doctors and psychologists specialised in sleep medicine who evaluated the ADG children.
PSG studies were carried out according to international guidelines,22–24 starting at 10:00p.m. and ending at 06:00a.m. (±30min); they included bipolar EEG recordings (Fp1-F3, F3-C3, C3-P3, P3-O1, F7-T3, T3-T5, T5-O1, Fp2-F4, F4-C4, C4-P4, P4-O2, F8-T4, T4-T6 and T6-O2), electrooculogram (EOG), electromyography (EMG) of the chin and anterior tibialis (Grass technology safelead 48″, 72″ and 96″ electrodes), Pro-tech thermistor oronasal bridge mount, plethysmography belts for recording chest and abdominal respiratory effort (Ambu RIPmate inductance belts 26″ to 65″), microphone (Pro-tech), oximetry (Masimo oximeter multi-site sensor, Nonin 8000J 3M flexible sensor) and body position (Pro-tech). PSG recordings were performed with Alice 5 sleepware equipment version 2.8.78 (Respironics Inc., Koningjinjle, Netherlands, 1999–2010) or Cadwell systems, Easy 1 model software version 2.1 (Cadwell Industries Inc., Kennewick, USA, 1997–2004) and were visually interpreted by qualified personnel who used the current criteria established by the American Academy of Sleep Medicine.23,24
The following variables were obtained from the PSG studies: wakefulness (%), light sleep (%), slow wave sleep (%), REM sleep (%), total sleep time (%), sleep onset latency (min), N2 latency (min), N3 latency (min), REM sleep latency (min), ratio of electroencephalographic arousals (number of events/total sleep time), number of electroencephalographic arousals.
To compare the averages of continuous variables between the two groups, the Student's t test was used for independent samples and a p value <0.05 was used to determine significance. The data were analysed using the SPSS statistical package, version 19 in Spanish (IBM, SPSS Statistics, NY, USA, 2010).
Regarding ethical considerations, it should be mentioned that the anonymity of the research participants and all the children was protected, and all the children and their parents or guardians were thoroughly informed regarding the importance of participation in the study. The parents or guardians signed an informed consent form in accordance with the recommendations of the Declaration of Helsinki.25
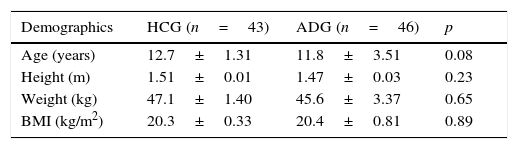
ResultsPairing between the groups was stratified; the demographic variables are shown in Table 1.
Comparison of demographic data between the group of healthy children (HCG) and the group of children with arousal parasomnias (ADG).
| Demographics | HCG (n=43) | ADG (n=46) | p |
|---|---|---|---|
| Age (years) | 12.7±1.31 | 11.8±3.51 | 0.08 |
| Height (m) | 1.51±0.01 | 1.47±0.03 | 0.23 |
| Weight (kg) | 47.1±1.40 | 45.6±3.37 | 0.65 |
| BMI (kg/m2) | 20.3±0.33 | 20.4±0.81 | 0.89 |
The data are summarised as averages±SE.
BMI: body mass index.
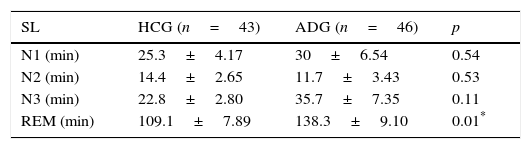
No significant differences were observed by comparing the two groups in terms of sleep onset latency (p<0.54), N2 latency (p<0.53) or SWS latency (p<0.11). However, there was a significant increase identified in the ADG for REM sleep latency (p<0.01) compared to the HCG; see Table 2.
Comparison of sleep latency between the group of healthy children (HCG) and the group of children with arousal disorders (ADG).
| SL | HCG (n=43) | ADG (n=46) | p |
|---|---|---|---|
| N1 (min) | 25.3±4.17 | 30±6.54 | 0.54 |
| N2 (min) | 14.4±2.65 | 11.7±3.43 | 0.53 |
| N3 (min) | 22.8±2.80 | 35.7±7.35 | 0.11 |
| REM (min) | 109.1±7.89 | 138.3±9.10 | 0.01* |
The data are summarised as averages±SE.
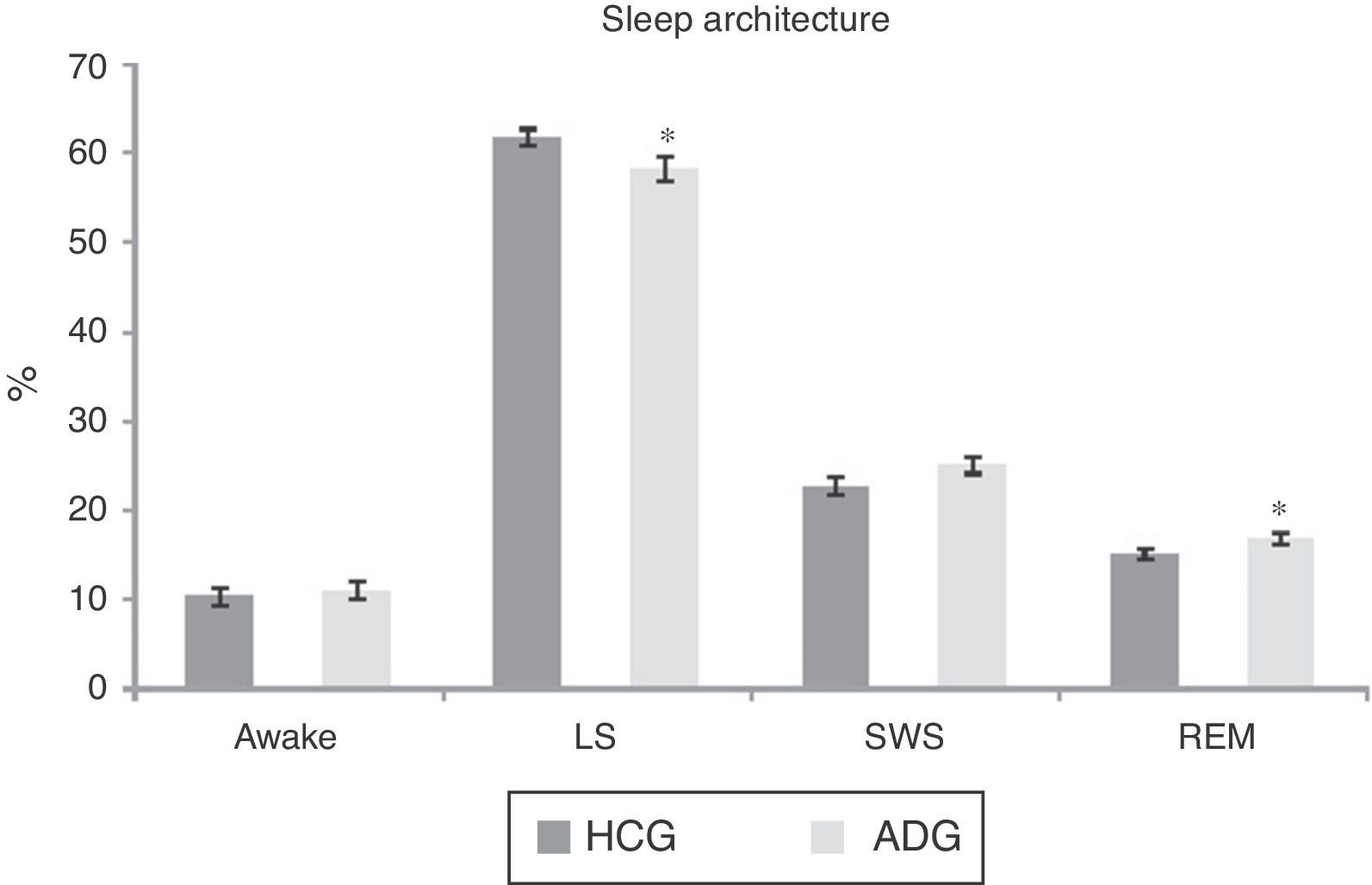
In terms of sleep architecture, there were no significant differences between the HCG and the ADG regarding the percentage of wakefulness (p<0.60) or SWS (p<0.08). However, a significant decrease was seen in LS (p<0.04) and a significant increase in the percentage of REM sleep (p<0.03) compared to the HCG; see Fig. 1.
To conclude, no significant differences were observed in the ADG by comparing total sleep time (p<0.97), number of electroencephalographic arousals (p<0.35) or the ratio of electroencephalographic arousals (p<0.49), compared to the HCG.
DiscussionThe general aim of this research was to compare sleep architecture between the HCG and the ADG; an increase in the percentage of REM and a decrease in LS (both significant) were found in the ADG.
It should be mentioned in relation to these findings that the decrease in REM and SWS, together with an increase in LS, are expected changes as part of CNS maturity, due to the ontogeny of sleep.26
It has also been described that AD remit spontaneously during adolescence, and they have therefore been proposed as sleep disorders caused by CNS immaturity.27,28
Based on the above, it could be said that the changes in sleep architecture identified in the ADG may be indicators of the above described immaturity. This hypothesis requires more in-depth research in the future.
Moreover, the changes found in sleep architecture also provide information in terms of the nature of AD as, by definition, these disorders do not cause alterations in the length of sleep stages,10,29 but we did find these changes in our results by comparing patients with the HCG.
After almost forty years classifying different sleep disorders, more research still needs to be done in terms of parasomnias.
Suggestions and limitations of the studyOne of the limitations of this study was the small number of participants studied; in future research, the number of patients studied must be increased.
Of the entire ADG sample, 3% of the patients were on prescription medication for epilepsy, depression or attention deficit hyperactivity disorder. In future studies, these pharmacological factors must be excluded.
No patients with comorbid sleep disorders were included in this study (such as sleep-related breathing disorders or periodic limb movement disorder). In future research, patients with comorbid sleep disorders will be included in order to determine specific treatment regimens.
Another line of research to be examined is the cyclic alternating pattern (CAP), which is an indicator of sleep stability that should also be studied to better understand the nature of AD.
ConclusionsCompared to the HCG, it was identified that in the ADG there were an increase in REM latency and the percentage of REM, as well as a decrease in LS. There are changes in sleep architecture that may be a result of the CNS immaturity that has been described in patients with non-REM sleep parasomnias.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that they have no conflicts of interest.
The authors would like to thank Daniel Santana, Adrián Poblano and Rafael Santana for their comments on the manuscript, and Iván Miranda and Mauricio Ruíz for their invaluable collaboration.