Early treatment of skeletal Class III patients is usually handled with the use of maxillary protraction face mask. The results of this orthopedic therapy are often accompanied by adverse dentoalveolar effects. An alternative treatment is skeletal anchorage comprised of temporary anchorage devices (TADs), which uses two titanium plates fixed with mini implants placed in the zygomatic process of the maxilla and two side plates between the lower canine and right and left and the use of intermaxillary elastics. This results in maxillary advancement and improvement of facial aesthetics while reducing dentoalveolar adverse effects.
El tratamiento temprano de pacientes clases III esqueletal generalmente se maneja con el uso de la máscara facial de protracción maxilar, en el cual los resultados de esta terapia ortopédica frecuentemente son acompañados de efectos dentoalveolares desfavorables. Una alternativa de tratamiento es el anclaje esquelético comprendido de dispositivos de anclaje temporal, el cual utiliza dos placas de titanio fijadas con mini-implantes colocadas en los procesos cigomáticos de los maxilares y dos placas entre el lateral y canino inferior derecho e izquierdo, además del uso de elásticos intermaxilares, obteniendo como resultado un avance maxilar y mejoramiento de la estética facial y disminuyendo los efectos dentoalveolares desfavorables.
Maxillary protraction with the use of facemask at early ages is the treatment of choice for skeletal class III patients. Such treatment generates a positive overjet through the combination of dentoalveolar and skeletal movements, since the forces are applied mainly to the teeth 12 to 16hours per day for 9 to 12 months, causing undesirable effects.1
Short-term studies of maxillary protraction have shown only limited effects on mandibular advancement (2-3mm on average) in addition to a posterior mandibular rotation and dentoalveolar changes (proclination of the maxillary incisors, mesialization and extrusion of maxillary molars and retroclination of mandibular incisors).2 Long-term results of maxillary protraction indicate that there is a relapse rate of 25%- 33% of patients which presented a negative overjet relapse. In this kind of treatment orthopaedic effects must be maximized since dentoalveolar changes are those that present the greatest relapse.3
However, a small number of patients with skeletal class III problems will ultimately require orthognathic surgery, which is why any treatment that can eliminate or reduce the extent of the problem is of great help.4
Skeletal anchorage in growing patientsIn recent years there has been an increase in the use of temporary anchorage devices (TADs), which are often used in orthognathic surgery and fracture fixation. Skeletal anchorage devices have been used successfully in orthodontics to achieve multiple movements such as dental intrusions, open bite correction, molar distalization, etc. and in recent studies they have been given applications in orthopaedic treatments.5
Kokich in 1985 introduced the use of absolute anchorage to achieve maxillary protraction. He used protraction forces with the use of a facemask and intentionally used as anchorage anquilosed deciduous canines with the aim of treating a patient with maxillary deficiency.6 Afterwards, Smalley experimented with osseointegrated implants for the maxillary protraction in monkeys using a force of 600g per side to stimulate circumaxillary sutures. An anterior displacement of 8mm was obtained.7 Singer placed mini implants in the zygomatic processes of the maxillae implementing 400g of force to a child with sequelae of cleft lip and palate (maxillary retrusion) thus obtaining as a result a maxillary advancement of 4mm as well as a descent due to the vector of force application. Additionally, an improvement in the patient's profile was caused by a posterior mandibular rotation.8
Indications for skeletal anchorageTADs as skeletal anchorage are used in skeletal class III patients with hypoplasia of the maxilla determined by cephalometric analysis and soft tissue profile evaluation, in addition to presenting molar class III and negative overjet. These patients must be between the ages of 9 to 14 years in a pre-pubertal period.9
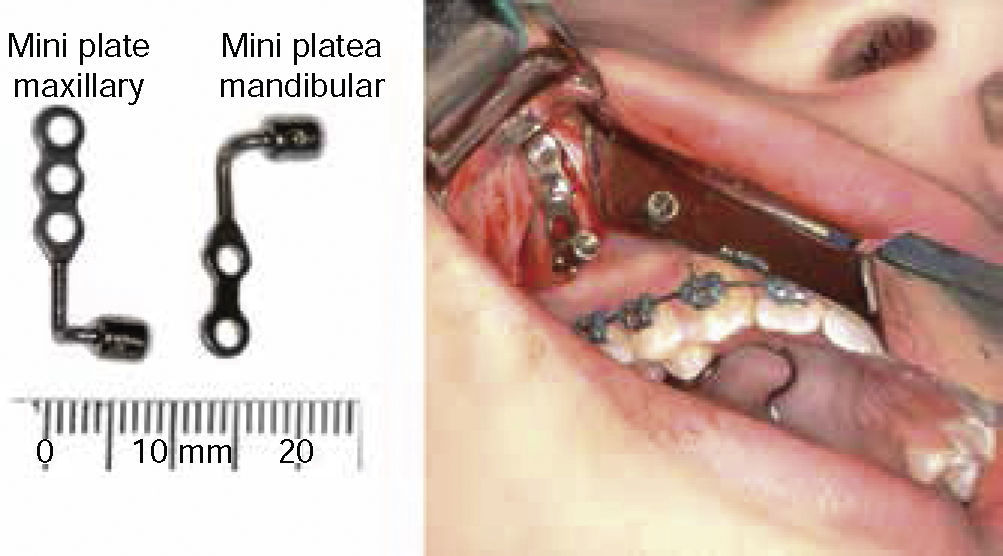
The surgical procedure described by Dr. Hugo De Clerck consists in the placement of four mini plates placed in each one of the maxillary zygomatic processes. The mini plates are going to generate a force vector that passes through the nasomaxillary complex stimulating the circumaxillary sutures. In the lower arch one mini plate is placed on each side of the anterior region of the mandible between the right and left permanent lateral incisor and permanent canine. Fixation of the plates is achieved with three mini implants for the maxilla and two for the mandible. In order to perform a correct positioning of the lower plates it must be to certain that the canine has already erupted so as to prevent any damage when inserting the mini implant (Figure 1). One should wait 2 to 3 weeks for the process of tissue healing and afterwards, apply orthopedic forces.10
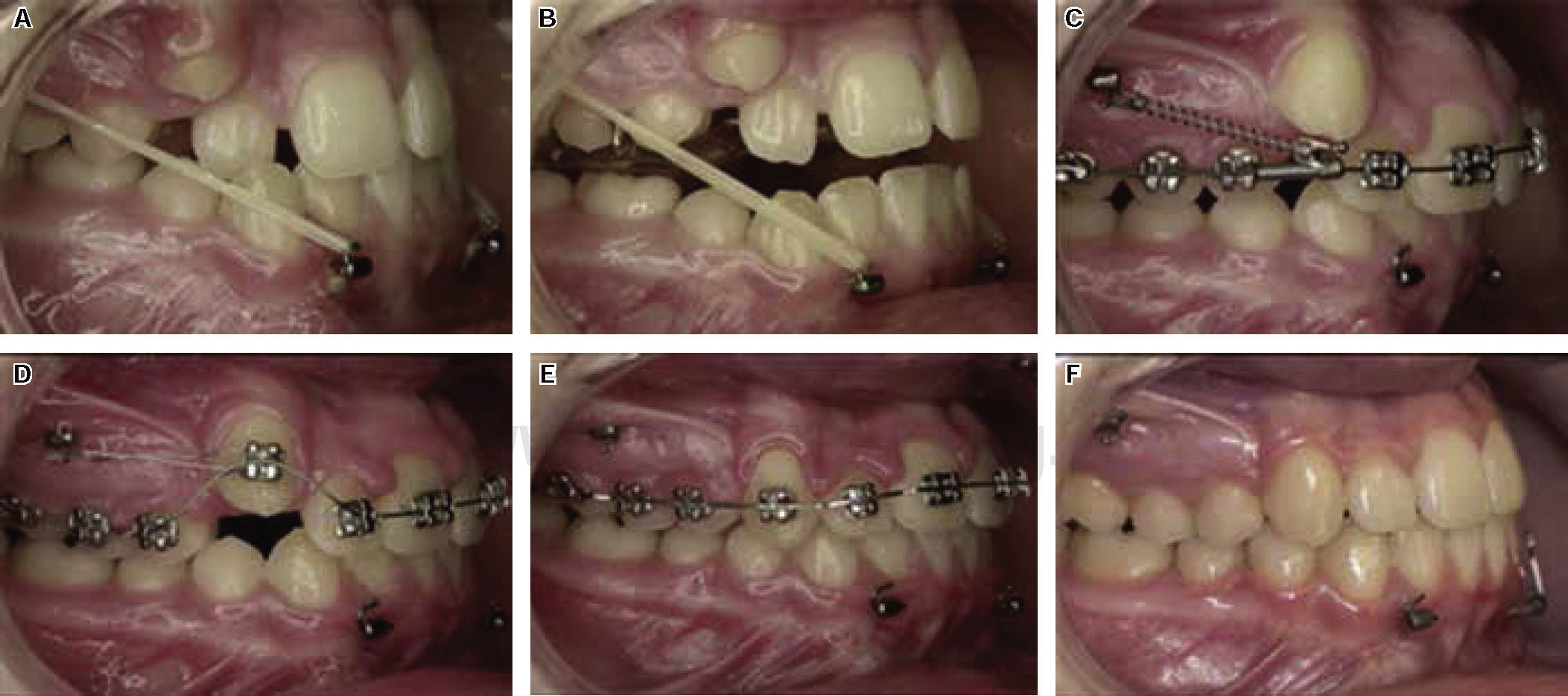
The orthopedic protocol mentions that after three weeks one must apply intermaxillary elastics on each side with a class III force vector, which will move the maxilla forward and downwards and the mandible backwards and upwards (Figure 2). The initial elastics must exert a force of 150g on each side and after the first month it will increase to 250 grams with the same vector. To determine the force the patient must be at maximum intercuspation. The duration of orthopedic traction is 12.5 months with a range of 9 to 14 months of 24 hour use. An acrylic plate or placement of resin stops to increase vertical dimension and achieve overjet might also be used. The orthodontist will determine the ideal time to remove the elastics, usually upon achieving a positive overjet.9
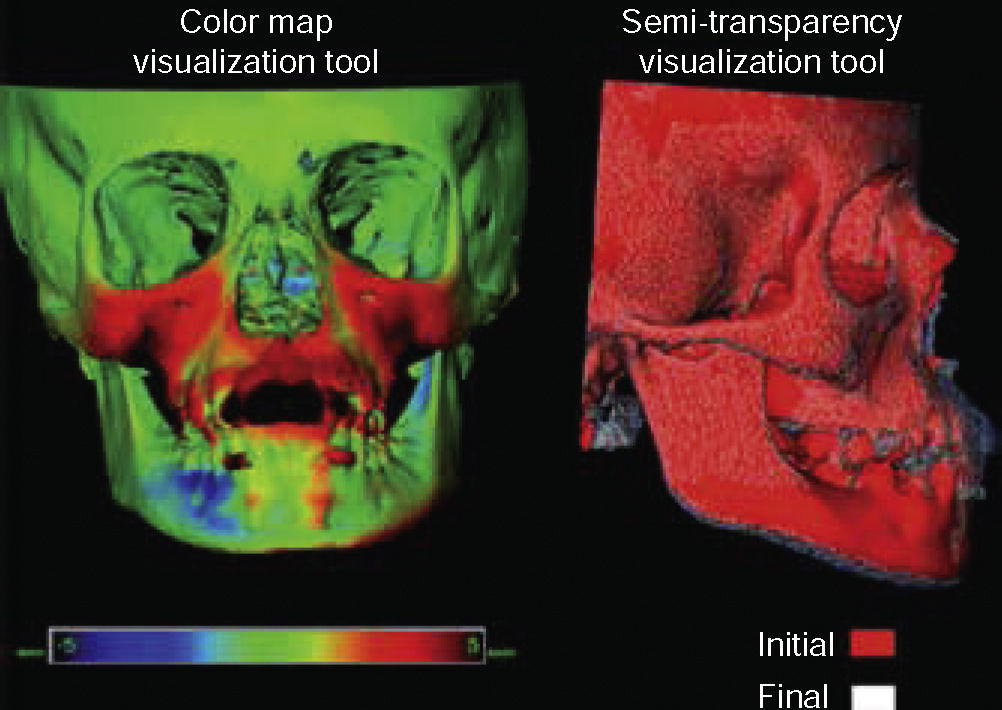
To perform an accurate positioning of the plates a cone beam CT scan (CBCT) must be used for detecting the most calcified areas of the zygomatic process of the maxilla for proper mechanical retention of the mini implants. The best plate stability is achieved in patients of at least 11 years of age. Additionally, the use of CBCT may be useful to assess maxillary advancement in this kind of treatment before (T1) and a year after setup of orthopedic mechanics (T2), with the aid of super impositions of three-dimensional images and evaluating the actual progress of maxillary protraction (Figure 3).
CBCT images must assess the following anatomical regions:
- 1)
Anterior region of the maxilla (point A)
- 2)
Zygomatic process of the maxilla
- 3)
Most anterior region of the mandible (pogonion)
- 4)
Anterior and posterior surface of the condyles
- 5)
Lower ridge of the mandible
- 6)
Glenoid fossa
- 7)
Soft tissues11
It has been clinically proven that the continuous forces exerted by the intraoral intermaxillary elastics over TADS in skeletal class III patients have better results than the use of intermittent forces of extraoral elastics with the facemask.12
Generally patients who are skeletal class III with an antero-posterior deficiency of the maxilla lack space for canine eruption, that is why once overjet is achieved molar and premolar distalization movements may be perform to obtain space and thus position the canines in the arch (Figure 4).
DISCUSSIONOrthopedic procedures with the use of skeletal anchorage in growing patients offers major advantages regarding aesthetics, function and long term stability. The use of intermaxillary elastics improves facial and skeletal relations in addition to diminishing the effects that cause dentoalveolar relapse. In some cases the implementation of this technique may be sufficient to avoid orthognathic surgery in the future or at least reduce the severity of the surgical correction after the patient has completed growth. Growing patients who undergo this procedure easily adapt to the aesthetic changes that are gradually manifested unlike orthognathic surgery post-surgical changes which occur almost immediately.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia