The present article describes an epidemiological study of the prevalence of signs and symptoms of the temporomandibular joint disorder (TMJ) in 284 patients with malocclusion, first received in the Orthodontics Clinic of the Postgraduate Studies and Research Division (DePeI) of the National Autonomous University of Mexico (UNAM). The aim was to determine the prevalence of signs and symptoms of temporomandibular joint disorder in a sample of patients aged 12 to 68 years with malocclusion prior to orthodontic treatment and occlusal, skeletal and demographic variables. Among the results, it was found that one third of the sample had some sign or symptom of Temporomandibular Disorder, and there was no statistically significant difference between men and women. One out of three patients for both Class III and Class II presented some sign or symptom of TMD. Forty-two percent of the cases with open bite, and thirty two percent with cross bite had TMD. One out of four cases with TMD presented pain in the masticatory muscles.
El presente trabajo es un estudio epidemiológico de prevalencia de signos y síntomas de trastorno temporomandibular en 284 pacientes con maloclusión, recibidos por primera vez en la Clínica de Ortodoncia de la División de Estudios de Postgrado e Investigación de la Universidad Nacional Autónoma de México. El objetivo fue determinar la prevalencia de signos y síntomas del trastorno temporomandibular en una muestra de pacientes de 12 a 68 años con maloclusión previo al inicio del tratamiento de Ortodoncia y variables oclusales, esqueléticas y demográficas. Entre los resultados obtenidos se encontró que 1/3 de la muestra presentó algún signo o síntoma de trastorno temporomandibular, y no existió diferencia estadística significativa entre hombres y mujeres, 1 de cada 3 pacientes tanto de Clase III como de Clase II presentó algún signo o síntoma de TTM. El 42% de los casos con mordida abierta, así como el 32.5% de mordida cruzada presentaron TTM. 1 de cada 4 de los casos con TTM presentó dolor en músculo masticatorio.
The temporomandibular joint disorder (TMJ) has been appointed with several terms; in 1934 James Costen described some symptoms relating to the ear and to the Temporomandibular Joint that were given the name of Costen syndrome. There are also other terms such as TMJ syndrome, temporomandibular joint dysfunction, which was coined by Shore in 1959, functional alterations of the temporomandibular joint by Ramfjord and Ash in 1971, Occluso-mandibular Disorder, Mio arthropathy of the temporomandibular joint, pain dysfunction syndrome, among others. In 9182 Bell appointed the name temporomandibular joint disorder which was adopted by the American Dental Association in 1983 and is used to describe the functional alterations of the masticatory system.1–3
The Epidemiology studies the distribution and determinants of events (particularly, diseases) related to health and the application of these studies to disease control and other health problems.4 Epidemiological studies determine the frequency and distribution of diseases. If the signs and symptoms of TMD are common in the general population, the TMD becomes an important issue that must be addressed.1,3
The literature has reported malocclusion to be one of the causes of TMD and on other occasions it has been described as only a predisposing factor. This situation has led to the conduction of epidemiological studies in which the prevalence of TMD is related to several types of malocclusion.5
RATIONALEThe importance and extent of TMJ disorders presents us with the need to know data for determining the frequency and distribution of this disorder in Mexican population in order to be able to understand it in a more comprehensive way and address the diagnosis and treatment of this ailment more effectively.
OBJECTIVETo determine the prevalence of signs and symptoms of TMJ disorders and its association with occlusal, skeletal and demographic variables in a sample of patients, ages 12 to 68 years, who had a malocclusion prior to the start of orthodontic treatment and who sought care at the Orthodontics clinic of the DePeI during 2010-2012.
MATERIAL AND METHODSThe population chosen for the study was 1,098 Mexican patients with malocclusion received at the Orthodontics Clinic of the UNAM by the 24 residents of the specialty of Orthodontics between November 2010 and May 2012.
The applied exclusion criteria were: patients with a diagnosis of rheumatoid arthritis, patients with diminished intellectual or motor capacity unable to answer the anamnesis by themselves, patients with any kind of prior joint surgery, pregnant patients, patients who did not complete the clinical examination and/or the anamnesis and patients with fixed or removable orthodontic appliances at the time of clinical evaluation. The final sample consisted of 284 cases.
The clinical examination of the temporomandibular disorder's signs and symptoms was based on the one described by Jeffrey Okeson. The classification for determining the kind of TMJ disorder was Dr. Welden Bell's.
The type of study was retrospective, cross-sectional and did not pose any danger for the patients. The statistical analysis was performed with the IBM program SPSS 20.
RESULTSThe prevalence of temporomandibular disorders in a Mexican population with malocclusion was 29.9% (n= 85), which means that one out three patients with malocclusion had some sign or symptom of TMD (Figure 1).
The existence of signs and symptoms of TMD was slightly greater in men, with 31.7% (n = 33), and 28.8% (n = 52) for women, although no statistically significant difference was found (Figure 2).
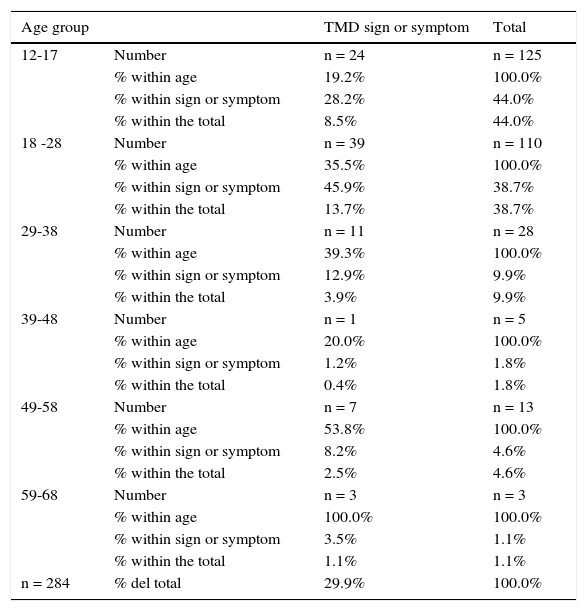
The age group with the highest prevalence of TMD was 59 to 68 years with 100% (n = 3) of the cases within their group, which represents 1.1% of the sample, followed by the group of 49 to 58 years with 53.8% (n = 7) of the cases within their age group and 2.5% of the sample. In third place was the group of 18 to 28 years since for every 3 young people, one showed some sign or symptom of TMD, representing 13.7% (n = 39) of the total sample (Table I).
TMD prevalence per age group.
| Age group | TMD sign or symptom | Total | |
|---|---|---|---|
| 12-17 | Number | n = 24 | n = 125 |
| % within age | 19.2% | 100.0% | |
| % within sign or symptom | 28.2% | 44.0% | |
| % within the total | 8.5% | 44.0% | |
| 18 -28 | Number | n = 39 | n = 110 |
| % within age | 35.5% | 100.0% | |
| % within sign or symptom | 45.9% | 38.7% | |
| % within the total | 13.7% | 38.7% | |
| 29-38 | Number | n = 11 | n = 28 |
| % within age | 39.3% | 100.0% | |
| % within sign or symptom | 12.9% | 9.9% | |
| % within the total | 3.9% | 9.9% | |
| 39-48 | Number | n = 1 | n = 5 |
| % within age | 20.0% | 100.0% | |
| % within sign or symptom | 1.2% | 1.8% | |
| % within the total | 0.4% | 1.8% | |
| 49-58 | Number | n = 7 | n = 13 |
| % within age | 53.8% | 100.0% | |
| % within sign or symptom | 8.2% | 4.6% | |
| % within the total | 2.5% | 4.6% | |
| 59-68 | Number | n = 3 | n = 3 |
| % within age | 100.0% | 100.0% | |
| % within sign or symptom | 3.5% | 1.1% | |
| % within the total | 1.1% | 1.1% | |
| n = 284 | % del total | 29.9% | 100.0% |
The prevalence of Class I malocclusion was 44.4% (n = 126), for Class II, 40% (n = 114) and for Class III, 15.5% (n = 44) (Table II). In relation to TMD, 1 of every 3 patients showed some sign or symptom of TMD, both in Class II (32.4%, n = 37) and Class III (36.3%, n = 16) cases, whereas for Class I, only 1 of every 4 (25.3%, n = 32) presented them (Table II).
Cross bite was present in 44.3% (n = 126) of the patients from whom 1 of every 3 showed some sign or symptom of TMD (14%, n = 41). From the cases who had cross bite and TMD, 41.4% (n = 17) of them had anterior cross bite, 36.5% (n = 15) had unilateral posterior cross bite and 21.9% (n = 9) were cases with bilateral posterior cross bite, which represent the 5.9, 5.2 and 3.1% respectively of the total sample (Table III).
The prevalence of open bite in the sample was 7.3% (n = 21). Forty-two percent of the open bite cases showed signs and symptoms of TMD. 2.4% (n = 7) of the patients had anterior open bite and TMD, this represents 50% of the anterior open bites. Only 25% (n = 1) of the unilateral posterior open bites and 30% (n = 1) of the bilateral posterior open bites also had some signs or symptoms of TMD, which represents a 0.3 and 0.3% of the total sample respectively (Table VI).
Twenty-six percent (n = 22) of the cases with TMD presented pain in some masticatory muscle.
In relation to the overjet, the largest percentile prevalence with TMD was concentrated in the range of more than -2 to -0.1mm overjet since 47.5% (n = 19) of this group presented TMD, followed by the range of > 6.1mm with a 47% (n = 8) and in third place, the range from 4.1 to 6mm with 29.5% (n = 13), representing 6.6, 2.8 and 4.5% respectively of the total sample. The overbite range with higher prevalence of TMD was the one with less than -2 to -0.1mm since 50% (n = 24) of the cases in that range presented some sign or symptom, followed by the range of 4.1 to 6mm with 31% (n = 12) and in third place, the range from 2.1 to 4mm with 28.5% (n = 24), which accounted for 8.4, 4.2 and 8.4% of the total sample respectively (Table VandFigure 3).
contingency table, TMD prevalence in overjet and overbite.
| Overjet | Overbite | ||||
|---|---|---|---|---|---|
| Total | TMD | Total | TMD | ||
| Overlap | < -6.1 | 0 | 0 | 1 | 0 |
| -6.0 a -4.1 | 0 | 0 | 3 | 0 | |
| -4.0 a -2.1 | 10 | 0 | 5 | 1 | |
| -2.0 a -0.1 | 40 | 19 | 48 | 24 | |
| 0.0 – 2.0 | 79 | 23 | 93 | 21 | |
| 2.1 – 4.0 | 91 | 21 | 84 | 24 | |
| 4.1 – 6.0 | 44 | 13 | 38 | 12 | |
| > 6.1 | 17 | 8 | 9 | 2 | |
| Total | 281 | 84 | 281 | 84 | |
Total sample = 284. lost = 3.
The present study TMD prevalence was 29.9%. In studies such as the one by Tanne in patients of 4-29 years of age before orthodontic treatment with and without cleft lip and palate, the report was of 18.5-19.4%. Gonçalvez reported 39.2% of TMD in the general population of persons aged 15-65 years; Runge reported a 36.3% in teenage and adult patients seeking orthodontic treatment.5–7
However, there are reports in the literature ranging from a 16 to 59% prevalence of TMD symptoms, and 33 to 86% for signs of TMD.6,8,9
No statistically significant difference was found between men and women, which is consistent with studies in Asian populations, while studies on western populations reported a higher prevalence in women.6,9,10
It was found that 26% of the sample had muscle pain. Riolo reported 17% prevalence in patients aged 6-19 years, Gonçalvez 15.4%, Dibbets 5% in adolescents and 21% in the same patients 14 years after orthodontic treatment, while Tanne reported only 3%.5,6,11
Class III patients showed a higher prevalence of TMD, in skeletal patients 36.3% and in those cases of overjet within the range of -2 to -0.1mm, 47.5%.
In terms of vertical overbite, open bite in a range of -2 to 0.1mm showed the highest prevalence with 50% of the cases in that group, followed in second place by deep bite in a range of 4.1mm to 6mm with the 31%.
Comparatively between anterior and posterior cross bite, anterior open bite presented a higher prevalence of TMD with a 5.9 and 3.1% respectively.
The variations reported in different epidemiological studies of temporomandibular disorders are due to differences in sampling, criteria, and methods for the collection of information among other things, which causes comparisons between studies to be not quite reliable or have certain limitations. However, they allow us to observe certain trends and ranges of matches.
CONCLUSIONSIn patients with malocclusion the study yielded a significant prevalence of temporomandibular disorders.
It is important to know that a percentage of our patients will present this kind of condition. We should be able to recognize and diagnose them in a timely manner to provide the pertinent treatment to each and every one of our patients.
Orthodontics Specialty Resident, Division of Postgraduate Studies and Research (DePeI), National Autonomous University of Mexico (UNAM).
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Professor at the Orthodontics Department, Division of Postgraduate Studies and Research (DePeI), National Autonomous University of Mexico (UNAM).
Professor of the Department of Preventive Dentistry and Public Health, Faculty of Dentistry, National Autonomous University of Mexico (UNAM).