Cephalometrics is a standardized universal method for the diagnosis, prediction and treatment planning of various facial deformities. The aim of this article is to propose a simplified bidimensional cephalometric study.
La cefalometría es un método universal estandarizado que permite el diagnóstico, la predicción y la planeación del tratamiento de diversas deformidades dentofaciales. El objetivo del presente artículo es proponer un estudio cefalométrico bidimensional simplificado.
The patient who suffers from a dentofacial deformity experiences functional, aesthetic and psychological alterations which constitute the main reasons for requesting surgical orthodontic treatment.1,2
Pre-surgical assessment includes an examination of the hard and soft tissues of the mouth and face, as well as of masticatory function. Several diagnostic aids such as intra and extra oral clinical photographs, stereolithographic, plaster or plastic models mounted on a semi-adjustable articulator, panoramic radiographs, postero-anterior and lateral cephalograms among others are included in the pre-surgical records set.3
It is important to perform a post-surgical prediction and submit it to the patient with enough anticipation to evaluate their expectations, listen to his or her opinion, doubts and fears regarding the treatment that will aim to achieve a facial change.3,4
There are different methods for performing a surgical prediction:
- 1.
Pre and post-surgical cephalometric tracing based on a standardized lateral headfilm.
- 2.
Photographic images printed on paper or captured by software.
- 3.
Plaster or stereolithographic models.4–7
The clinician and student who uses these procedures for the first time, may find it difficult to obtain them and manage the specific software.8–10 This causes that the most commonly used prediction procedure is the lateral cephalometric tracing performed on tracing paper.
This article intends to describe a two-dimensional technique for surgical prediction by means of an accessible software based on mean values and techniques already described in the literature by several authors.4,5,10,11
MATERIALS AND METHODSA computer, lateral cephalograms in JPG format, and the Microsoft Office software Power Point(®) in addition to iDraw(®) are used.
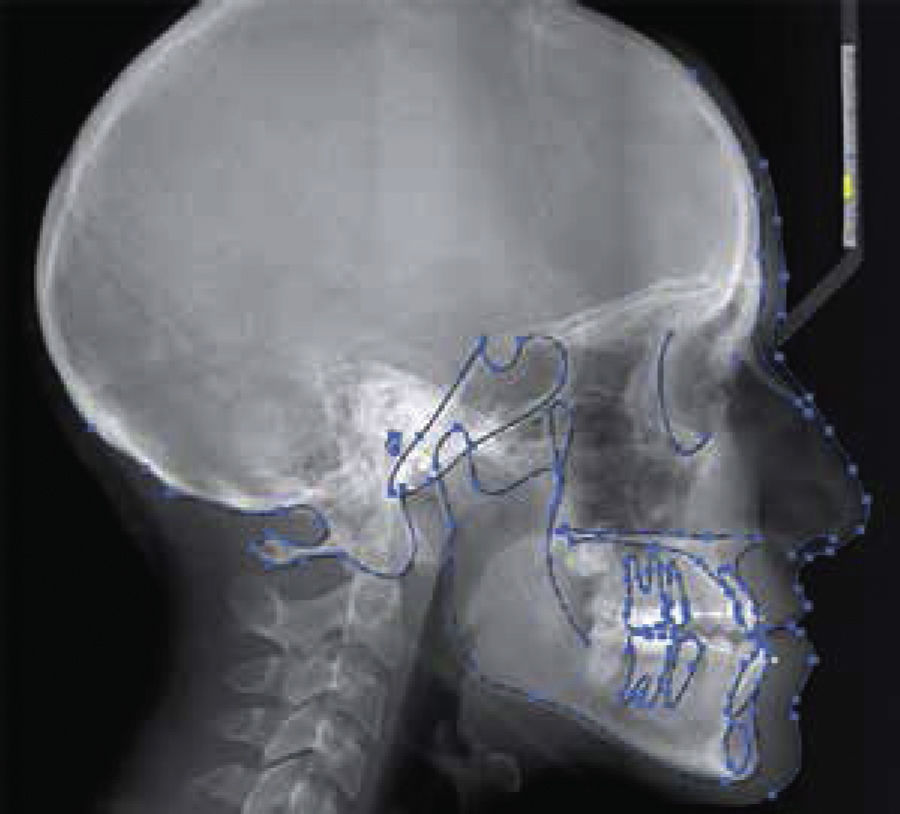
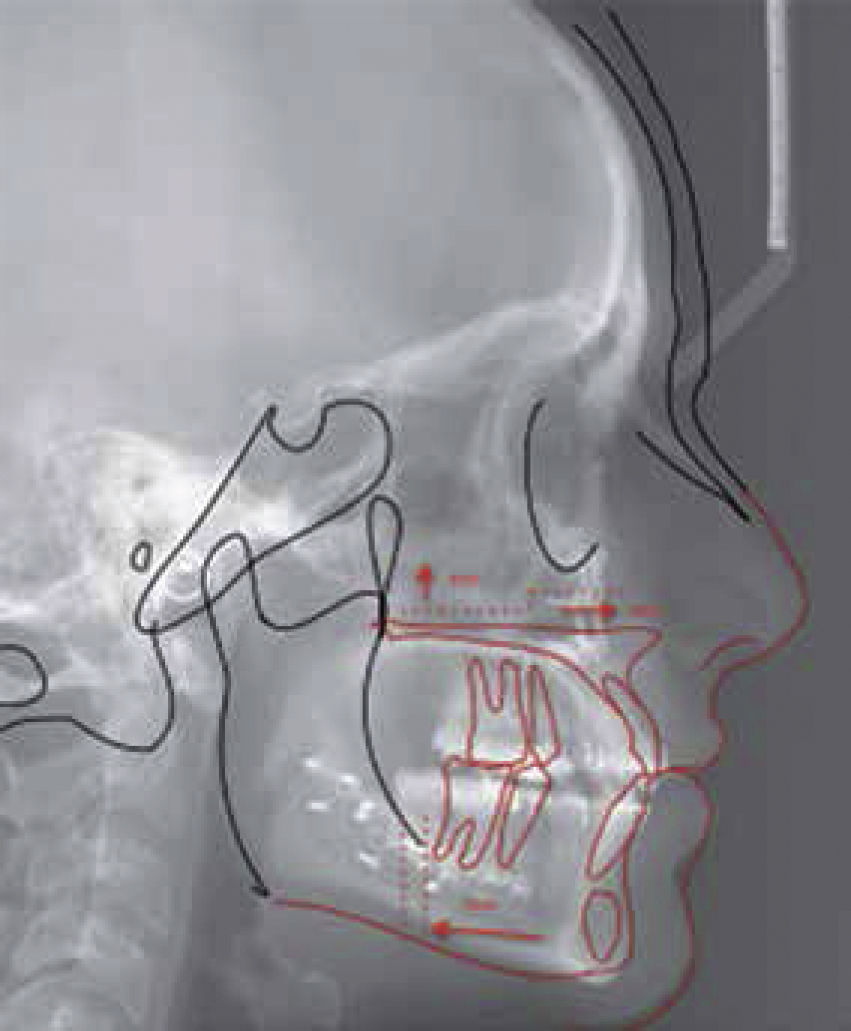
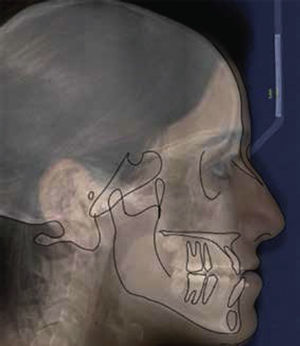
Once the lateral cephalogram in JPG format is placed in a blank document of the Power Point software, a line of 5 or 1cm is drawn over it which will standardize in a 1:1 ratio the cephalometric tracing with respect to the reference rule in the cephalostat, increasing or decreasing the image until both of them match (Figure 1).
Once the relationship of the radiograph is equal to the reference, it is saved as JPG format image in order to open it later with the iDraw(®) program. This program allows easy location of the anatomical structures, by manipulating the image contrast as well as the zoom, without losing sight of the structures that are being worked with.
The outline of the bony and soft structures is performed with the pencil tool by making solid lines or intermittent points of the anatomical structures in the cephalogram. It is important to select the structures that are going to change their position in order to make intervals between mouse clickings (as seen in figure 2): between each blue dot there is a line that may be changed in position and shape, with the opportunity to decide the number of blue dots.
In the event of a mistake during the tracing of the bony and facial contour the tracing segment or dotted lines to be erased are selected and with the Delete key the structures are removed, leaving the rest of the tracing without modifications.
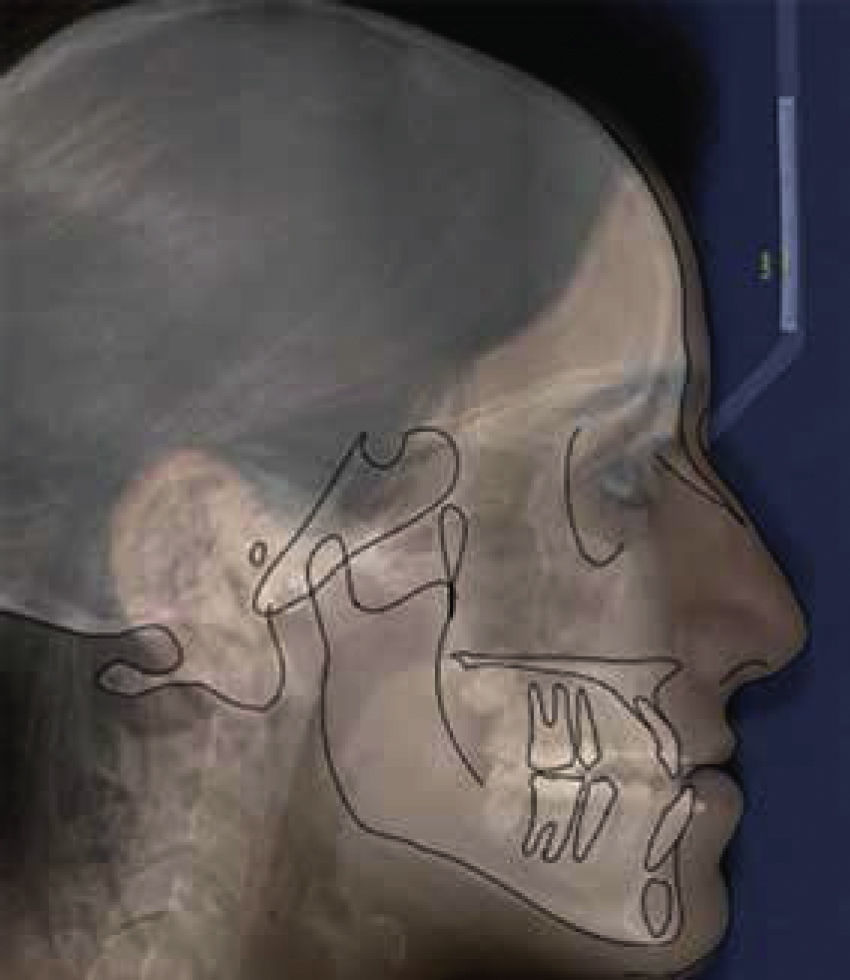
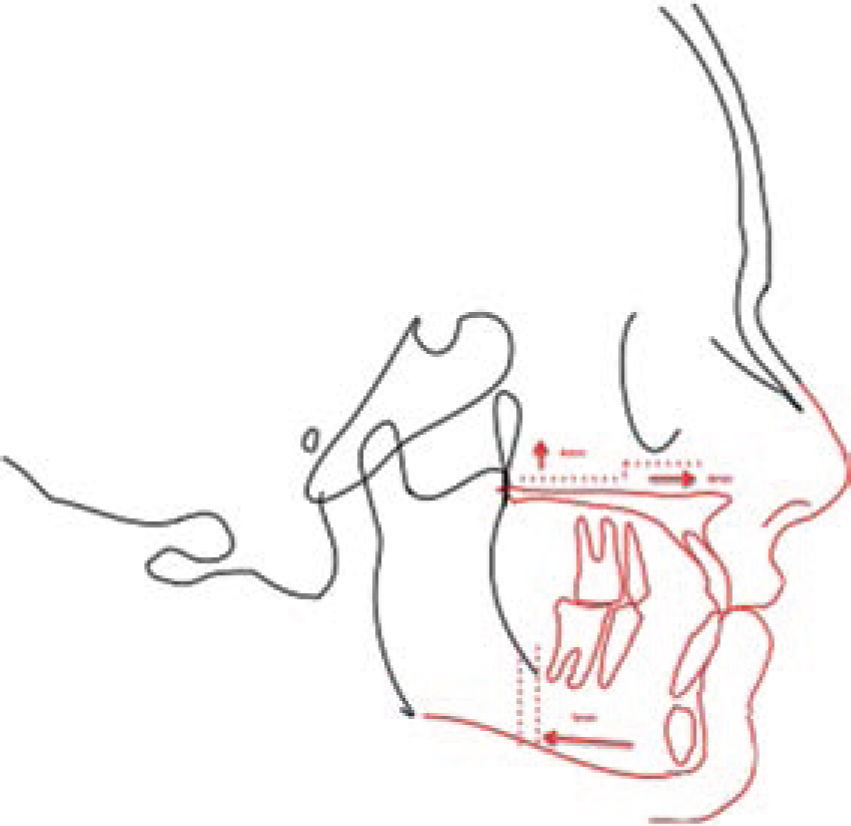
Once the tracing of the bony and facial contour is completed, all segments are selected without the cephalogram image thus the format of bony structures and facial contours to perform the cephalometric tracing are obtained.
The tracing may be printed as many times as necessary in the event requiring more than one cephalometric tracing without having to repeat multiple tracing papers thus avoiding variations when duplicating the procedures manually and having the additional advantage of not needing a cephalometric tracing and view box (Figure 3).
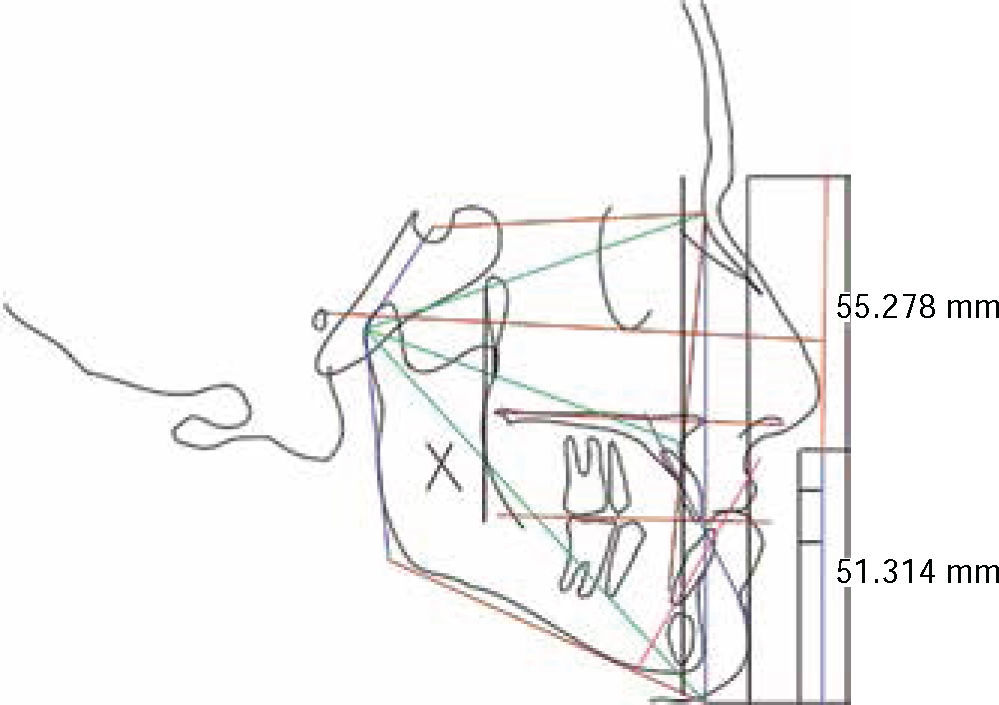
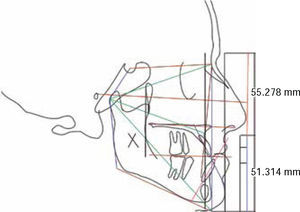
Once the format of bony structures and facial contours has been obtained, the cephalometric tracing that the clinician considers relevant to obtain a diagnosis may be performed by means of an image that has a 1:1 ratio. However, the strokes may also be performed on the iDraw program(®) as shown in figure 4.
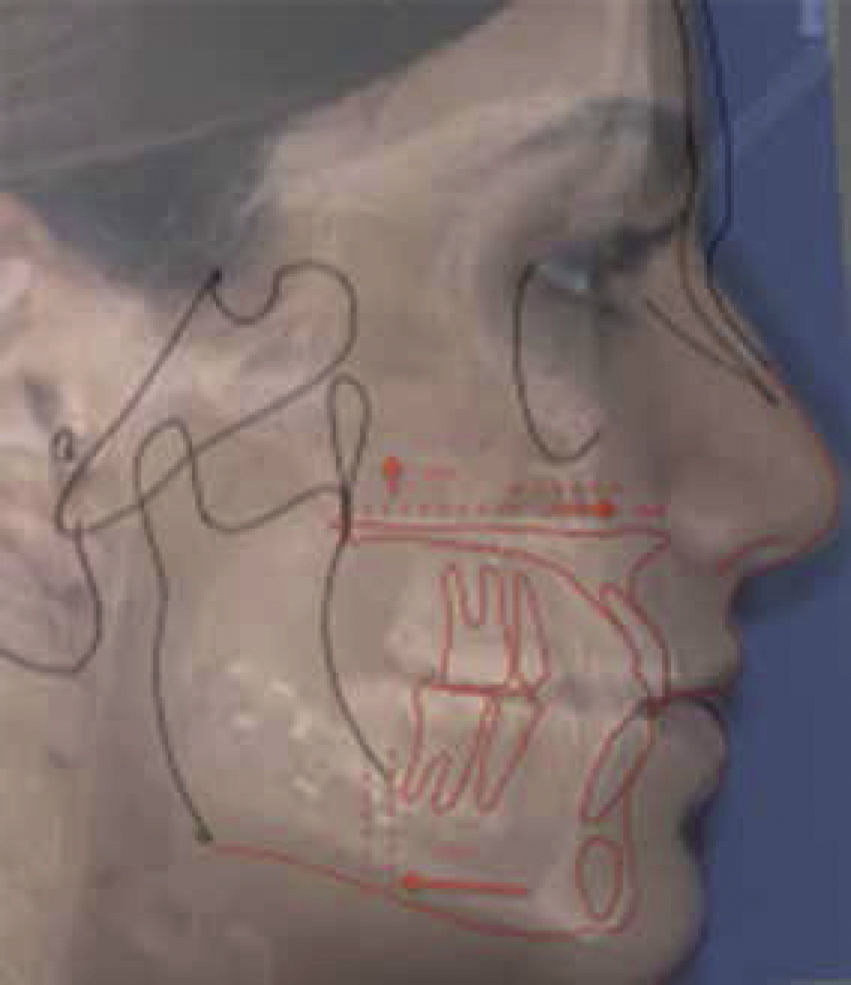
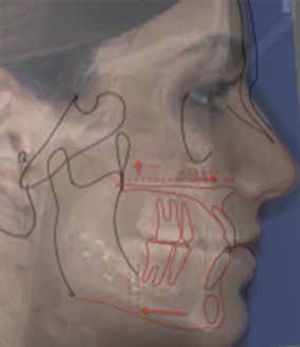
The same format may be used in the Microsoft Office program, Power Point(®)to interact with the patient profile photos and the cephalogram thus obtaining 1:1 ratios of the three images by means of the transparency tool (Figure 5).
With the clinical occlusal and cephalometric diagnosis the surgical prediction is performed using the format created in iDraw(®).
The structures that will not change their position are selected copied and pasted in the Microsoft Office Power Point software(®).
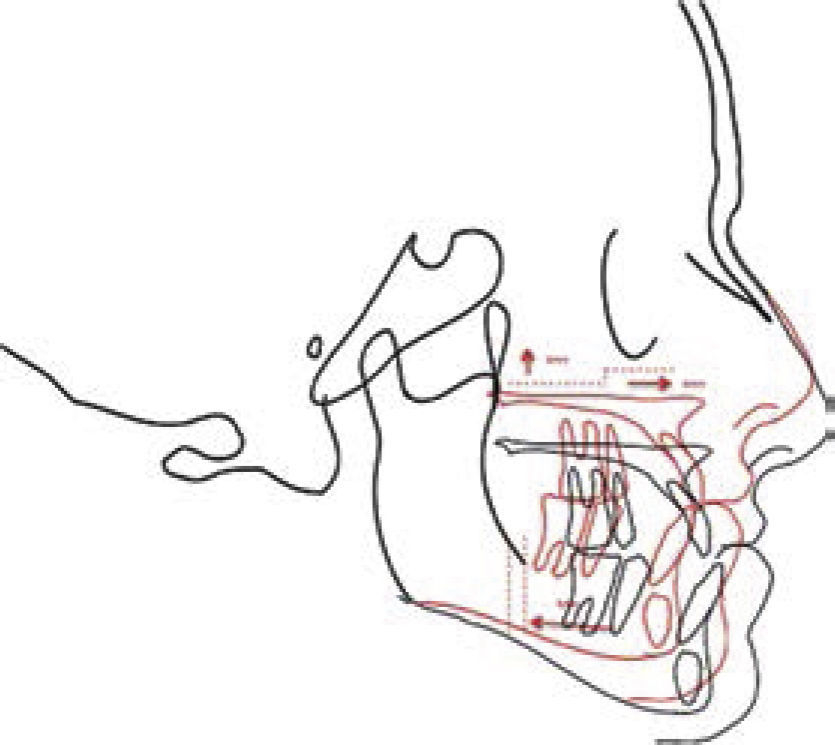
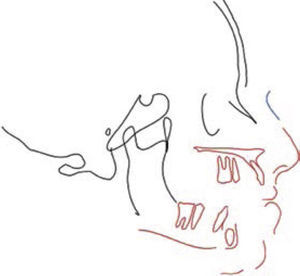
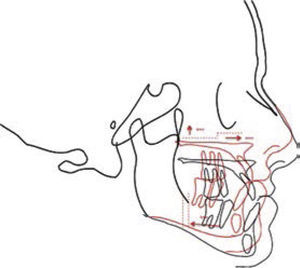
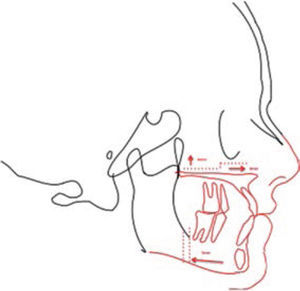
Subsequently the structures that change position are marked, with the option of modifying their color in order to best exemplify their movements, and placed in the Microsoft Office Power Point software(®) as shown in figure 5.
All the structures are placed in the document and based on the results of the diagnosis they may be moved to the desired position since this program allows minutely calculated antero-posterior, vertical and rotational movements (Figure 6).
Once the movements are performed according to the diagnosis, the prediction is obtained and color, text, osteotomy lines or some other necessary element may be applied as exemplified in the Figures 7 and 8.
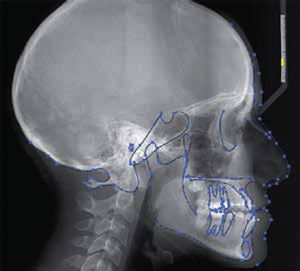
Once the surgery has been conducted, a superimposition of the prediction and the new post-surgical cephalogram, is performed again matching the measurements to a 1:1 ratio with the prior prediction. One may even add the post-surgical photograph for comparison between the prediction and the post-surgical results (Figures 9 and 10).
DISCUSSIONTechnological advancements always play an important role in the evolution of surgical techniques and planning methods.10
Currently digital three-dimensional surgical predictions require highly specialized software and occasionally, the collaboration of trained technicians for their elaboration, by which at times, they are not considered as a first option.11–13 Computer-based surgical simulation has the potential to replace completely the reference standard both in surgical prediction as well as in plaster models surgery.14–16 However, studies comparing three-dimensional techniques with specific software and traditional methods are the only ones who have reported its accuracy and advantages. It is necessary to perform external studies that show a cost-benefit analysis as well as its indications and accuracy.14 It is not possible to adapt or standardize three-dimensional predictions with specific software which makes traditional techniques a standard that continues to be used.15–19
CONCLUSIONSThe surgical prediction hereby described aims to reduce errors that commonly occur when the clinician is confronted for the first time with patients with severe dentofacial deformities. It achieves to simplify steps such as the manual development of multiple tracing papers, errors regarding size of the X-ray or related with the identification of anthropometric o cephalometric points.
The present technique allows, by means of a computer, to draw the facial contour freehand with the mouse, following the anatomical structures, changing the contrast, approaching or moving away from a specific area and in this way makes it easier to observe in more detail. The elaboration of straight lines, selecting a starting point for all of them, the minutely measured rotation and vertical, anterior and posterior movements facilitates tracing a surgical prediction since it is impossible to perform all these on tracing paper, radiographic film or digital radiography printing.
Oral and Maxillofacial Surgeon. Professor of the Faculty of Dentistry, National Autonomous University of Mexico. Professor of the Faculty of Dentistry, Technological University of Mexico.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia