Specific anal ulcers occur in 11% of patients with anorectal disease. Of these, 35% present immunodeficiency with a CD4 count <500. This type of anal ulcer coexists mainly in patients who are anoreceptive, HIV positive, with haematological disorders or anal carcinoma.
ObjectiveTo determine the anal ulcer healing rate in immunocompromised patients using the three-drug regimen and/or anal ulcer excision biopsy if the first treatment fails.
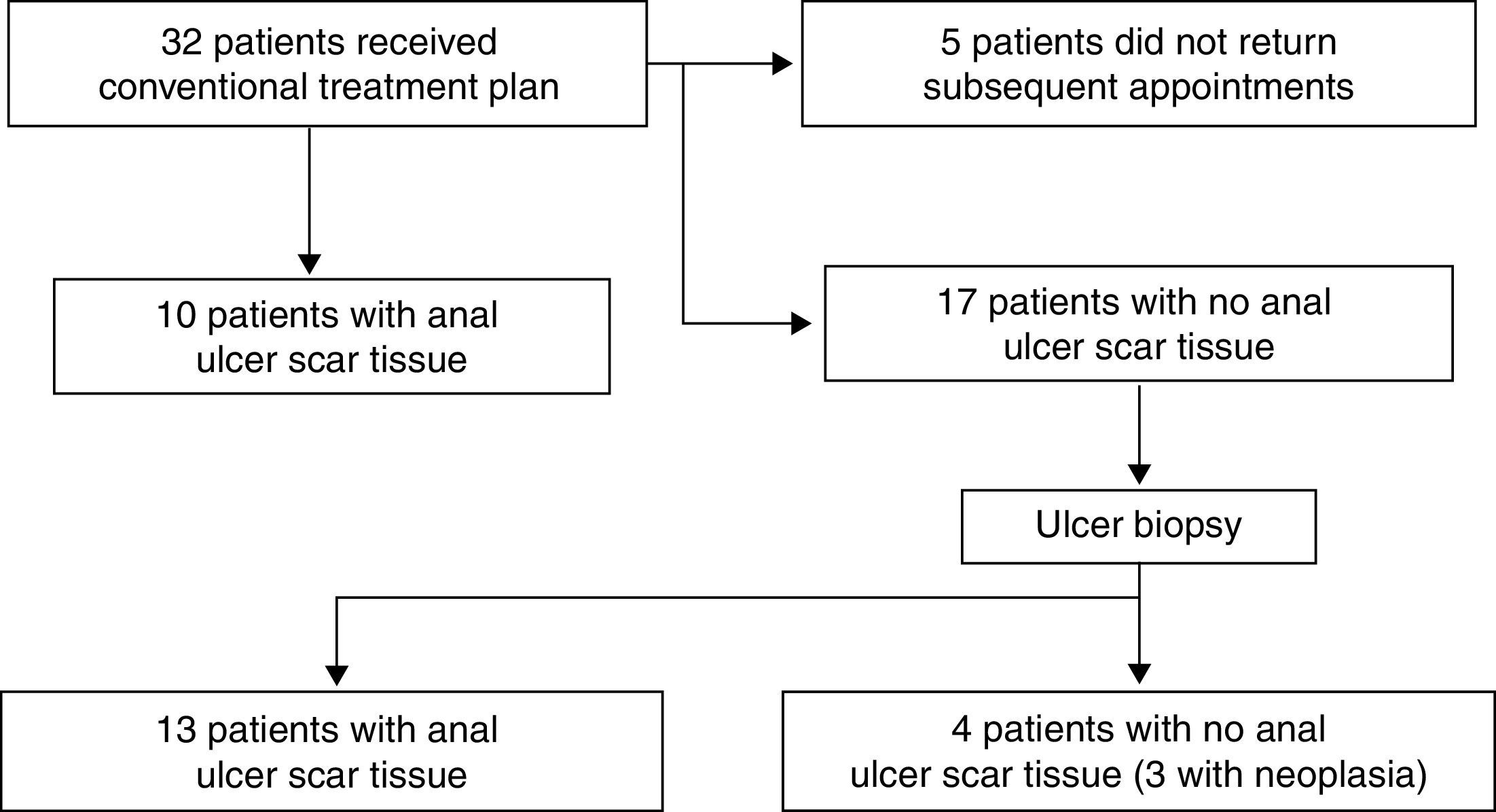
Materials and methodsA prospective cohort study was conducted in 32 immunocompromised patients with specific anal ulcer diagnosis. They were evaluated from January 2013 to December 2013 in the Colorectal Unit of the Hospital General de México. Patients with atypical anal ulcer were treated according to the conventional three-drug regimen: single dose of IM ceftriaxone 1g, single dose of oral azithromycin 1g and a 14-day course of oral acyclovir 400mg every 6h.
Patients who did not respond as expected to the three-drug regimen were submitted to anal ulcer excision biopsy under anaesthesia. A complete anal ulcer biopsy was taken and sent to pathologist for study. The cohort was followed up for four weeks to assess healing. Though, patients who did not heal beyond this time were given a total of 6 months of follow up.
ResultsHealing occurred in 33% of patients who were administered the three-drug regimen. Of those patients who underwent anal biopsy, 77% had healed at 4 weeks. Those patients that did not heal had a baseline CD4 count <250.
ConclusionsThe cure rate for anal ulcer using the three-drug regimen is 33%, and 77% after excision biopsy.
La úlcera anal específica se presenta en 11% de los pacientes con patología anorectal; donde 35% presentan inmunucompromiso con recuento CD4<500; siendo más frecuente en anoreceptores, VIH seropositivos, trastornos hematológicos y carcinomas anales.
ObjetivosDeterminar el porcentaje de cicatrización de las ulceras anales en los pacientes inmunocomprometidos con triple esquema y/ó luego de biopsia escisional de la úlcera anal si hubo falla en el primer tratamiento.
Materiales y MétodosEstudio prospectivo tipo cohorte con 32 pacientes inmunocomprometidos y con diagnóstico de úlcera anal específica de enero de 2013 a diciembre de 2013, en la Unidad de Coloproctologia del Hospital General de México. El esquema convencional de triple droga utilizado para el tratamiento de la úlcera anal atípica emplea dosis única de Ceftriaxona 1 gramo IM y Azitromicina 1 gramo VO, además Aciclovir 400mg VO c/6hrs por 14 días.
Quienes presentaron resultado desfavorable de cicatrización de la úlcera anal con tratamiento de triple droga fueron candidatos para exploración bajo anestesia con biopsia escisional de la úlcera anal. Se tomó biopsia completa de la úlcera anal y se envió a estudio con el patólogo. Se estableció cuatro semanas como cohorte para evaluar cicatrización en estos pacientes. Prolongamos el cohorte del tiempo de seguimiento hasta 6 meses en los pacientes que no presentaron cicatrización luego de biopsia excisional de la úlcera anal.
ResultadosLos casos bajo tratamiento con triple droga el 33% obtuvieron una respuesta favourable a cicatrización. Los sometidos a biopsia anal el 77% presentaron cicatrización a las 4 semanas. De los últimos que no cicatrizaron tenían inicialmente recuento de CD4<250.
ConclusionesEl porcentaje de cicatrización de úlceras anales con esquema de triple droga es de 33% y al realizar biopsia escisión es de 77%.
Typically, 90% of perianal ulcers in both men and women have a posterior midline location. Anterior fissures occur in 10% of patients, being more common in women. Less than 1% of fissures is outside the posterior midline location or may be multiple. These atypical fissures can be associated with Crohn's disease, sexually transmitted disease (STD), HIV, syphilis, herpes, tuberculosis or anal cancer.2 Mycotic lesions, though uncommon, can be related to histoplasmosis. Candida may cause secondary contamination of lesions of another origin. With respect to tumours, it is common to find the presence of AIDS related tumours: Kaposi's sarcoma or non-Hodgkin lymphoma. A growing incidence of anal epidermoid or squamous cell carcinoma is described in this population, though it is not found among AIDS-related tumours.10
Anal ulcers are a frequent finding that represent 10–15% of anal pathologies in immunocompromised patients. More than half of these cases are due to herpes simplex (HSV). Secondly, ulcers may be found that are associated with CMV, TB and Syphilis, among the most common, and to a lesser extent ulcers of a pre-malignant or malignant nature. Finally, idiopathic ulcers may present in the anal area and are usually deep and disabling. Cytological examination or skin biopsy of the external portion of the lesions will allow diagnosis.15
6–34% of patients infected with the human immunodeficiency virus (HIV) have associated perianal disease, of which 50–85% requires surgery. In other cases the cause is not defined and it is determined to be idiopathic.1 Anal ulcers of idiopathic origin in patients with HIV are characterised by being very painful and the majority present purulent discharge. It is believed, as mentioned by Denis et al., that these ulcers have the same cryptoglandular origin as anal abscesses.7
The theory recently emerged of the existence of viral synergism with cytokine production, which can result in the destruction of tissue and the formation of deep and invasive anal ulcers that can destroy the internal/external anal sphincter or even affect the ischioanal fossa. There is another presentation in which there are two or more ulcers, which are not so invasive and may reach no further than the dentate line; it is probable that these two presentations have a different physiopathology and aetiology. However, more studies are required in order to establish the aetiology and physiopathology and thus provide the correct treatment of anal ulcers to the HIV-positive patient.16
It is considered that according to previous reports referring to cicatrisation and related to the reduction in CD4 values, patients with AIDS present a poor prognosis with respect to the more aggressive treatments.6
A cohort study showed that the lower the CD4+ levels are in HIV patients, the greater the prevalence of HPV, and consequently a greater prevalence of anal dysplasia. It is thus considered that a high CD4 count is a protective factor against opportunistic viral infections.21
Approximately 50% of anal ulcers have no identifiable aetiological agent. Some believe that these idiopathic ulcers may be caused by HIV itself. No optimum treatment for these types of idiopathic ulcer is known, but various options exist. First, conservative treatment with hip baths and local treatment, considering simultaneous treatment with aciclovir and metronidazole. Surgery should be considered in cases of persistent symptomatic lesions. Although in these patients cicatrisation is usually slow, the asymptomatic relief is often dramatic.11
Although no universally accepted treatment exists yet, some authors recommend medical treatment, others recommend the injection of steroids into the lesions and others choose surgery when there is no response to the symptoms or when medical treatment has failed.1
Immunological improvements exist in HIV patients treated with highly active antiretroviral therapy (HAART). This includes protease and transcriptase inhibitors. The viral load is reduced in HIV patients and the T lymphocytes CD4+ increase, thus improving their life expectancy. However, since they live with immunosuppression for long periods, they are vulnerable to opportunistic infections.16
On the one hand, the effect of HAART may restore immunity and reduce the incidence of dysplasia associated with HPV. However, increasing the life expectancy of patients with HIV can result in the development of slow carcinogenic processes. However, more epidemiological studies are needed to clarify this aspect.20
The idiopathic anal ulcer in the immunocompromised adult is a disease that is seen increasingly in the Coloproctology Unit of the Hospital General de México. There are currently no studies in this respect in Mexico and in our institution.
The conventional treatment plan used for anal ulcers in immunocompromised patients in the Coloproctology Unit and which empirically continues to be used is not supported by a study that allows us to determine the effectiveness of the treatment.
At the same time we wanted to determine the rate of cicatrisation of anal ulcers in these immunocompromised patients after the combined use of the conventional treatment and a biopsy under sedation in those who did not respond to initial treatment.
Materials and methodsA prospective, cross-sectional, observational study was conducted. The study was based on 32 immunocompromised patients diagnosed with an atypical anal ulcer in the period from January 2013 to December 2013, in the Coloproctology Unit of the Hospital General de México. The characteristics taken into account to discern between typical and atypical anal ulcers, was that the latter must present chronicity data, be an excavated lesion with prominent edges without epithelialization and be located outside the midline.
Patients with a diagnosis of atypical anal ulcer, assessed at an external centre or who were referred to us due to symptoms of anal pain and/or pruritus.
The conventional treatment plan that we use in our Coloproctology Unit involves the use of ceftriaxone 1g IM or IV single dose, azithromycin 1g single dose orally and aciclovir 400mg orally every 6h for 14 days.
Patients who presented a negative result for the cicatrisation of the anal ulcer with triple drug treatment were candidates for an examination under anaesthesia with excisional biopsy of the anal ulcer. This was performed in ambulatory surgery under sedation and local anaesthesia. Simple lidocaine is used with bicarbonate 20 ml: 3 ml, and the patients are placed in the jack-knife position. A complete biopsy of the anal ulcer was taken and sent to pathology for subsequent analysis.
The time needed to evaluate whether or not the anal ulcer in patients subjected to an excisional biopsy had completely healed was standardised at four weeks. The follow-up period of the cohort was extended up to 6 months in patients who did not show healing after the excisional biopsy of the anal ulcer.
Statistical analysisThe information obtained was processed in Word XP format. Part of the statistical analysis employed the Chi-squared test using the SPSS programme. P<0.05 was taken as statistically significant.
ResultsOf the 32 patients, 28 were male (87.5%) and 4 female (12.5%). The predominant age group was 31–40 (34%). The most common origin was Distrito Federal with 20 patients (62.5%).
Of the patients who presented for the first time, half presented with symptoms for less than 1 month, the most common being anal pain and tenesmus.
Within the most frequent types of immunocompromised patient, 21 were HIV-positive patients (65.5%), of which 4 had AIDS. 3 patients had leukaemia (9%), 1 (3.5%) had systemic lupus erythematosus, 1 (3.5%) had nephropathy and 6 (18.5%) were not immunocompromised. Other sexually transmitted diseases that were found to be associated at the time of diagnosis of the perianal ulcer was Human Papilloma Virus in 6 patients (18.75%), 1 patient (3.12%) with Herpes Simplex, 1 patient (3.12%) with tuberculosis and 1 patient (3.12%) with gonorrhoea. We found that of the HIV carriers, 12 (85.7%) had already received treatment with Atripla. Of this group, those under 30 years of age presented an Ro of 7 (CI 95% for 3.8–8.0) for sexually transmitted disease.
Of the reactive HIV patients, 17 (81%) had a CD4+ count ≥250 and 4 (19%) a CD4+ ≤250. Of the total number of HIV and/or AIDS carriers (n=21), 11 (52%) patients presented an undetectable viral load, the rest being detectable.
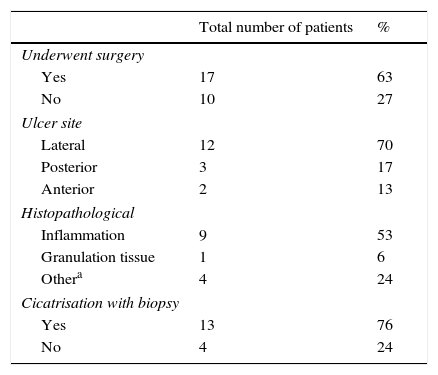
An examination under anaesthesia was performed and a biopsy taken on 18 (56%) of the total patients in the study. Patients were subjected to this procedure when, after conventional treatment, there was no improvement in the cicatrisation of the anal ulcer. Of the patients subjected to surgery, the ulcer was found to be perianal in 10 (58%) and in 7 patients (42%) it was found to be in the anal passage. Within the transoperative findings, 3 cases were observed (anal fistula, abscessed anal fistula and anal condylomas). The location of the anal ulcer was variable; however, its most common location was in the lateral and posterior region (Fig. 1).
Cultures of the discharge were taken together with the biopsy under sedation. Escherichia coli was found in 25% and Streptococcus sp in 8%. Contamination was reported in the rest of the samples sent. The most frequent histopathological result was acute and chronic inflammation in 13 (76%) patients, 1 patient presented non-Hodgkin lymphoma, 1 patient presented Kaposi's sarcoma and 1 patient presented epidermoid carcinoma. Of the 10 patients subjected to an AFB test with biopsied tissue, only 1 was positive (10%).
The 32 patients were indicated treatment according to the conventional treatment plan of this unit (CTP). There was only a notable improvement in the cicatrisation of the anal ulcer in 9 (28%) patients, 18 (56%) presented no improvement and 5 patients (4%) abandoned the treatment but did not attend their subsequent appointment. In the postoperative stage of the patients who received the CTP, 14 (77%) presented cicatrisation of the wounds and 4 (23%) presented no cicatrisation, the latter presented CD4+<250 (Table 1).
Results of anal biopsies.
| Total number of patients | % | |
|---|---|---|
| Underwent surgery | ||
| Yes | 17 | 63 |
| No | 10 | 27 |
| Ulcer site | ||
| Lateral | 12 | 70 |
| Posterior | 3 | 17 |
| Anterior | 2 | 13 |
| Histopathological | ||
| Inflammation | 9 | 53 |
| Granulation tissue | 1 | 6 |
| Othera | 4 | 24 |
| Cicatrisation with biopsy | ||
| Yes | 13 | 76 |
| No | 4 | 24 |
Only 1 patient (5.88%) of the postoperative group presented a complication: an infection at the surgery site which was treated with antibiotics. Of the 32 patients, 5 did not attend the subsequent appointments after the start of treatment. 4 weeks were established as the standard time to assess whether or not there was complete cicatrisation in the patients subjected to biopsy of the anal ulcer. We found that of the postoperative patients, only 6 attended their subsequent appointments 3 months after surgery. It was the 4 patients (1.48%) with CD4+<250 and AIDS who did not present cicatrisation after the excisional biopsy of the anal ulcer at the end of 6 months of follow-up.
DiscussionMore than 50% of the patients underwent surgery after having received treatment with the CTP according to Nadal et al., 6–34% of the patients infected with the human immunodeficiency virus (HIV) has associated perianal disease, of which 50–85% requires surgery.1 The most common location of the perianal ulcer was posterior and lateral, and Mallari et al found in a study with 58 HIV patients with anal fissures, that the most common location was posterior in 47 patients, anterior in 7 patients and posterior plus anterior in 4 patients.17
In our population, more than 80% of patients with a diagnosis of HIV were already receiving treatment with Atripla. As expected, the most common sexually transmitted disease is HPV and it is most frequently found in patients ≤30 years of age. According to Greebon et al., in young patients with HIV there is a higher prevalence of HPV and thus a higher prevalence of anal dysplasia.21
We observed that a favourable factor for better cicatrisation presented in reactive HIV patients with CD4+≥250. According to a cohort study, Nadal et al. asserted that a high CD4 count is a protective factor against opportunistic viral infections.1 Similarly, for the majority of our patients the viral load was undetectable. Laurent Abramowitz et al. reported that immunological improvements exist in HIV patients treated with highly active antiretroviral therapy (HAART): reducing the viral load and increasing T lymphocytes CD4+.16
We used a conventional treatment plan with aciclovir for 14 days, ceftriaxone and azithromycin in monodose, with which we obtained cicatrisation results in a third of the cases. However, when performing the biopsy on said ulcer the response to medical treatment was not favourable, obtaining cicatrisation results in 77% of patients.
The most common microorganism found in the discharge cultures was E. coli, which is explained by the anatomical location and thus the high probability of contamination that exists when taking the sample. Meanwhile, the most common histopathological finding was acute and chronic inflammation (76% of cases). This, in particular, explains why no specific causal agent is found in the majority of studies. This is the case with the case of Cello et al., where approximately 50% of anal ulcers have no identifiable etiological agent. Some believe that these idiopathic ulcers may be caused by HIV itself.
We found 1 patient with non-Hodgkin lymphoma, 1 patient with Kaposi's Sarcoma and 1 patient with Epidermoid Carcinoma. This is in agreement with a comparative and retrospective study by Nadal et al., in which the patients who were studied for perianal ulcers and in whom a tumour was found in the histopathological study, were most frequently HIV-positive patients compared to HIV-negative patients. The most frequent tumours being Kaposi's Sarcoma and Epidermoid Cancer. It was also found that the non-Hodgkin lymphomas are considered common in the perianal region in HIV-positive patients.7
ConclusionsBased on the results obtained, we note that the use of the conventional treatment plan together with a biopsy of the anal ulcer in patients who did not adequately respond at first, present cicatrisation in 77% of cases. The incidence of neoplastic lesions is 17%, which suggests that special attention must be paid in these patients to achieve early detection and the appropriate treatment.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.