Down syndrome (DS) is a chromosomal disorder with variable phenotypic expression, although different patients share some common features. Among them, hypotonia, ligament laxity and delayed psychomotor development stand out. These traits can improve with early therapy, but remain as gait instability and pathologic compensatory strategies in adult patients.
Pathological gait in DS patients has been studied previously, but the treatment of motor problems has not been approached from a neurological rehabilitation viewpoint, focused on quality of function.
ObjectivesThe aim of this study was to describe the gait alterations in a sample of patients with DS and to assess changes after Bobath physiotherapy.
Material and methodsAn experimental prospective uncontrolled study was performed. Ten adults with DS (mean age: 28 years) were assessed at baseline and after 10 sessions of Bobath physiotherapy treatment. Quantitative data (such as step length or walking speed) and qualitative data (such as characteristics of arm movements and instability) were recorded by an evaluator blinded to the treatment received.
ResultsClear deviations with respect to normal adult gait were found, and a trend towards improvement after physiotherapy treatment. The results were significant in the correction of pitch angle and its symmetry.
The study has revealed the potential benefits of physiotherapy in adults with DS and the need to complete more studies in this sense.
El síndrome de Down (SD) es un trastorno cromosómico de expresión fenotípica variable, aunque con rasgos comunes en los distintos pacientes. Entre ellos, destaca la hipotonía, hiperlaxitud ligamentosa y el retraso en el desarrollo psicomotor. Estos rasgos mejoran con la terapia temprana, pero persisten en forma de inestabilidad de la marcha y compensaciones patológicas en el adulto.
La marcha patológica en estos pacientes ha sido objeto de estudios previos, pero el tratamiento de los problemas motores no ha sido abordado desde un enfoque neurorrehabilitador, dirigido a la calidad del funcionamiento.
ObjetivosEl propósito del presente estudio es describir las alteraciones de la marcha en una muestra de pacientes con SD y evaluar los cambios después del tratamiento con fisioterapia Bobath.
Material y métodosEstudio prospectivo experimental de tipo ensayo no controlado. Diez personas adultas con SD (edad media: 28 años) fueron evaluadas en situación basal y después de 10 sesiones de fisioterapia Bobath. Se recogieron variables cuantitativas (como longitud del paso, velocidad de la marcha) y variables cualitativas (como calidad del braceo o inestabilidad) a través de un evaluador ciego al tratamiento fisioterápico.
ResultadosSe encontraron claras desviaciones respecto a la marcha adulta normal y una tendencia a la mejoría después del tratamiento fisioterápico. Esta mejoría fue significativa en la corrección del ángulo y en la simetría del paso.
Se pone de manifiesto el potencial beneficio de la fisioterapia en adultos con SD y alteraciones de la marcha, así como la necesidad de realizar más estudios en este sentido.
Down syndrome (DS) is a genetic-based disorder having variable phenotype expression in different individuals. In spite of that, there are shared clinical manifestations (specific physiognomy, cognitive disabilities that vary in degree, hypermobility, muscular hypotonia, and growth delay).
Individuals with DS frequently suffer from motor disability, which includes slowness of movements and reaction times, as well and posture and balance problems. Delayed motor development is linked to the muscular hypotonia and ligament mobility, although neuropathological alterations (such as cerebellar dysfunction, delay in myelination or proprioceptive and vestibular deficits) can also have an effect.1,2 The presence of rigidity and early joint deterioration is typical in these individuals as well. All of this contributes to the presence of gait and balance disorders from infancy that lasts till adulthood.
Over the past several years, several studies on and descriptions of gait biomechanics in children and adults with DS have been published.2–7 Various interventions to help the motor problems of these individuals have also been reported, based on physical training in strength or resistance.8–13 In 2011, Mendonza et al.13 compared the effects of aerobic training and resistance exercises in adults with and without DS, demonstrating similar benefits for the patients with DS and the control individuals. That study also revealed improvements in walking economy after the intervention, with qualitative benefits, not only quantitative ones. Nevertheless, the physiotherapeutic approach aimed at improving gait quality in adults with DS is a relatively undocumented matter at present.
Among the different physiotherapy methods, the Bobath concept is based on taking advantage of plastic neurological changes to achieve normal movement, which leads to optimal function. This treatment type has demonstrated its efficacy in clinical practice in patients with movement alterations caused by a neurological disease and has been used successfully in children with DS.14–16
Based on these data, this study was set up with the goal of identifying the pathological features of walking in 10 adults with DS and assessing potential benefits of treatment using Bobath physiotherapy.
Material and methodsA prospective, evaluator-blinded uncontrolled experimental study was performed. The sample consisted of 10 patients with DS, aged between 22 and 39 years, with autonomous walking. The patients lacked any other disorder that might interfere in movement and gait (whether permanently or temporarily). The patients participated in the Down Syndrome Foundation's Sports Section in Madrid (Spain) and were selected consecutively, when they voluntarily offered consent or by their legal guardian.
Each patient's basal posture and gait (pre-treatment) was assessed individually as follows:
- -
Assessment of standing posture. The patient was asked to walk a few steps away and then return and stop in front of the camera with comfortable straight, natural posture. No corrections were made to the subject's posture so that the image would faithfully reflect his or her body schema. The subjects were asked to remain still and front, back and right and left side photographs were taken, moving the camera around the patient.
- -
Gait assessment:
- •
Measurement of gait descriptors. Walking speed and cadence were measured in an open, flat-level space. To do so, the patient was asked to walk for 22m at a comfortable speed, the central 10m were timed, and the steps in those 10m were counted.
- •
Video documentation of walking. The central 10m of a 22-m route were recorded, avoiding the el effect of acceleration and deceleration at the beginning and end of walking, respectively. Various shots were taken: frontal plane (from the front and the back) and sagittal plane (right lateral and left lateral).
- •
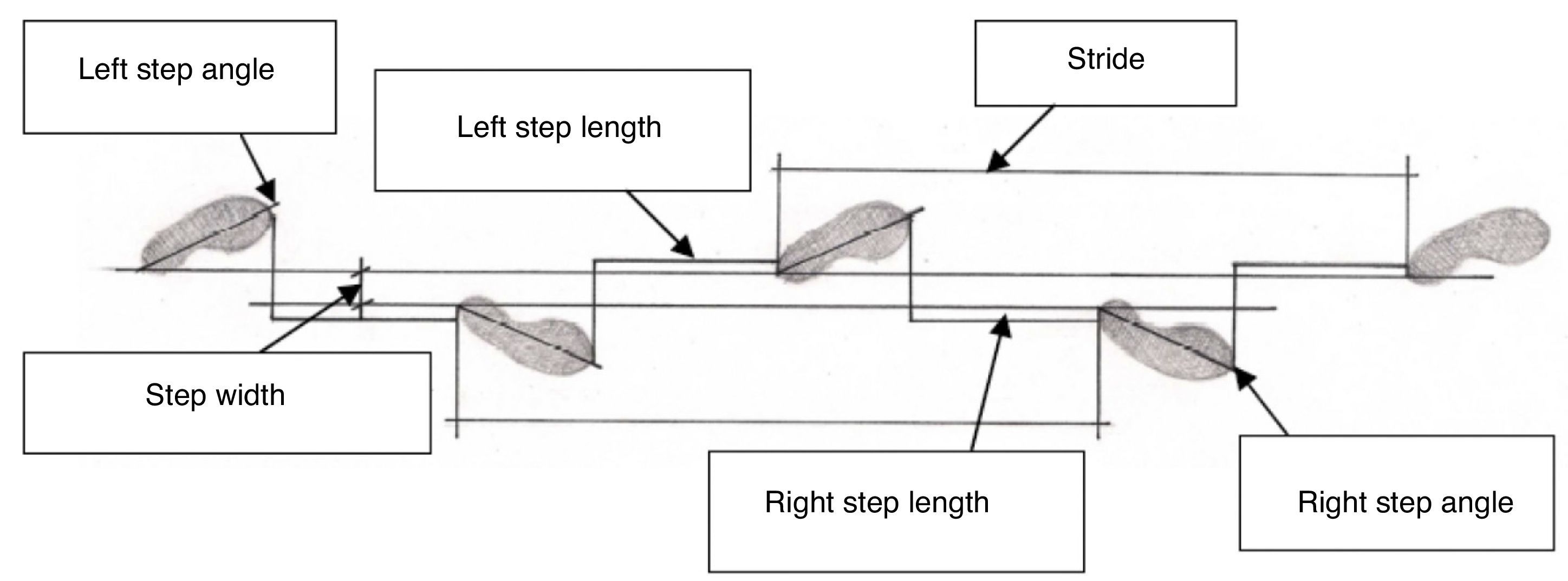
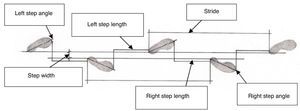
Analysis of the impression of footprints while walking. Each patient was asked to walk over a homogeneous surface with the soles of his or her shoes rubbed with chalk. The route was 22m long, at a free cadence. Five consecutive footprints from the central steps were measured, registering step width, step length, step angle and stride length (Fig. 1).
- •
After the baseline session, each patient received 10 Bobath physiotherapy sessions, 1 session a week. Further details are given later in the article.
Finally, the assessment tests that had been performed at the baseline registry were repeated for a comparative study. The following data were obtained for each patient (pre- and post-treatment):
- -
Posture (correct/incorrect, description).
- -
Speed (m/s).
- -
Cadence (number of steps/min).
- -
Arm swing in counterphase (presence/absence, normal/abnormal, description).
- -
Score for the “eight qualitative analysis criteria for gait”,17 according to four ratings, from 0 (excellent, no alteration) to 3 (markedly altered gait):
- •
General body attitude while walking.
- •
Variability in the manner of walking and in the progression.
- •
Important losses of balance.
- •
Decision in heel contact.
- •
Hip extension observable while walking.
- •
Synchronism between the upper and lower limbs.
- •
Distance between the feet on the ground.
- •
Duration of double support.
- •
Cycle or stride length: distance between two ground contacts of the same foot.
- •
Step length: distance between the support foot toe and the heel of the moving foot that contacts the ground.
- •
Step width: separation between the heels.
- •
Step angle: rotation of the foot at the moment that it contacts the ground.
- •
An evaluator randomly analysed the photographs and gait video recordings. The evaluator was a physiotherapist with experience in neurological disorders and treatment. He was blinded to whether the posture or walking being evaluated was pre- or post-treatment. Afterwards, the results were ordered in tables, based on the chronological moment in which the posture/walking register had been performed.
Physiotherapeutic treatmentTreatment was based on a series of therapeutic strategies found within the Bobath concept. These strategies were applied in combination to each patient according to her or his individual needs and were adapted to each specific case. The strategies were the following:
- -
Obtain appropriate muscle length and joint alignment.
- -
Avoid compensation.
- -
Modulate tone.
- -
Facilitate normal movement components.
- -
Provide posture stability and control.
- -
Awaken balance and righting reactions.
- -
Repeat without repeating (variability of movement).
- -
Practice specific tasks.
The procedure for each patient was as follows: Alienation of the key points and the interaction of the subject's support base with gravity in various postures (decubitus, sitting, standing on both feet, standing on 1 foot, stepping position, etc.) were assessed. Attempts were made to align the musculoskeletal system properly, modifying muscle length and amplitude to modify muscle shortening and hypertonia (which in turn favour better alignment and, consequently, more effective muscular activation). Afterwards, movement and its components were facilitated actively and functionally. Lastly, motor skills were practiced; specifically, walking in the context of aiming at an objective (the task of walking around was practiced in contexts that were significant to the patients).
Standard valuesFor the qualitative gait variables, the standard was represented by a score of 0 on the scale used, both for each of the items and for the total score.17 The scale established scores corresponding to acceptable, poor or very poor results.
Posture and arm swinging were assessed as normal or abnormal. Deviations from the standard were described in detail, according to the blinded physiotherapist evaluator's criteria.
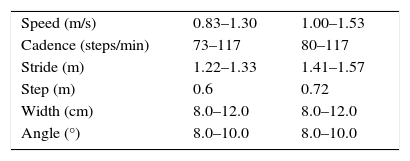
To obtain the quantitative standard values, we took into account different sources, that in turn gathered references obtained by various authors.17,18 The standard values chosen for comparison with our data were the ranges of extreme values observed by the set of the authors consulted; differentiated parameters were established for males and females. Table 1 shows the standard reference values used in this study.
Statistical analysisThe statistical analysis was carried out with the SPSS program. We chose a repeated measures analysis of variance (ANOVA) model. This allowed us to analyse two measurements from the same subject (pre- and post-treatment) and consequently analyse the possible effect of an intervening factor.
ResultsTen patients with DS, with a moderate degree of disability, participated in the study: 8 men and 2 women. They were from 22 to 39 years old, with a mean age of 28 years. All patients walked independently and did sports regularly, and they continued doing so during the development of the study.
In the pre-treatment assessment, in 100% of the cases, there were many variables evaluated that did not correspond with the standard reference values. In the post-treatment assessment, some of these variables were modified, although not always significantly (Tables 2 and 3), as indicated below.
- -
Cycle length. In the baseline situation, all the patients had lower cycle lengths than the standard values. Following treatment, 70% of the patients improved, especially the females.
- -
Speed. In the baseline evaluation, 90% of the patients had a faster speed than normal. After treatment, speed continued to be higher, without statistically significant changes.
- -
Cadence. The patients also had a higher cadence than expected at baseline. Following treatment, the cadence did not normalise. In fact, it even increased slightly in the men, without statistically significant changes.
- -
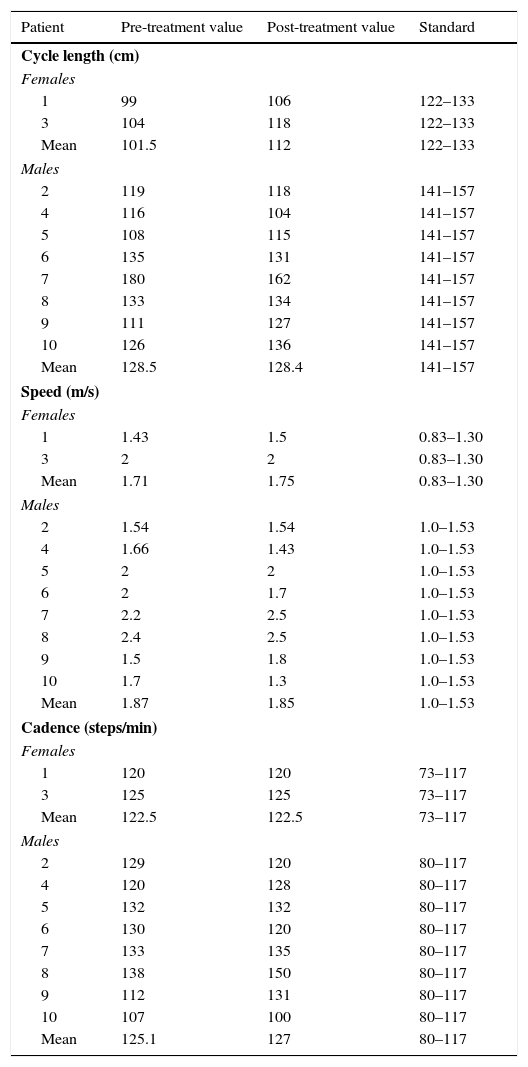
Symmetry of step. In 80% of the cases, the baseline difference between one step and the other was greater than 0 and, consequently, the steps were asymmetric. This asymmetry fell between 1 and 6cm of difference, with a mean of 2. Following treatment, the values for this parameter generally improved, with the mean changing from 2 to 1.2cm.
- -
Step width. In 50% of the patients, the baseline situation was abnormal in that the step width was larger (one patient had a lower than standard value). Four out of five patients with width alteration improved with the physiotherapeutic treatment.
- -
Symmetry of the step angle. At baseline, all the patients presented asymmetry between the right and left step angles, with a degree of asymmetry ranging between 2° and 16°. After treatment, this symmetry showed an important correction, going from a pre-treatment mean of 7.4° to a mean of 2.1° post-treatment.
Results and mean values for the length, speed and cadence gait variables.
| Patient | Pre-treatment value | Post-treatment value | Standard |
|---|---|---|---|
| Cycle length (cm) | |||
| Females | |||
| 1 | 99 | 106 | 122–133 |
| 3 | 104 | 118 | 122–133 |
| Mean | 101.5 | 112 | 122–133 |
| Males | |||
| 2 | 119 | 118 | 141–157 |
| 4 | 116 | 104 | 141–157 |
| 5 | 108 | 115 | 141–157 |
| 6 | 135 | 131 | 141–157 |
| 7 | 180 | 162 | 141–157 |
| 8 | 133 | 134 | 141–157 |
| 9 | 111 | 127 | 141–157 |
| 10 | 126 | 136 | 141–157 |
| Mean | 128.5 | 128.4 | 141–157 |
| Speed (m/s) | |||
| Females | |||
| 1 | 1.43 | 1.5 | 0.83–1.30 |
| 3 | 2 | 2 | 0.83–1.30 |
| Mean | 1.71 | 1.75 | 0.83–1.30 |
| Males | |||
| 2 | 1.54 | 1.54 | 1.0–1.53 |
| 4 | 1.66 | 1.43 | 1.0–1.53 |
| 5 | 2 | 2 | 1.0–1.53 |
| 6 | 2 | 1.7 | 1.0–1.53 |
| 7 | 2.2 | 2.5 | 1.0–1.53 |
| 8 | 2.4 | 2.5 | 1.0–1.53 |
| 9 | 1.5 | 1.8 | 1.0–1.53 |
| 10 | 1.7 | 1.3 | 1.0–1.53 |
| Mean | 1.87 | 1.85 | 1.0–1.53 |
| Cadence (steps/min) | |||
| Females | |||
| 1 | 120 | 120 | 73–117 |
| 3 | 125 | 125 | 73–117 |
| Mean | 122.5 | 122.5 | 73–117 |
| Males | |||
| 2 | 129 | 120 | 80–117 |
| 4 | 120 | 128 | 80–117 |
| 5 | 132 | 132 | 80–117 |
| 6 | 130 | 120 | 80–117 |
| 7 | 133 | 135 | 80–117 |
| 8 | 138 | 150 | 80–117 |
| 9 | 112 | 131 | 80–117 |
| 10 | 107 | 100 | 80–117 |
| Mean | 125.1 | 127 | 80–117 |
Results of the symmetry of step, step width and symmetry of the step angle variables and comparison with their standard values.
| Patient | Pre-treatment value | Post-treatment value | Standard |
|---|---|---|---|
| Symmetry of step (cm) | |||
| 1 | 2 | 1 | 0 |
| 2 | 3 | 1 | 0 |
| 3 | 6 | 5 | 0 |
| 4 | 0 | 0 | 0 |
| 5 | 2 | 2 | 0 |
| 6 | 3 | 0 | 0 |
| 7 | 2 | 0 | 0 |
| 8 | 1 | 0 | 0 |
| 9 | 1 | 1 | 0 |
| 10 | 0 | 2 | 0 |
| Mean | 2 | 1.2 | 0 |
| Step width (cm) | |||
| 1 | 9 | 7.5 | 6–12 |
| 2 | 6.5 | 10 | 6–12 |
| 3 | 17 | 12 | 6–12 |
| 4 | 10 | 10 | 6–12 |
| 5 | 8.5 | 12 | 6–12 |
| 6 | 5 | 6 | 6–12 |
| 7 | 12.5 | 17 | 6–12 |
| 8 | 12 | 9 | 6–12 |
| 9 | 13 | 11 | 6–12 |
| 10 | 12.5 | 11.5 | 6–12 |
| Mean | 10.6 | 10.6 | 6–12 |
| Symmetry of step angle (°) | |||
| 1 | 4 | 3 | 0 |
| 2 | 3 | 1 | 0 |
| 3 | 16 | 14 | 0 |
| 4 | 10 | 0 | 0 |
| 5 | 6 | 0 | 0 |
| 6 | 2 | 0 | 0 |
| 7 | 4 | 0 | 0 |
| 8 | 3 | 1 | 0 |
| 9 | 16 | 1 | 0 |
| 10 | 10 | 1 | 0 |
| Mean | 7.4 | 2.1 | 0 |
Analysing the step angles separately, the right step angle was the one most predominantly deviated (14.8°, when the norm lies between 8° and 10°). This was significantly corrected following treatment, changing to a mean of 9.2°. Both the improvement in the symmetry of the step angle and the improvement in the right step angle were statistically significant, with the following values:
- •
Symmetry of the step angle F19=13.02473; P=.0057.
- •
Right step angle F19=11.27157; P=.0084.
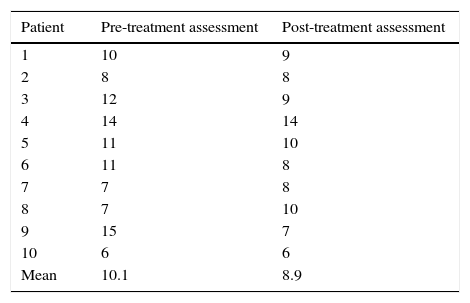
The analysis of the qualitative gait scale revealed pathological pre-treatment values, with scores ranging from 6 to 15 (mean of 10.1). After treatment, there was a slight improvement in these scores, with the mean dropping to 8.9. However, the differences were not statistically significant (Table 4).
We complemented the pre- and post-treatment assessments with the physiotherapist evaluator's blinded subjective evaluation of the subjects’ posture and arm swing in counterphase. Both these parameters were abnormal in all patients in the pre-treatment evaluation, but were still not considered normal in the second evaluation. It is worth emphasising that 40% of the patients showed a lack of arm swing in the baseline evaluation, dropping to 20% after treatment.
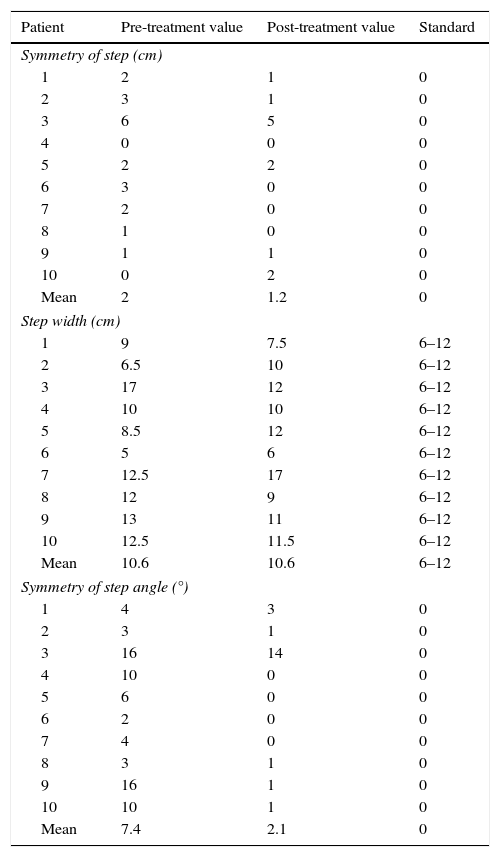
The analysis of the mean values for each of the variables studied (Table 5) showed that there was a 50% improvement in mean values, 20% remained stable and 30% became worse. The improvement corresponded to the variables of cycle length in the females, symmetry of step, symmetry of step angle, speed in males and qualitative gait scale totals. Among these differences, the improvement in the symmetry of step angle was the only statistically significant one.
Mean values for the quantitative gait variables and for the qualitative gait scale total.
| Mean gait variable values | |||
|---|---|---|---|
| Variables | Pre-treatment | Post-treatment | Standard |
| Cycle length (cm) | |||
| Females | 101.5 | 112 | 122–133 |
| Males | 128.5 | 128.4 | 141–157 |
| Symmetry of step | 2 | 1.2 | 0 |
| Step width (cm) | 10.6 | 10.6 | 6–12 |
| Symmetry of angle | 7.4 | 2.1* | 0 |
| Speed (m/s) | |||
| Females | 1.72 | 1.75 | 0.83–1.30 |
| Males | 1.88 | 1.85 | 1.00–1.53 |
| Cadence (steps/min) | |||
| Females | 122.5 | 122.5 | 73–117 |
| Males | 125 | 127 | 80–117 |
| Qualitative scale total | 10.1 | 8.9 | 0 |
In our study, we assessed the baseline situation of 10 adult patients with DS that had not specific stability or walking complaints and lacked other disorders that could interfere with gait. In spite of this, we found that the subjects generally had a posture and gait pattern that clearly deviated from what is considered standard for their population of reference (decreased cycle length, increased speed and cadence, asymmetrical step and step angle, altered standing posture and altered counterphase arm swing).
There are prior studies in which the presence gait disorders are described in patients with SD.2–6,19 However, we consider that identifying the persistence of these alterations in the adult patient is of interest, along with qualitatively characterising the alterations. With this information, individualised physiotherapeutic interventions become possible, as in this study.
There are sufficient clinical experiences and prior research that confirm that early attention to children with DS is effective.5 These differences are based on taking advantage of the phenomenon of neuroplasticity to improve psychomotor development. Although this phenomenon occurs predominantly in children, there is current evidence that neuroplasticity persists during adult life. The fact that the musculoskeletal system has the capacity to adapt has also been established.14 All of this provides a theoretical basis from which we can conceive that it is possible for physiotherapy to benefit the neurological control of the adult with DS, even though there had been no studies on this question until now.
This study provides data indicating that these benefits are real and clinically applicable, generally improving gait pattern. It is notable that there are significant changes in symmetry for the step angle, in spite of the limited sample of patients treated.
Achieving a qualitative improvement of the gait pattern in patients that preserve functionality (as is the case in our sample) could have an effect on preventing or delaying the appearance of chronic osteoarticular diseases, which are especially common in individuals with DS. This would be particularly interesting to evaluate in studies with long-term follow-up.
Although our study sample was limited, the results indicate an overall benefit from the treatment. It would be of great interest to extend the research, in this sense, with controlled studies, larger samples and the possibility of carrying out developmental follow-up.
In short, we have been able to demonstrate that adults with DS present posture and walking disorders that differentiate them from the population without DS. These disorders can be modified through directed physiotherapeutic intervention, and the Bobath concept can be useful for this treatment. Changing the gait pattern could help to prevent long-term complications and increase functional improvement. Further research is needed in this area.
Conflict of interestThe authors have no conflicts of interest to declare.
The contents of this publication are part of the Master's Thesis Neurorehabilitation presented by Maria de las Mercedes Bermejo House at the Catholic University of Murcia in June 2014 were also presented in part at the LXVI Meeting of the Spanish Society of Neurology, in Valencia in November 2014.