Root resorption is a complication of orthodontic treatment that may occur in various degrees of severity. However, considerable root resorption can also be appreciated in patients where root development has been interrupted by different circumstances during the orthodontic treatment. A 9-year-old female patient was admitted after being in a treatment with fixed appliances for 3 years. She presented clinical features of anterior open bite and the radiographic evaluation showed important root resorption of the four maxillary incisors. It was decided to use a more conservative approach instead of fixed appliances during the initial phase of treatment and a myofunctional therapy was chosen. Assessment of the upper airways was performed before placing a tongue crib accompanied by exercises of the orbicularis oris muscle complex, after one month of follow-up appointments, bite closure was obtained. Chances of relapse are reduced with appropriate growth guidance and changes in the muscular behavior of young patients.
La reabsorción radicular es una complicación que se puede presentar en el tratamiento ortodóncico en diversos grados. Asimismo, en pacientes cuyo desarrollo radicular es interrumpido por diferentes causas puede observarse un acortmiento radicular. Fue admitida una paciente femenina de 9 años de edad después de un tratamiento interceptivo de 3 años de duración, que presentó características clínicas de mordida abierta anterior. En la valoración radiográfica se observó un acortamiento considerable de los cuatro incisivos superiores. Se tomó la decisión de no colocar aparatología fija de forma inicial y abordar el problema con una terapia muscular funcional. Después de evaluar la permeabilidad de las vías aéreas superiores, se colocó una trampa de lengua y mediante ejercicios peribucales se consiguió cerrar la mordida tras un mes de citas de control. Al guiar el crecimiento esquelético y modificar el comportamiento muscular del paciente se reduce la posibilidad de recidiva.
Root shortening, a specific type of external root resorption, is an orthodontic treatment complication that occurs in mild degrees on most occasions in patients who undergo important orthodontic movements. However, it is rare that such reabsorption is severe enough to create a clinical problem. Currently, it has not been reported in the literature the spontaneous loss of a dental organ due to the root resorption by iatrogeny.
External apical root resorption is the loss of root structure involving the apical region to such a degree that can it be detected by means of dentoalveolar radiographs. The reabsorption can be physiological, as is the exfoliation of temporary teeth, or pathologic, when it affects permanent teeth. It may be defined as a defense mechanism by which the body responds to external or internal stimuli and takes place in hard tissues.1 External root resorption is probably the most common sequelae of orthodontic treatment, because forces applied on teeth in a short period of time may produce root resorption.2
Root resorption associated with orthodontic treatment is more evident in patients on whom heavy, long-term and in an adverse direction forces, were applied or when the tooth is not capable of withstanding normal forces due to a deterioration of the support system by factors such as pressure of the adjacent teeth, periodontal inflammation, periapical inflammation, tooth reimplantation, severe occlusal trauma, dentoalveolar trauma with partial or total avulsion, tumors and cysts, endocrine and metabolic disorders or idiopathic factors.3,4 In addition, the severity and type of malocclusion are important factors that must be taken into consideration since it has been observed that an increased overjet and open bites have a greater risk of root resorption.5,6
Classic orthodontics consists of fixed appliances for solving dental malocclusions, but sometimes it is better to use functional forces instead of stronger mechanics. Continuous and heavy forces produce greater root resorption by the generated friction and the recovery inability of the periodontal ligament.4
BackgroundAt the beginning of the last century, the orthodontic community was shocked by the root damage that may occur due to orthodontic movement.1 The condition was more evident in subjects where the forces applied on the teeth were strong and applied for long periods of time, in inadequate directions or in individuals whose teeth were unable to withstand normal forces due to the weakening of the support system. Root resorption was located in the outer surface of the root and could be observed in the cervical, middle and apical thirds.3,4
Controversy exists in clinical and laboratory research reports on root resorption compared to the incidence and amount of external apical root resorption. The mean for root resorption varies from 0.2mm to 2.93mm, while the prevalence of radiographic detectable resorption varies from 0 to 100%.7-9 Such controversies may be attributed to the considerable differences in the studied tooth type, sample sizes, follow-up duration, type of dental movement, measurement methods and patient’s characteristics.1
The etiology of root resorption has two phases: a stimulus and a re-stimulation. In the first phase, the stimulus affects non-mineralized tissues, such as the precement or cementhoid tissue which covers the external root surface. This stimulus may be mechanical (by dental trauma or orthodontic treatment) or chemical (dental bleaching with high concentrations of hydrogen peroxide).2
The exposed mineralized tissue is colonized by multinucleated cells, which initiate the resorption process. However, if there are no more stimuli to the reabsorbing cells, the process will end spontaneously. The repair with cement will happen in two to three weeks, if the affected surface does not involve a large area. If the affected area is large, the cells have the ability to invade the root before the cementoblasts can colonize the surface and generate anchylosis. In the second phase, the continuation of the resorption process depends on continuous odontoclasts stimulation or re-stimulation by infection or pressure.2
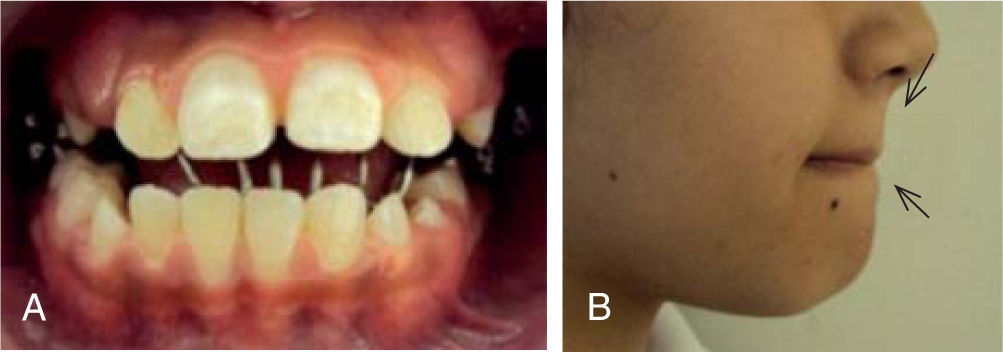
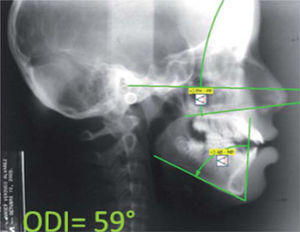
Case reportFemale patient, 9 years of age, attends the Orthodontics Clinic at the Postgraduate Studies and Research Division of the National Autonomous University of Mexico. Upon interrogation, the patient’s mother explained that the patient underwent a previous orthodontic treatment for 3 years to correct the anterior open bite. Her chief concern was the relapse of the anterior open bite four months after appliance removal. Upon clinical examination, a convex profile, chin muscles hypertonicity, anterior open bite and atypical swallowing were observed accompanied by a mouth-breathing habit.
Initial recordsExtra and intraoral photographic records were obtained (Figures 1and2) as well as cast study models. Clinically, an anterior open bite in the mixed dentition stage was observed. It was also observed during clinical examination that the patient showed a tongue thrusting and mouth breathing habit. The lower facial third was increased and chin muscle hypertonicity was observed at lip closure.
In the radiographic assessment, an important root shortening was observed in the upper incisors producing a 1:2 crown-root ratio (Figure 3). In the lateral head film, lip incompetence was confirmed and narrow upper airways were noted so a medical consultation with an otorhinolaryngologist was suggested to rule out a possible upper airway obstruction (Figure 4).
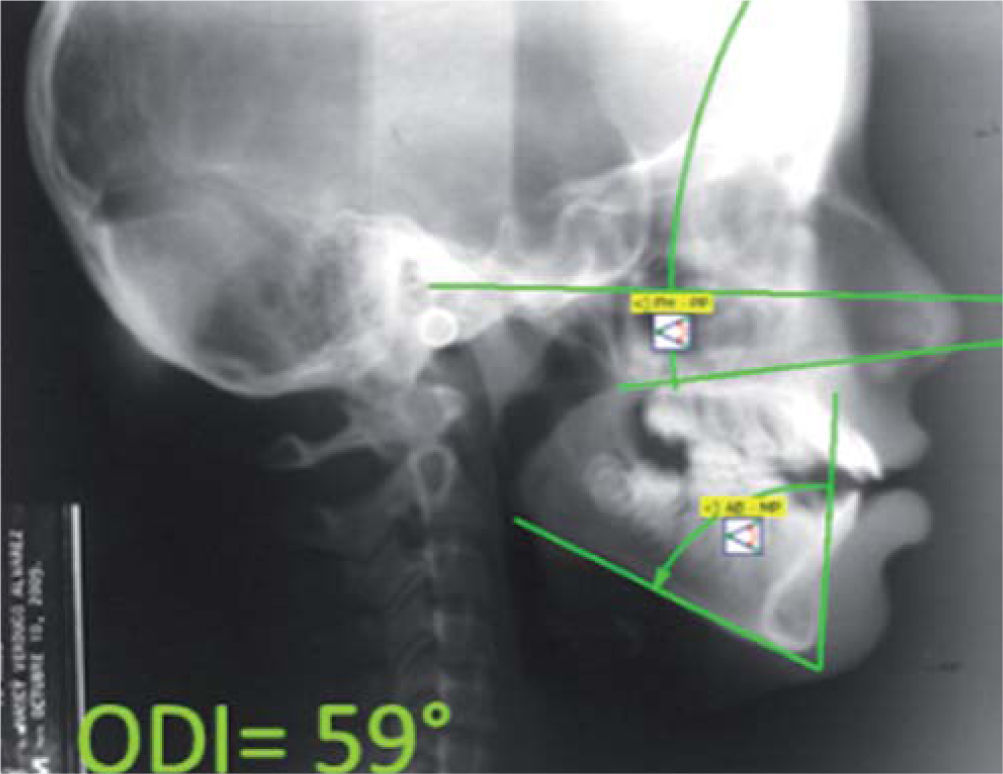
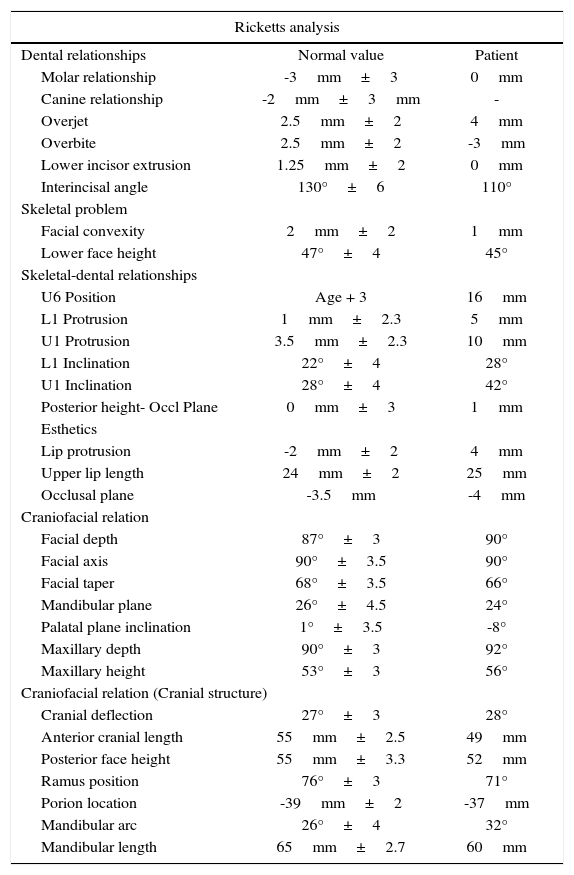
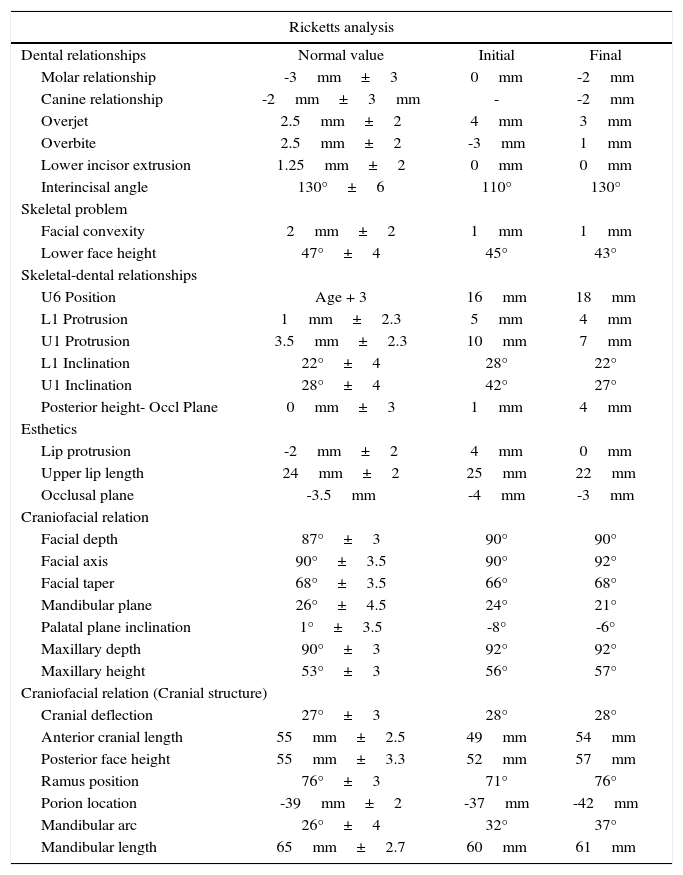
The patient was diagnosed as a skeletal class I with anterior open bite due to an hyperdivergent mandible and severe incisor proclination according to Ricketts cephalometric analysis (Table I). To make the analysis more complete, we decided to measure the overbite depth indicator (ODI), which is a specific method to assess open bite. It was proposed by Dr. Kim,10 and it is obtained from the difference between the mandibular plane-AB plane angle and the Frankfort plane-palatal and plane angle. Normal values are 74.5°±6. The patient’s ODI showed an open bite tendency with a 59 degrees negative value compared to the norm (Figure 5).
Initial patient values for the Ricketts cephalometric analysis.
| Ricketts analysis | ||
|---|---|---|
| Dental relationships | Normal value | Patient |
| Molar relationship | -3mm±3 | 0mm |
| Canine relationship | -2mm±3mm | - |
| Overjet | 2.5mm±2 | 4mm |
| Overbite | 2.5mm±2 | -3mm |
| Lower incisor extrusion | 1.25mm±2 | 0mm |
| Interincisal angle | 130°±6 | 110° |
| Skeletal problem | ||
| Facial convexity | 2mm±2 | 1mm |
| Lower face height | 47°±4 | 45° |
| Skeletal-dental relationships | ||
| U6 Position | Age + 3 | 16mm |
| L1 Protrusion | 1mm±2.3 | 5mm |
| U1 Protrusion | 3.5mm±2.3 | 10mm |
| L1 Inclination | 22°±4 | 28° |
| U1 Inclination | 28°±4 | 42° |
| Posterior height- Occl Plane | 0mm±3 | 1mm |
| Esthetics | ||
| Lip protrusion | -2mm±2 | 4mm |
| Upper lip length | 24mm±2 | 25mm |
| Occlusal plane | -3.5mm | -4mm |
| Craniofacial relation | ||
| Facial depth | 87°±3 | 90° |
| Facial axis | 90°±3.5 | 90° |
| Facial taper | 68°±3.5 | 66° |
| Mandibular plane | 26°±4.5 | 24° |
| Palatal plane inclination | 1°±3.5 | -8° |
| Maxillary depth | 90°±3 | 92° |
| Maxillary height | 53°±3 | 56° |
| Craniofacial relation (Cranial structure) | ||
| Cranial deflection | 27°±3 | 28° |
| Anterior cranial length | 55mm±2.5 | 49mm |
| Posterior face height | 55mm±3.3 | 52mm |
| Ramus position | 76°±3 | 71° |
| Porion location | -39mm±2 | -37mm |
| Mandibular arc | 26°±4 | 32° |
| Mandibular length | 65mm±2.7 | 60mm |
A lingual stainless steel grid was placed in the upper arch as a reminder for the correction of the lingual thrust. Exercises of the perioral musculature were instructed, pressing the anterior segment of the dental arches to correct the anterior open bite as well as the mouth breathing habit (Figure 6). Control appointments were scheduled monthly to assess changes in both dental and lip position.
After the first month of treatment, complete closure of the anterior open bite was observed and it was decided to postpone as much as possible the placement of fixed appliances in the upper arch until dental stability of the upper anterior teeth was obtained. There was a decrease of the lower facial third after achieving closure of the anterior open bite. When an adequate overbite was achieved, 018-slot Edgewise appliances were placed in the lower arch to begin dental alignment. Once the upper permanent canines erupted, we placed appliances in the upper arch without including the four upper incisors. A 0.135 Flex Twist archwire was used (Figure 7).
Once the alignment of the upper canines, was achieved was 0.016 steel Utility type archwire was used in the anterior segment. Three months after we decided to place appliances in the upper incisors and 0.135 flex Twist previously formed archwire (Figure 8).
During the entire treatment, orofacial myofunctional exercises were maintained and a periodical radiographic control of the upper incisors was performed for evaluation of any modification of their root anatomy. Once dental stability, was observed, it was decided to place a 0.016×0.016 steel archwire with a bend for negative root torque on the upper incisors (Figure 9).
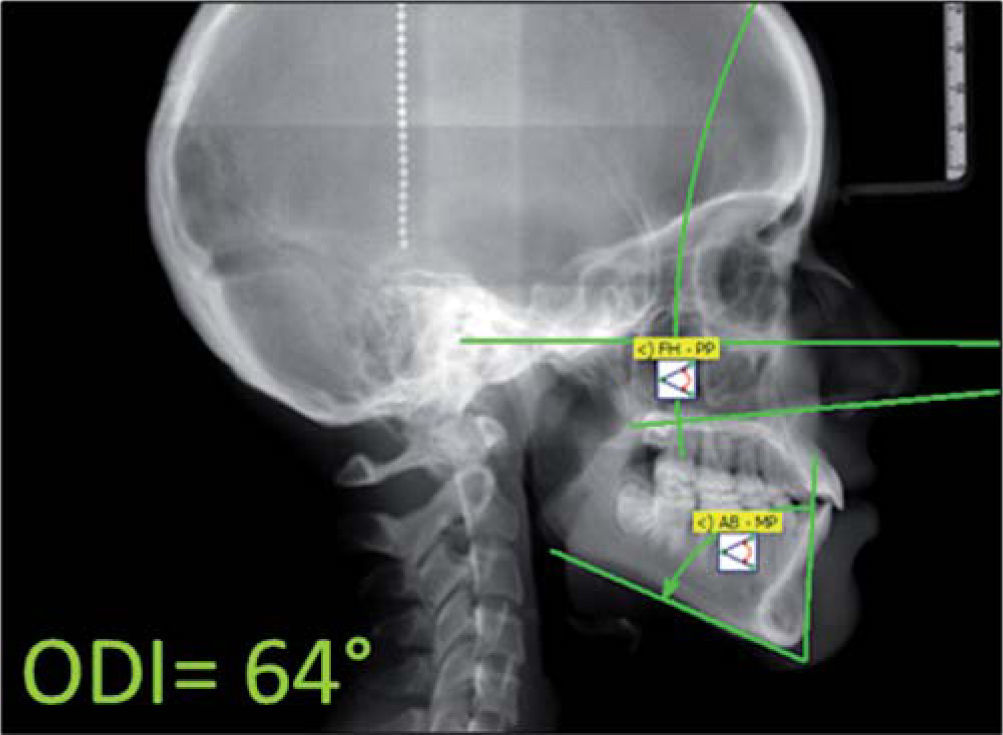
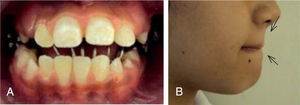
The bite correction was maintained during the following appointments until appliance removal was decided. For retention, a circumferential retainer was placed with an acrylic coat for the labial portion of the incisors both on the upper and lower arches. The final radiographic evaluation showed a significant change in the direction of mandibular growth as well as in the incisor position (Figure 10). Also, a new cephalometric analysis was performed to compare the results with initial cephalometric values (Table II). Significant changes were found in regard to incisor inclination and protrusion and in the soft tissues. Once again the ODI was used to compare the skeletal changes obtained with treatment and there was a positive change in the ODI value, very close to normal values value (Figure 11). Dental and skeletal changes were reflected in the patient’s facial appearance where a favorable change in profile and smile could be observed (Figure 12).
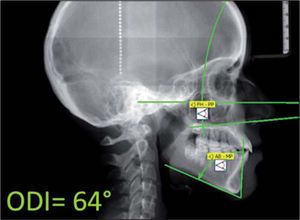
Initial and fi nal cephalometric values.
| Ricketts analysis | |||
|---|---|---|---|
| Dental relationships | Normal value | Initial | Final |
| Molar relationship | -3mm±3 | 0mm | -2mm |
| Canine relationship | -2mm±3mm | - | -2mm |
| Overjet | 2.5mm±2 | 4mm | 3mm |
| Overbite | 2.5mm±2 | -3mm | 1mm |
| Lower incisor extrusion | 1.25mm±2 | 0mm | 0mm |
| Interincisal angle | 130°±6 | 110° | 130° |
| Skeletal problem | |||
| Facial convexity | 2mm±2 | 1mm | 1mm |
| Lower face height | 47°±4 | 45° | 43° |
| Skeletal-dental relationships | |||
| U6 Position | Age + 3 | 16mm | 18mm |
| L1 Protrusion | 1mm±2.3 | 5mm | 4mm |
| U1 Protrusion | 3.5mm±2.3 | 10mm | 7mm |
| L1 Inclination | 22°±4 | 28° | 22° |
| U1 Inclination | 28°±4 | 42° | 27° |
| Posterior height- Occl Plane | 0mm±3 | 1mm | 4mm |
| Esthetics | |||
| Lip protrusion | -2mm±2 | 4mm | 0mm |
| Upper lip length | 24mm±2 | 25mm | 22mm |
| Occlusal plane | -3.5mm | -4mm | -3mm |
| Craniofacial relation | |||
| Facial depth | 87°±3 | 90° | 90° |
| Facial axis | 90°±3.5 | 90° | 92° |
| Facial taper | 68°±3.5 | 66° | 68° |
| Mandibular plane | 26°±4.5 | 24° | 21° |
| Palatal plane inclination | 1°±3.5 | -8° | -6° |
| Maxillary depth | 90°±3 | 92° | 92° |
| Maxillary height | 53°±3 | 56° | 57° |
| Craniofacial relation (Cranial structure) | |||
| Cranial deflection | 27°±3 | 28° | 28° |
| Anterior cranial length | 55mm±2.5 | 49mm | 54mm |
| Posterior face height | 55mm±3.3 | 52mm | 57mm |
| Ramus position | 76°±3 | 71° | 76° |
| Porion location | -39mm±2 | -37mm | -42mm |
| Mandibular arc | 26°±4 | 32° | 37° |
| Mandibular length | 65mm±2.7 | 60mm | 61mm |
Six months after orthodontic treatment, a clinical exam was conducted to assess the patient’s occlusal condition as well as retainer use. We observed an improvement in dental interdigitation compared to the day of appliance removal (Figure 13). Also, an adequate lip competence was observed and the absence of the atypical swallowing habit that the patient showed at the beginning of treatment (Figure 14).
DiscussionIn spite of the fact that open bite is known to have a multifactorial etiology, the muscular factor is without doubt one of the most important that must be taken into consideration. In this particular case, muscle function from both the masticatory complex and the tongue was affected resulting in an anterior open bite.
According to Lieberman and Gazit,11 one of the predisposing factors for open bite is tongue activity, either as passive or active thus becoming one of the etiological factors of this malocclusion. A modified lingual posture interferes with respiratory function and has an important role in the development of an anterior open bite. These two situations (lingual posture and respiratory function) are an important factor combination that must be controlled before, during and after orthodontic treatment.
Patients with atypical swallowing mainly use facial muscles to perform suction instead of swallowing. The specialist in communication disorders Ann Beard Ehrlich discovered that whencorrecting a pattern of atypical swallowing, one should focus on voluntary change of habits thus becoming easier to control. The patients is shown the right way in which masticatory muscles must be used, and also the correct position in which the tongue must be placed during swallowing.12
Myofunctional therapy benefits the patient, since in addition to having an effect on the open bite, abnormal habits are corrected and the tonicity of the orbicularis oral muscles is improved which in turn allow lip competence.13-15 It also achieves better nasal flow, which favorably affects muscular posture and other functions.
There are several treatments for anterior open bite such correction sucha as molar intrusion,16 bicuspid extractions,17 and orthognatic surgery.18 Molar intrusion has been among the most used method for the correction of this kind of malocclusion. Due to the difficulty in obtaining true molar intrusion through the use of traditional biomechanics, nowadays the use of micro-implants has demonstrated greater effectiveness for open bite correction.16,17,19
In other cases it is often resorted to extraction of the first and second premolars due to their high overbite stability after orthodontic treatment.17 However, vertical changes are more noticeable with second premolar extractions and therefore they are recommended for cases with vertical growth patterns.20,21
The complexity of a severe anterior open bite increases the difficulty of conventional orthodontic treatment, so that most of the time, its correction is through surgical-orthodontic treatment.21 One of the great advantages of this treatment is its long-term stability and its low relapse rate.18
ConclusionsDue to the clinical conditions of this case, we chose to follow a more conservative approach instead of using fixed appliances during the initial stage of the treatment. Based on this decision, we came up with the idea of using myofunctional therapy. Once the correction of the open bite was obtained we continued with the next stage of treatment, placing conventional fixed appliances. Orthodontic treatment in early stages of root development should be reconsidered in order to avoid root shortening specially when using heavy orthodontic forces. By guiding skeletal growth and modifying the patient’s muscle activity the possibility of relapse is reduced.