Dilated pupil is an important factor for good visualization during pars plana vitrectomy (PPV) in patients with diabetic retinopathy. Despite its side effects, intravitreal adrenaline has been used to maintain pupil dilation.
ObjectiveTo assess the effect of intravitreal adrenaline infusion on pupil dilation in patients with diabetic retinopathy undergoing PPV.
MethodsThis study included 30 eyes of 30 patients with progressive diabetic retinopathy underwent PPV. Pupils of all eyes were dilated by topical application of a combination of 1% tropicamide and 2.5% phenylephrine, and eyes were randomized 1:1 to continuous intravitreous infusion of adrenaline (0.5mg/500ml in balanced salt solution) or vehicle control. Surgical procedures were recorded with a high definition video recorder. Normalized pupillary area (NPA) was measured on recorded images before and at the end of surgery.
ResultsPost-operative NPA differed significantly between the two groups (p=0.04). By contrast, pre-operative NPA (p=0.81) and changes in NPA (p=0.17) did not.
ConclusionIntravitreal infusion of adrenaline did not have a significant effect on pupil dilation, compared with non-adrenaline, in patients with diabetic retinopathy undergoing PPV.
La dilatación de la pupila es un factor importante para una buena visualización durante la vitrectomía pars plana (VPP) en pacientes con retinopatía diabética. A pesar de sus efectos secundarios, la adrenalina intravítrea se ha utilizado para mantener la dilatación de la pupila.
ObjetivoEvaluar el efecto de la infusión de adrenalina en la dilatación de la pupila intravítrea en pacientes con retinopatía diabética sometidos a VPP.
MétodosEn este estudio se incluyeron 30 ojos de 30 pacientes con retinopatía diabética progresiva que se sometieron a VPP. Las pupilas de todos los ojos estaban dilatadas por aplicación tópica de una combinación del 1% de tropicamida y fenilefrina al 2.5%, y los ojos fueron asignados al azar 1:1 a infusión continua intravítrea de adrenalina (0.5mg/500ml en solución salina equilibrada) o a control de vehículo. Los procedimientos quirúrgicos se registraron con un grabador de vídeo de alta definición. El área pupilar normalizada (NPA) se midió en las imágenes grabadas antes y al final de la cirugía.
ResultadosLa NPA postoperatoria difería significativamente entre los 2 grupos (p=0,04). Por el contrario, en lo referente a la NPA antes de la operación (p=0,81) y después de los cambios en la NPA (p=0,17) no hubo esas diferencias entre grupos.
ConclusiónLa infusión de adrenalina intravítrea no tuvo un efecto significativo sobre la dilatación de la pupila, en comparación con los casos de no infusión de adrenalina, en pacientes con retinopatía diabética sometidos a VPP.
Maintaining a dilated pupil during pars plana vitrectomy (PPV) is an important factor for good visualization during surgery, particularly for patients with diabetic retinopathy. Because diabetic patients show a small resting pupil and weak mydriasis response, eyes of diabetic patients undergoing PPV are frequently treated with continuous intravitreal infusions of adrenaline, diluted in balanced salt solution (BSS), to maintain pupillary dilation.1,2 Adrenaline is frequently added to the indwelling posterior segment infusion during vitreoretinal procedures in order to maintain peri-operative mydriasis and assist with hemostasis.3 Previous study shows that adrenaline in the intraocular infusion has beneficial effect in maintaining mydriasis in cataract surgery.4
Adrenaline, however, was shown to induce the synthesis of endogenous prostaglandins, which can disrupt the blood-retinal barrier and cause cystoid macular edema.5,6 Adrenaline has also been found to significantly reduce blood flow to the optic nerve head and have cardiovascular adverse effects.7 This study investigated the ability of continuously infused intravitreal adrenaline to maintain pupil dilation during PPV in patients with diabetic retinopathy.
Subjects and methodsThis study was a randomized control trial involving 30 eyes of 30 patients with diabetic retinopathy who underwent PPV at Cicendo Eye Hospital. Written informed consent was obtained from each patient, and the study protocol was approved by the Ethics Committee of the Faculty of Medicine of Padjadjaran University.
Consecutive patients were enrolled and randomized 1:1 using block permutation to the treatment (adrenaline) and control (non-adrenaline) groups, each consisting of 15 patients. Adrenaline solution for intravitreal infusion consisted of 0.5mg adrenaline dissolved in 500ml BSS. Each pupil was dilated by topical application of one drop of tropicamide 1% and one drop of phenylephrine 2.5% three times each at 60, 45, and 30min before surgery.
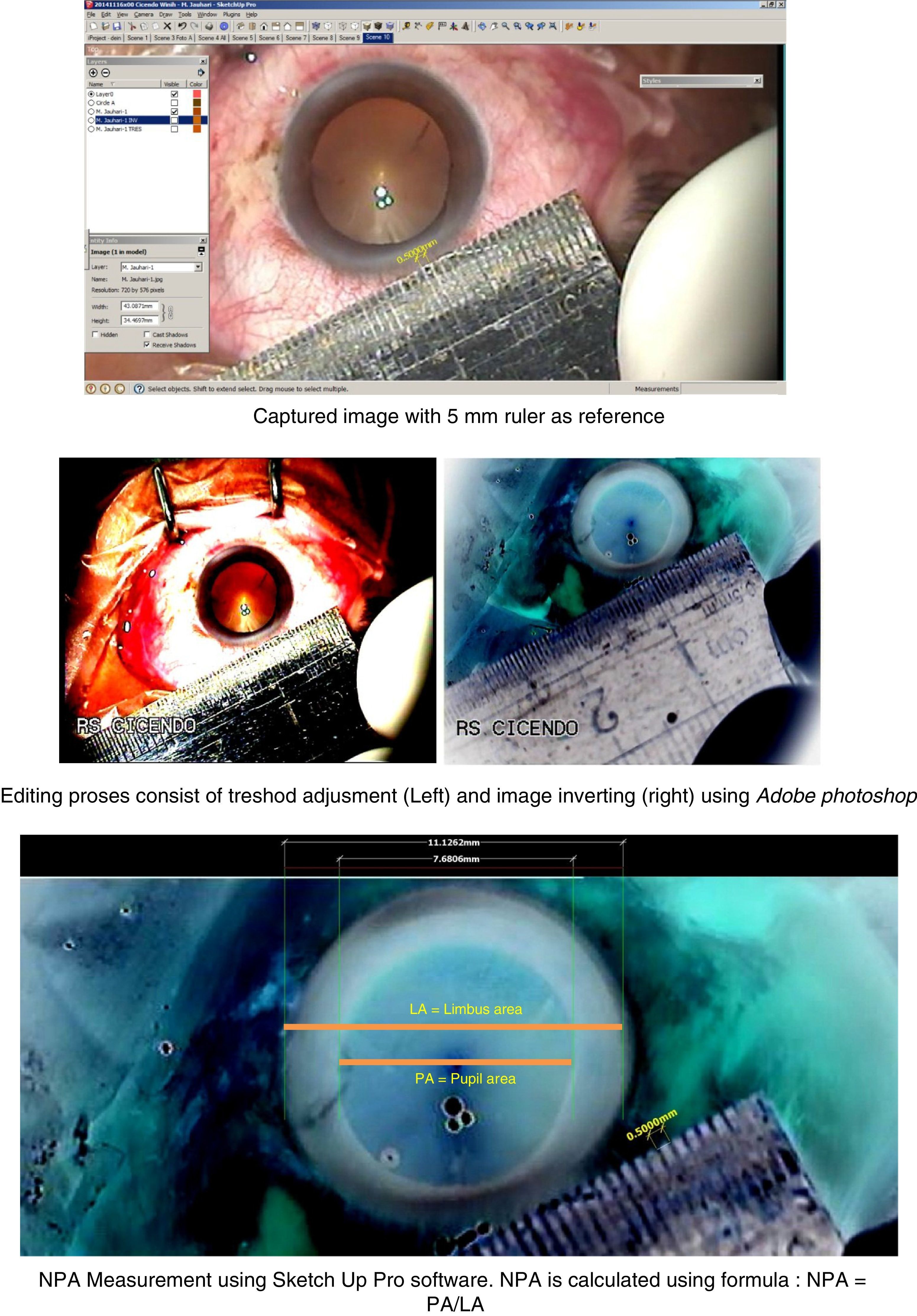
All surgical procedures were recorded with a high definition video recorder. Eye parameters were measured using by Sketch Up Pro on photos of each recording, which had been edited with Adobe Photoshop. Pupillary dilation was determined by measuring normalized pupillary area (NPA), defined as pupillary horizontal diameter divided by limbal horizontal diameter in millimeters (Fig. 1). NPA was measured twice in each eye, before and after surgery, and the difference was calculated. NPA was measured by individuals blinded to subject allocation. Statistical analyses were performed using SPSS® software.
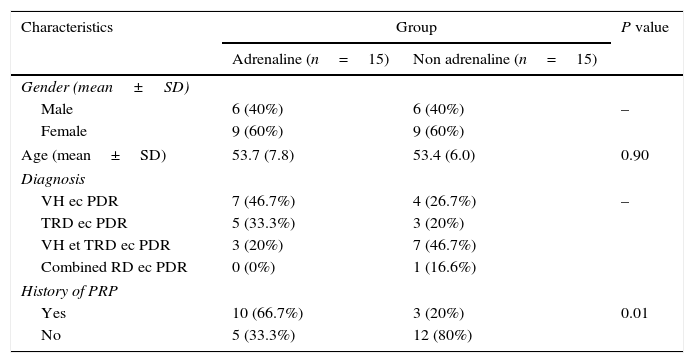
ResultsOf the 30 patients included in this study, 15 were randomized to the adrenaline group and 15 to the control group. Their mean ages were 53.7 years and 53.4 years, respectively, and there were no significant between-group differences in age and gender distribution. The most common diagnosis in the adrenaline group was vitreous hemorrhage due to progressive diabetic retinopathy (PDR; 46.7%) and the most common diagnoses in the control group were vitreous hemorrhage and tractional retinal detachment due to PDR (46.7%). Ten (66.7%) patients in the adrenaline group and three (20%) in the control group had a history of pan-retinal photocoagulation (p=0.01). Table 1 shows the detailed characteristics of the study subjects.
Characteristics of the study subjects.
| Characteristics | Group | P value | |
|---|---|---|---|
| Adrenaline (n=15) | Non adrenaline (n=15) | ||
| Gender (mean±SD) | |||
| Male | 6 (40%) | 6 (40%) | – |
| Female | 9 (60%) | 9 (60%) | |
| Age (mean±SD) | 53.7 (7.8) | 53.4 (6.0) | 0.90 |
| Diagnosis | |||
| VH ec PDR | 7 (46.7%) | 4 (26.7%) | – |
| TRD ec PDR | 5 (33.3%) | 3 (20%) | |
| VH et TRD ec PDR | 3 (20%) | 7 (46.7%) | |
| Combined RD ec PDR | 0 (0%) | 1 (16.6%) | |
| History of PRP | |||
| Yes | 10 (66.7%) | 3 (20%) | 0.01 |
| No | 5 (33.3%) | 12 (80%) | |
PDR, proliferative diabetic retinopathy; VH, vitreous hemorrhage; TRD, tractional retinal detachment; RD, retinal detachment; PRP, pan retinal photocoagulation.
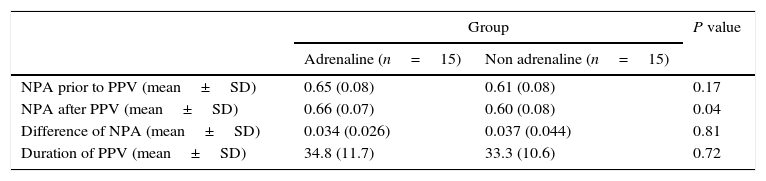
Although NPA before surgery was similar in the adrenaline and control groups (0.65 vs. 0.61, p=0.17), NPA was significantly higher after surgery in the adrenaline than in the control group (0.66 vs. 0.60, p=0.04). Mean differences in NPA were similar in the two groups (Table 2).
Measurement of normalized pupillary area (NPA) and duration of PPV.
| Group | P value | ||
|---|---|---|---|
| Adrenaline (n=15) | Non adrenaline (n=15) | ||
| NPA prior to PPV (mean±SD) | 0.65 (0.08) | 0.61 (0.08) | 0.17 |
| NPA after PPV (mean±SD) | 0.66 (0.07) | 0.60 (0.08) | 0.04 |
| Difference of NPA (mean±SD) | 0.034 (0.026) | 0.037 (0.044) | 0.81 |
| Duration of PPV (mean±SD) | 34.8 (11.7) | 33.3 (10.6) | 0.72 |
NPA, normalized pupillary area.
Diabetic patients have smaller sized pupils and weaker dilation than healthy individuals.8 These alterations in diabetic patients are caused by sympathetic nerve neuropathy and degenerative changes in pupillary dilator muscle. Degenerative changes have been observed in smooth muscle, nerve endings, and connective tissues of diabetic irises.9 Electron microscopy showed that, in diabetic individuals, pathologic changes were greater in pupillary dilator muscles than in pupillary sphincter muscle.10 Glycogen accumulation by pigment epithelial layer was also documented in diabetic irises.11
In a dark environment, pupillary size in diabetic patients is inversely proportional to both the duration of diabetes and blood glucose level. Duration of diabetes in this study was uncertain, since most study subjects could not accurately determine the time of disease onset, and others were found to have diabetes on diagnosis of diabetic retinopathy. Diabetes can be determined by measuring blood levels of glucose and HbA1C, a marker for control of glucose level. However, most of the subjects in this study were not checked their level of HbA1C. Therefore, this is considered as one of the limitations of this study.
This study found that treatment with adrenaline did not significantly alter pupil response in the two groups. Adrenaline has a short half-life of 2–3min and is rapidly eliminated through body organs. In addition, contractions of the pupillary dilator muscle are mediated by the α1 receptor located in this muscle. This muscle embryologically originated from the anterior iris, along with blood vessels and nerves that supplied the muscle. The administration of adrenaline by intravitreal infusion in this study assumed that flow from the anterior segment to the anterior iris was blocked by a barrier consisting of the posterior lens capsule and anterior hyaloid. All of the subjects included in this study were phakic. Thus results may differ if subjects are aphakic or if the posterior lens capsule and anterior hyaloid are not intact, a barrier deprivation that can create a communication between the vitreous and anterior chambers (3). Intravitreal adrenaline is an α1 agonist that acts on pupillary dilator muscle. However, following topical application of 2.5% phenylephrine, an α adrenergic agonist, adrenaline cannot bind to its receptors at times shorter than its half-life (2–3h).
The results of this study differed from those of another assessing the effects of intravitreal infusion of two adrenaline concentrations, 0.5 and 1mg/500ml, on pupillary diameter.7 That previous study found that both adrenaline doses resulted in significant pupil dilation, but most subjects had already undergone cataract surgery and their lens status and posterior capsule were unreported. For example, an aphakic lens and/or a posterior lens rupture could result in “barrier deprivation”, creating a communication between the anterior and posterior segments and affecting the pharmacokinetics of intravitreal adrenaline. Lens status (aphakia or pseudophakia) also contributes to differences in pupillary size.
Pupillary dilation response may also be influenced by other factors, including age. Older age has been associated with pupillary myosis and decreased sympathetic tone of the pupillary dilator muscle.12 However, in this study, there was no difference in age distribution between the treatment and control groups. Pupillary response to drugs that dilate pupils depended on iris color, as determined by race. Dark irises contain more melanin pigment, making it harder to dilate their pupils using a standard dose of the drugs. A study of the mydriatic effects of phenylephrine, cyclopentolate, scopolamine, homatropine, and atropine on blue, brown and dark irises, depending on race showed that phenylephrine was ineffective as a mydriatic agent on eyes from black subjects. By contrast, treatment with scopolamine, homatropine, and cyclopentolate resulted in approximately equal degrees of mydriasis in the three races studied.13–15 Because our subjects did not differ in race, outcomes associated with race were not determined.
Eyes of diabetic patients show a weak pupillary dilation response to instillation of anticholinergic drugs, but hypersensitivity to adrenergic drugs. The decreased sympathetic tone in patients with diabetic retinopathy may explain why additional instillation of a sympathomimetic agent, such as phenylephrine, can cause a diabetic pupil to become hypersensitive, resulting in combinations of anticholinergic and sympathomimetic agents achieving adequate dilation in diabetic patients.13,15 This became the basis of preoperatively instilling combinations of cycloplegic (e.g., tropicamide) and sympathomimetic (e.g., phenylephrine) agents to dilate the pupil, as in this study.
The ability to dilate the pupil is reduced in diabetic retinopathy patients who have already undergone pan-retinal photocoagulation (PRP). It remains unclear, however, whether PRP itself is responsible or whether the severity of diabetic retinopathy made the diabetic pupil more resistant to mydriatic drugs. In this study, the proportion of subjects with a history of PRP was larger in the adrenaline than in the control group.
Pupillary dilation response on images can be estimated by counting pixels present in pupils using round or elliptical fitting or by assessing NPA.2 The optimal method of measuring pupillary area has not been determined, although NPA is reported to be superior to counting pixels and ellipse fitting because it minimizes noise in the periphery pupil and limbus.16,17
NPA was also measured in this study because of inter-individual differences in pupil structure and the ability to dilate and constrict the pupil, thus affecting iris response to light stimuli and drugs. This condition must be controlled for during comparisons of pupillary responses among individuals. For example, under scotopic conditions, papillary constriction will be lower in individuals with a pupillary diameter of 3mm than 5mm. Thus, significant pupillary constriction may be independent of retinal and optic nerve conditions.
The effectiveness of intravitreal adrenaline infusion in maintaining pupillary dilation was determined by measuring differences in NPA before and after surgery, with differences in the difference of NPA compared between the adrenaline and control groups. Although the difference of NPA did not differ significantly between the two groups, postoperative NPA differed significantly. This may have been due to the effects of tamponade with gas or air, the tamponades most frequently used during PPV surgery, especially for tractional retinal detachment due to diabetic retinopathy. Injection of gas or air as a tampon will enlarge pupil diameter.
Intraocular pressure (IOP) can also affect pupillary size. IOP will be higher at the end of surgery, due to an increased infusion pressure of approximately 25–30mmHg performed to prevent leakage from a sclerotomy wound. This condition will result in a larger pupil diameter at the end of surgery. The effects of tamponade and IOP on pupil diameter may have introduced bias in this study.
The duration of PPV surgery can also alter the effects of mydriatic drugs and dilation response. A longer duration of surgery can also increase surgical trauma, including the release of prostaglandins, neuropeptides such as substance P and calcitonin, enhancing miosis in diabetic irises. The mean duration of surgery was similar in the adrenaline and control groups (34.8 vs. 33.3min, p=0.72). All subjects in this study were administered topical tropicamide 1% and phenylephrine 2.5%, starting approximately 60min before surgery, to dilate their pupils. The mean duration of the pupillary dilation procedure and surgery was 94min. Tropicamide was effective for 6h and phenylephrine for 2–3h, indicating that the entire procedure was performed while the drugs were effective.
This study had several limitations. The first is the method used to measure pupil size. That is, the position of the eye or eye movement will affect the angle between the camera and the eye, altering the number of pixels captured by the camera and the shape of the circle or line fitted onto the pupil. A lower camera position will result in an apparently larger sized pupil.18 This situation can be minimized by positioning the eye using forceps so that it is perpendicular to the camera when the picture is taken. The pharmacokinetics of intravitreal adrenaline are also affected by lens status, intact posterior lens capsule and anterior hyaloid. All subjects in this study had phakic lenses. Studies are needed to compare the effects of intravitreal adrenaline on phakic, pseudophakic eye and aphakic eyes.
In conclusion, intravitreal infusion of adrenaline did not significantly alter pupillary dilation during PPV surgery in patients with diabetic retinopathy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.