Orthodontic treatment in periodontally compromised adult patients has proven to have long-term stability when both specialties combine efforts with the use of light and continuous forces, good periodontal therapy and proper dental hygiene restoring aesthetic and functional problems thus preventing relapse after treatment. This case report describes a female patient, 58 years of age, with no medical conditions, canine and molar class I, controlled chronic generalized periodontitis, extruded upper incisors, diastemas, gingival recession and dental mobility, vertical and horizontal bone defects, bi-protrusive skeletal class I.
ObjectiveEvaluate the response of periodontal tissue using orthodontic intrusion. 0.018″ x 0.022″ Roth appliances were used and after treatment, upper Hawley and lower bonded retainers.
Results3mm bone gain at the upper incisors area and 1mm in insertion of the gingival tissue; a 3mm intrusion was obtained thus shortening the length of the clinical crown.
ConclusionMultidisciplinary action is effective in intrusion movements that seek to increase alveolar bone as well as gingival insertion, reducing the depth of the periodontal pockets without root resorption and improving the patient's esthetics.
El tratamiento de ortodoncia en pacientes adultos periodontalmente comprometidos ha demostrado estabilidad a largo plazo cuando la combinación con ortodoncia se junta usando fuerzas ligeras y continuas, buena terapia periodontal e higiene dental adecuada, de esta manera se restablecerán problemas estéticos y funcionales previniendo la recidiva después del tratamiento. Este caso es de una paciente de 58 años sin antecedentes médicos, el diagnóstico: clase I canina y molar, biprotrusivo, clase I esquelética, enfermedad periodontal controlada, incisivos superiores extruidos, diastemas, recesión gingival y movilidad dental; defectos óseos verticales y horizontales.
ObjetivoEvaluar la respuesta del tejido periodontal mediante intrusión de incisivos a través de movimientos ortodónticos; se utilizó filosofía Roth 0.018″ x 0.022″, como retención placa Hawley superior y fija inferior.
ResultadosGanancia de 3mm a nivel óseo en los incisivos superiores y 1mm en la inserción del tejido gingival, intrusión de 3mm acortando la longitud de la corona clínica.
ConclusiónLa interacción multidisciplinaria es efectiva en el movimiento de intrusión dental obteniendo aumento de hueso alveolar e inserción gingival reduciendo la profundidad de las bolsas periodontales sin reabsorción radicular y mejorando la estética del paciente.
Nowadays, patients who seek orthodontic consultation are, to a large percentage, adults who have periodontal disease which causes an accelerated loss of support structures of the periodontal ligament causing pathological dental migration with upper incisor proclination, diastemas, rotations, extrusions, etc.1 Periodontitis with extruded incisors not only causes a premature contact of the occlusion, but also adversely affects dental aesthetics. Treatment of these patients requires multidisciplinary work to restore a healthy, functional and aesthetic dentition; in many cases dental intrusion through orthodontics is required to promote alveolar bone and soft tissue remodeling.1,2 Efficiency and treatment success depend on the response of the periodontal tissues, associated with the physiological processes of the activity of connective tissue cells in the alveolar bone.3,4
Erkan M. et al in their experimental study in 2007 reported that the intrusion movement increases the interproximal level of alveolar ridges, if periodontal therapy is evaluated periodically and the forces used are light (0.25N).5
Patients with periodontal disease may present two types of bone defects: horizontal and vertical; if they are treated with orthodontics to recover the loss of periodontal tissues where the morphology of the bone defect is angular, the complement with guided tissue regeneration would boost the improvement of the periodontal tissue and long-term stability of orthodontics.5,6
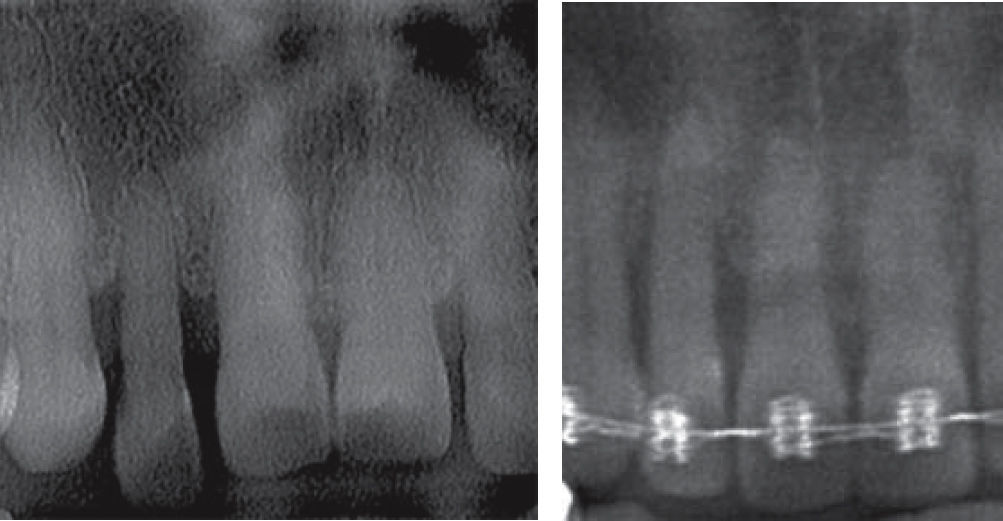
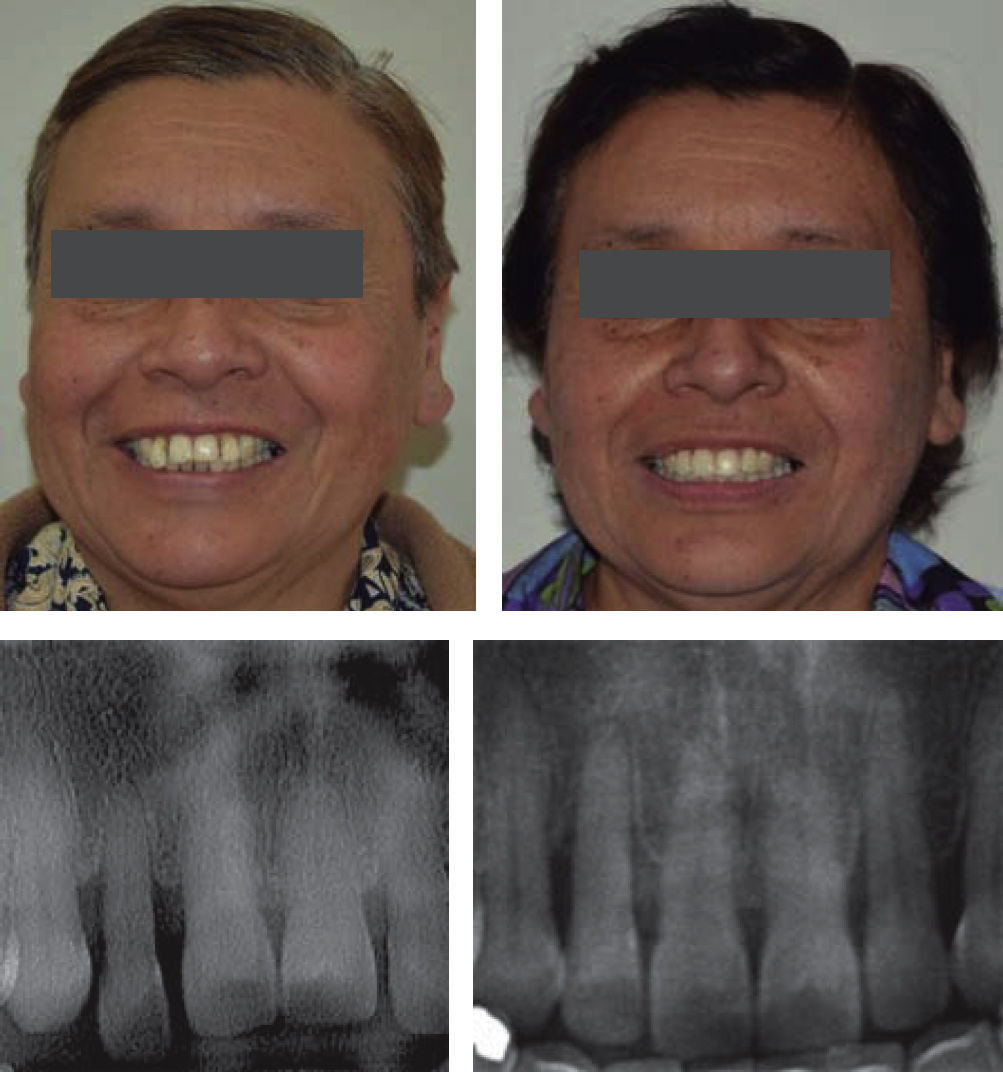
METHODSThe present case is a female patient of 58 years of age without apparent pathological antecedents; in her dental diagnosis she presented mismatched dental midlines, molar and canine class I, generalized chronic periodontitis, extruded upper lateral incisors, gingival embrasures, spacing, gingival recession and dental mobility; the radiological diagnosis determined vertical and horizontal bone defects; the cephalometric diagnosis revealed a straight profile, positive labial step, biprotrusive skeletal class I, dolichofacial biotype and upper incisor proclination. Everything described previously may be observed in (Figures 1 to 3).
The main concern of the orthodontist is to assess the stability of treatment results in periodontally compromised patients, hence the objective of this study was to analyze, evaluate, and improve the periodontal response parameters for orthodontic intrusion of upper lateral incisors; the treatment plan consisted of placement of 0.018″ x 0.022″ slot Roth appliances; the alignment and leveling phase was performed with 0.012″ x 0.012″ nickel titanium archwires, up to 0.016 stainless steel, respectively. In each orthodontic monthly appointment the patient was assessed periodontally; in the space closure phase elastic thread and intermediate open chain was used along with 0.016″ x 0.016″ Nickel Titanium and 0.016″ x 0.016″ SS archwires. For the final phase 0.016″ x 0.016″ Stainless Steel archwires and ¼ 3.5 oz light elastics were used. Finally, for retention an upper Hawley retainer and a lower fixed retainer from canine to canine were placed (Figures 4 to 6).
EthicsThe responsible committee established the ethical aspects by using the informed consent attached to the patient's clinical record of the Department of Orthodontics of the Division of Pos-graduate Studies and Research of the National Autonomous University of Mexico (UNAM) and with the Helsinki Declaration of 1975.
RESULTSThe results showed favorable changes by both clinical and radiological parameters.
A 3mm bone gain was obtained in the upper right lateral incisor and a 2mm gain for upper left lateral incisor; at the level of the central incisors, a 1mm increase was observed and 1mm of gingival tissue insertion. Leveling of the teeth was accomplished with a 3.5mm intrusion, shortening of the length of the clinical crown, a decrease in the depth of the periodontal pockets, nivelation of teeth with intrusion of 3.5mm, shortening the length of the clinical crown, reduction of the depth of periodontal pockets, clinical attachment gain without root resorption, closing of triangles and clear improvement in the aesthetic and the patient's smile, all this observed in figures 7 and 8.
DISCUSSIONRosa Marco et al., in 2016, through their study showed that the tension that the periodontal ligament experiments concentrated in the cervical area is related to the application point of the orthodontic force.4,7
Tian Cao et al in 2015 demonstrated bone loss during dental intrusion causing widening of the periodontal ligament space at the cervical area and deepening of periodontal pockets which they attributed to the displacement of the junctional epithelium that caused resorption of the marginal ridges to preserve the periodontal ligament in periodontal patients and aggravating the vertical bone defects.4,7
Ghezzi in 2008 evaluated 14 patients who underwent guided tissue regeneration and afterwards, dental intrusion with orthodontics. They concluded that the stability achieved after orthodontic treatment was maintained. They also showed a reduction in probing depth, an increase in bone height and papilla thus reaffirming the possibility that a combined orthodontic-periodontal approach to avoid damage to the periodontal apparatus improves the aesthetics and stability in the patient.2
In 2013 Farzin Heravi et al. demonstrated that the use of fixed appliances may lead to different adverse side effects such as increased plaque retention or high incidence of caries caused because of the difficulty in eliminating plaque; in adult patients with non-controlled periodontal problems, dental movements are contraindicated, since the active disease causes vertical bone defects, periodontal pockets and loss of bony ridges.8
Ghezzi found that during incisor intrusion the gingiva moves in the same direction around 60% and the epithelium is always adhered to the cementoenamel junction, the clinical crowns are shortened and the depth of the gingival sulcus increases around 40% not because of inflammation or swelling, but due to the accumulation of gingival tissue. In intrusions of less than 5mm the epithelium will always remain attached to the cementoenamel junction so that with fiberotomy, the horizontal bone defect may change towards an angular form thus providing more stability.2,9
Erkan et al assessed the gingival response to intrusion of mandibular incisors and observed that the gingival margin and the mucogingival moved in the same direction as the teeth in 79 and 62% of the cases, respectively.5,9
Bellamy et al., in 2008 found that the use of circumferential supracrestal fiberotomy controls the reabsorption of marginal bone that may cause the creation of a cone-shaped bone defect that may cause different adverse side effects such as increased plaque retention or incidence of tooth decay caused by the difficulty in the mechanical removal of plaque; in adult patients with non-controlled periodontal problems intrusion movements are contraindicated because active disease causes vertical bone defects, periodontal pockets and loss of bony ridges.8
Bellamy in 2008 showed that the intrusion of healthy incisors in adult patients, moved apically the dentogingival complex in areas where the loss of alveolar bone and root resorption were minimal compared to other orthodontic movements.8,10
CONCLUSIONS- •
The results of this clinical case show that multi-disciplinary treatment (orthodontics and periodontics) is effective for ensuring long-term stability without relapse.
- •
It was decided to perform the dental intrusion through the use of orthodontics to realign and level the teeth as well as to improve the lengths of the clinical crowns and in this way the patient's aesthetics and confidence were restored.
- •
Orthodontic intrusion with light and continuous forces generates new periodontal tissue formation, increases alveolar bone and gingival insertion by eliminating the depth of periodontal pockets.
- •
Treatment success is closely related to patient cooperation since regular periodontal maintenance is required as well as good dental hygiene because without these, orthodontic movements are limited and may cause adverse effects.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia