Case report of a 17-year-old male patient, skeletal class II, convex profile, not pleased with his facial appearance and without any intention to undergo surgical treatment. He presents severe protrusion and crowding, lip incompetence and protrusion, 7mm overjet and -3mm overbite. The treatment goals were to improve lip relation and esthetics, establish a functional occlusion, to improve the profile and muscular balance. Four first premolar extractions were performed and anchorage control was accomplished with a transpalatal and lingual arch. Treatment results were very successful achieving functional occlusion, lip competence, mandibular rotation and a decrease in profile convexity without surgical treatment. It is important to know the scopes and limits of orthodontic treatment regarding soft tissues, as well as maintaining anchorage to achieve profile changes with maxillary incisor retraction.
Paciente masculino de 17 años de edad, clase II esquelética, perfil convexo, no conforme con su aspecto facial y sin ninguna intención de someterse a un tratamiento quirúrgico. Presenta biprotrusión y apiñamiento dental severo, incompetencia y protrusión labial, sobremordida horizontal de 7mm y sobremordida vertical de -3mm. Los objetivos fueron mejorar la relación y estética labial, establecer una oclusión funcional, mejorar el perfil y equilibrar la musculatura. Se realizaron extracciones de cuatro primeros premolares y control de anclaje por medio de arco transpalatal y lingual. Los resultados del tratamiento fueron realmente satisfactorios logrando una oclusión funcional, compatibilidad labial, rotación mandibular y disminución de la convexidad del perfil sin la necesidad de un tratamiento quirúrgico. Es importante conocer los alcances y límites del tratamiento ortodóncico sobre los tejidos blandos, así como mantener un anclaje para lograr cambios en el perfil con la retracción del incisivo superior.
Class II malocclusion is one of the most common problems seen by orthodontists. In spite of the fact that successful treatment of this condition has been proved on many occasions, clinicians and patients continue to look for simpler and better methods for correcting the occlusion while maintaining or improving the facial appearance.1
The goal of modern orthodontic treatment consists not only in achieving dental and skeletal improvements, but also improvements in the soft tissues.2
The maxilla and mandible are the main osseous bases responsible for facial composition; the relationship between them, the occlusion and soft tissues define facial esthetics.The improvement of soft tissue profile depends on some variables related to the anatomy of the face, including lip thickness, facial muscle activity, ethnicity, gender, etc. The relationship between dentoalveolar movement and changes in the soft tissue can be observed in both the sagittal and the frontal plane.3
Dentoalveolar protrusion produces a convex facial profile, procheilia, and dental protrusion that result in lip incompetence and tension in the chin muscle. This condition is aesthetically unacceptable to some patients, who seek treatment for improving facial balance. Orthodontic treatment can correct the dentoalveolar protrusion by aligning and retracting the anterior teeth after the extraction of four premolars to reduce facial convexity and significantly improve lip posture.3
The assessment of facial balance and harmony includes studies on facial profile; the relationship between the nose, lips and chin can be altered by growth and orthodontic treatment and are important considerations for a balanced facial appearance.
Case report17-year-old male patient attends the orthodontics clinic with the following chief complaint: «I don’t like how my mouth and teeth look».
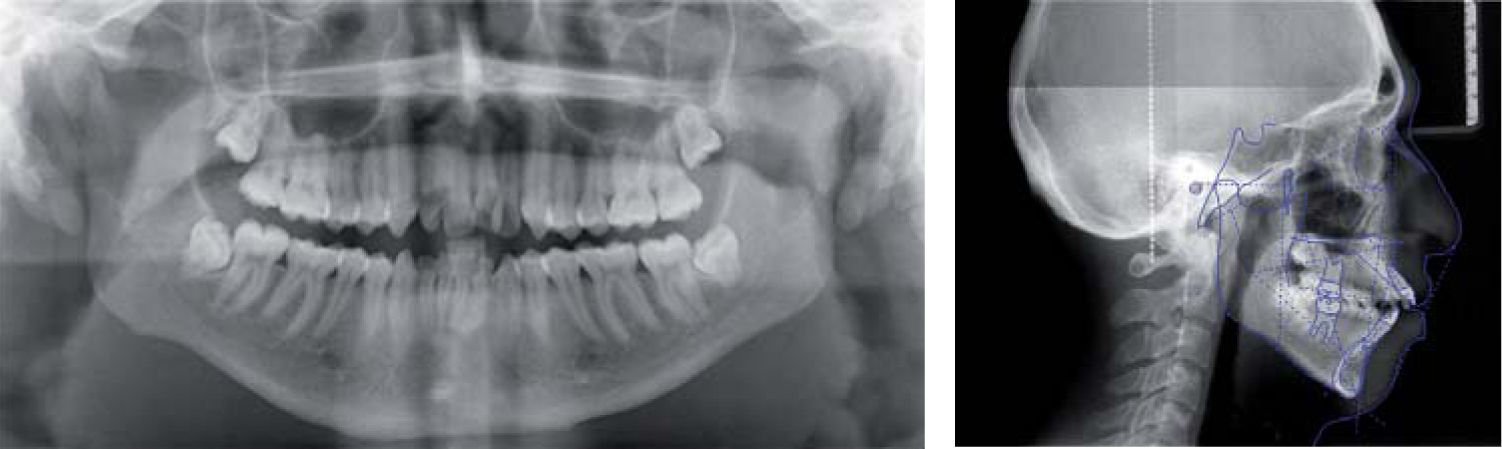
Cephalometrically, a dolichofacial, skeletal class II pattern with retrognathia, short anterior cranial base, increased vertical dimension, vertical growth, lower incisor protrusion, protrusion and proclination of the upper incisors is observed (Figure 1).
Upon facial examination, biprocheilia and lip incompetence at relaxed lip posture are observed. There is also chin muscle hypertonicity to achieve lip closure, a convex profile and a reduced cervico-mental distance (Figure 2).
Intraorally, the patient presents severe protrusion and dental crowding, 7mm overjet, -3mm overbite, bilateral canine class II, deviated dental midline, triangular and narrow upper arch shape (Figure 3).
Treatment goalsTo align and level the arches, position the incisor within their basal bone, increase vertical dimension, reduce overjet, achieve the six keys to occlusion,obtain occlusal stability, correct dental midlines, periodontal health, improve facial profile and muscular balance.
Treatment planWith the knowledge of the patient's dislike of his facial appearance and that he had no intention to undergo surgery the treatment plan should be designed to provide enough anchorage for upper incisor retraction and at the same time, space for molar mesialization to encourage mandibular rotation.
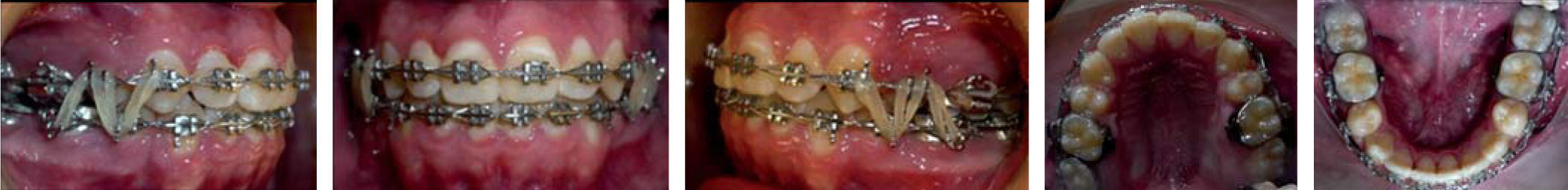
Treatment progress0.022 slot MBT brackets, a transpalatal and lingual arch were used; first upper and lower premolar extractions were performed and the alignment and leveling phase was begun with canine distalization (Figure 4).
Once the first treatment phase was finished, we continued with the space closure by means of active lacebacks (Figure 5).
Occlusion was detailed with the use of settling elastics and finally, circumferential retainers were placed (Figure 6).
ResultsExtra and intraoral photographs show satisfying results. The profile changed significantly due to the mandibular rotation and upper incisor retraction (Figure 7).
Occlusally, a bilateral class I molar and canine occlusion was achieved as well as a correct posterior intercuspation, an adequate overbite and overjet and anterior and canine guidance (Figure 8).
DiscussionClass II patients have a significant skeletal imbalance and orthodontic treatment is intended to correct or camouflage this discrepancy.1
Orthodontists have found that bicuspid extraction therapy causes changes in the profile and soft tissues. Many studies have focused their attention on the relationship between incisor retraction and changes in the upper and lower lip.4
Changes in the soft tissue profile are to some extent a matter of subjective opinion which varies from person to person according to fashion, race and social groups.4
Some studies have been based on lip changes in the sagittal plane, using superimpositions, lateral head films and facial photographs. However soft tissue changes in the frontal plane are more appreciated by patients because this is how they look at themselves in the mirror.5,6
We must study the proportions and adaptations of the normal soft tissue, its relation to tooth position and acknowledge that the stability of the results is influenced by soft tissue pressure and its balance effects.2
Beyond the obvious facial and dental changes, we observed positive changes in the patient's attitude and cooperation and improvement in his self-esteem.
ConclusionsFunctional occlusion, lip competence, mandibular anterior rotation, a decrease in profile convexity and a significant redistribution of the soft tissues around the chin was achieved without surgical treatment (Figure 9).
A correct diagnosis and case planning is essential for treatment success. It is important to understand the scope and limits of orthodontic treatment on soft tissues.
Regardless of the inherent characteristics of each facial type, beauty exists if there is symmetry, balance and proportion.