Case report of: a patient with severe inactive periodontitis, bone loss in the upper and lower anterior segments, supra-eruption of the upper and lower central incisors and spacing.
ObjectiveTo increase alveolar bone volume in the anterior segments, level and align the dental arches, upright incisors, close spaces and improve stability, function and esthetics.
MethodOrthodontic appliances were bonded, both dental arches were leveled and aligned; the incisors were intruded and their inclination corrected.
ResultsAlveolar bone volume was increased in the anterior segments thus reducing the bony defect between upper central incisors. Stability, function and aesthetics were improved.
ConclusionsThe orthoperio relationship has been well established, and the benefits of this relationship help the orthodontist to achieve contemporary treatment objectives.
Se presenta un caso clínico de paciente con periodontitis inactiva con severa pérdida de hueso en los segmentos anteriores superior e inferior, sobreerupción de incisivos centrales superiores e inferiores y múltiples diastemas.
ObjetivoAlinear y nivelar las arcadas dentales, eliminar la proinclinación de los incisivos, cerrar los diastemas, mejorar el balance de los tejidos blandos faciales e incrementar el volumen de hueso alveolar en los segmentos anteriores.
MétodosMediante la colocación de aparatología ortodóncica fija, se alinearon y nivelaron los arcos dentales, realizando intrusión y retroinclinación de los incisivos.
ResultadosSe obtuvo ganancia de hueso alveolar en los segmentos anteriores, disminuyendo considerablemente las bolsas periodontales y el defecto óseo entre incisivos centrales superiores, mejorando la estabilidad, función y estética.
ConclusionesLa relación orto-perio ha sido muy bien establecida, y los beneficios de esta relación ayudan al ortodoncista a obtener los objetivos contemporáneos de tratamiento.
According to the American Association of Orthodontics, 40 per cent of the patients who go to the dentist requesting to be treated orthodontically are adults. This situation compels the orthodontist to be faced with some previous diseases, the most common being periodontal disease.1
Despite the fact that these conditions are frequently found in adult patients, it is important to bear in mind that it is possible to perform orthodontic movements without increasing damage to the support tissues. In order to perform these movements in a harmless way, it is essential that there exists an adequate periodontal control that guarantees the absence of bacterial plaque; otherwise, bone loss will increase considerably.2
Patients with a history of periodontal disease may obtain benefits through the teamwork between the periodontist and orthodontist. The conditions of the injured periodontal tissue may be improved by means of orthodontic tooth movements.
It is important to consider that under these periodontal conditions, the therapeutic goals of treatment are limited. Therefore each case must be examined carefully and thoroughly, with the purpose of establishing interdisciplinary treatments where priorities and therapeutic possibilities are identified.3
CASE REPORTA male patient of 38 years of age attended the Orthodontics Clinic at the Division of Post- Graduate Studies and Research of the Faculty of Odontology of the National Autonomous University of Mexico referred by the Padierna Peripheral Clinic of the Faculty of Odontology of the UNAM with the suggestion of performing orthodontic treatment for improving his occlusal condition. The patient had a history of aggressive periodontitis which was treated through plaque control, scaling and root planing (the patient underwent previously root canals in the upper and lower central incisors), occlusal adjustment and splinting of the anterior segments. A flap debridement in these segments was performed using enamel matrix-derived proteins (Emdogain®, Straumann. Basel, Switzerland), plasma rich in growth factors and collagen membrane; all to improve the level of insertion.
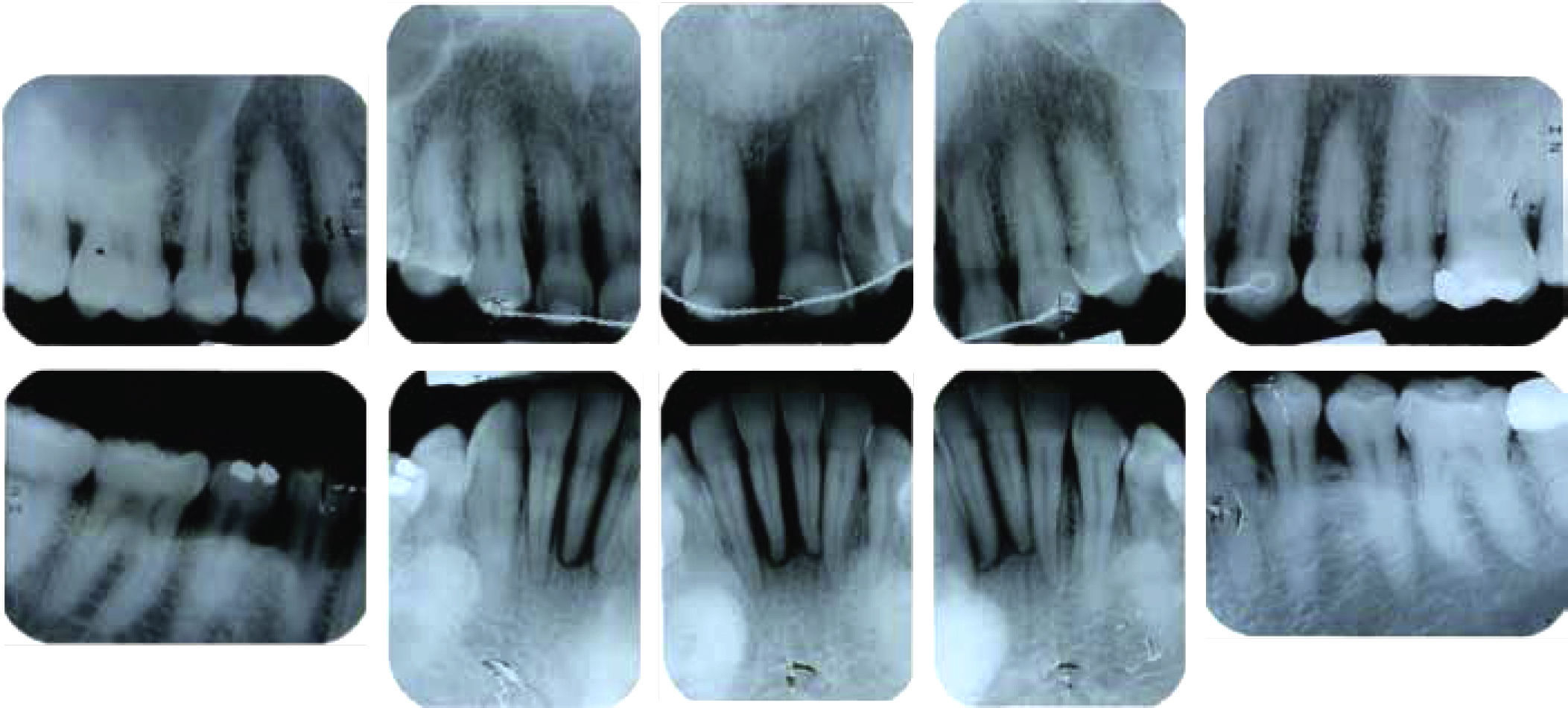
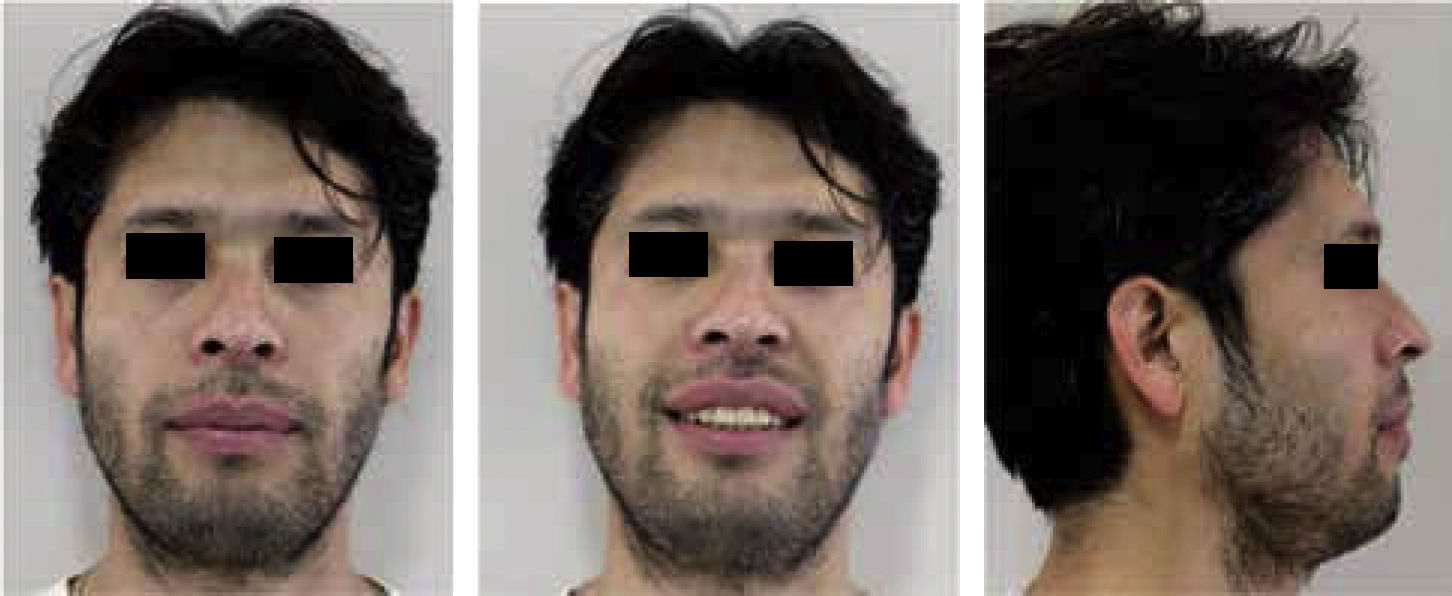
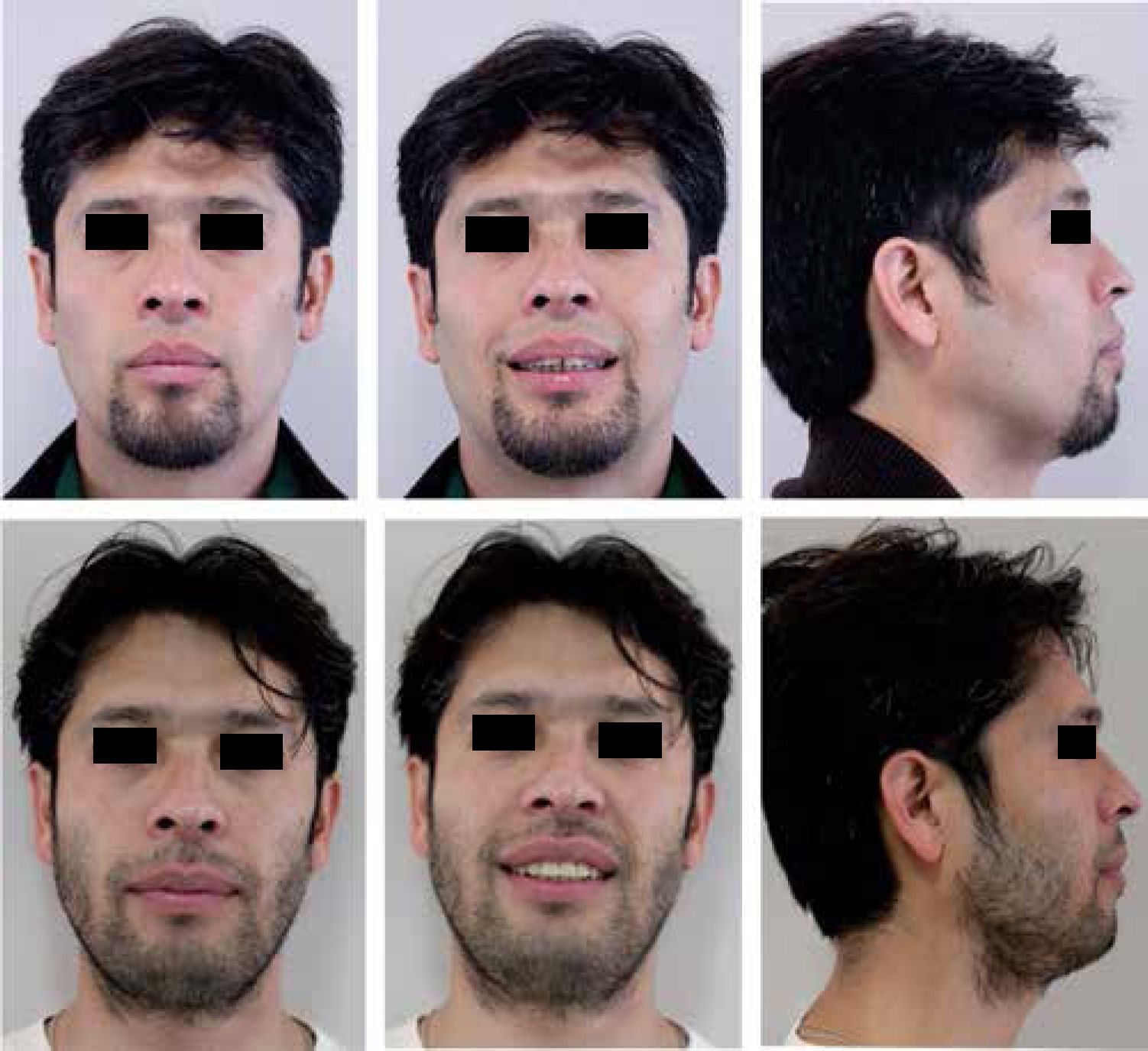
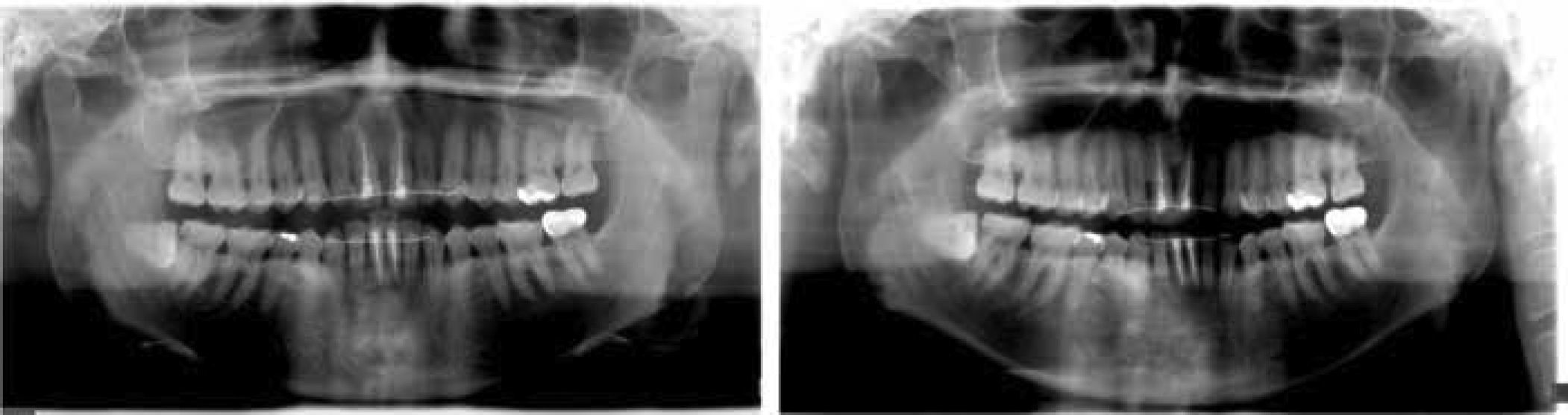
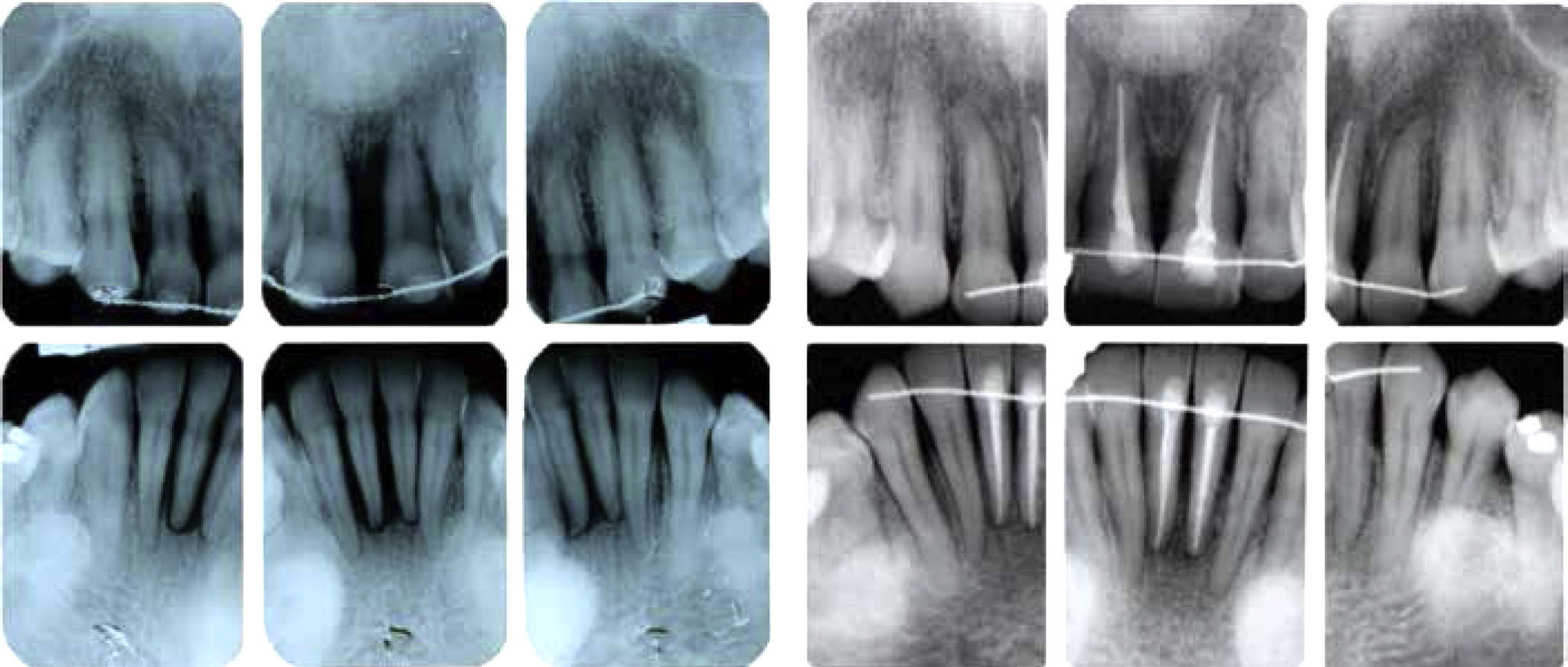
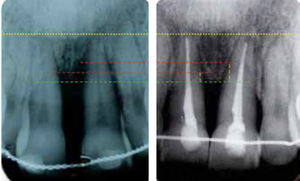
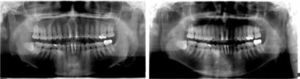
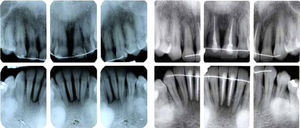
DIAGNOSISMesofacial patient, with convex profile (Figure 1), skeletal class II due to retrognathism (Table I), molar and canine class II, over-erupted incisors with severe upper and lower dental proclination, increased overjet, diastema, triangular arches (Figures 2 and 3) and widespread loss of alveolar ridges, mainly in the upper central incisors (Figure 4).
- •
Optimization of periodontal tissue.
- •
Intrusion of anterior segments.
- •
Space closure.
- •
Overjet reduction.
- •
Arch consolidation.
0.022” x 0.028” MBT fixed appliances (3M UNITEK, Monrovia, CA) were placed. Through height control during placement of the upper and lower anterior brackets, incisor over-eruption was corrected. Aligning and leveling of the arches was performed using 0.014” and 0.016” Nickel Titanium round arches. Subsequently, 0.016” x 0.022” rectangular arches of the same alloy and 0.016” x 0.022” stainless steel were used. Due to the existence of black triangles, it was decided to remodel the triangular anatomy of the upper and lower front teeth by performing interproximal reduction. Posterior anchorage segments were formed (linked in block from canine to molar) and subsequently proceeded to close the created spaces with elastic string from canine to canine. Incisal ameloplasty of the edges of the upper incisors was also conducted in order to improve aesthetics (Figure 5).
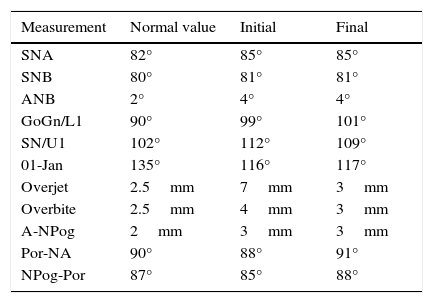
The patient was under continuous monitoring by the Department of Periodontics and periapical radiographic series for control and an orthopantomography for root parallelism were requested. Bracket repositioning was performed as necessary and a 0.016” Nickel-Titanium archwire was placed. Afterwards, a 0.016” x 0.016” stainless steel archwire was used to improve the anteroposterior relationship along with class II vector intermaxillary elastics 24hours a day.
Fixed appliances were removed and fixed retainers were bonded from canine to canine in both arches (Figure 6). Use of circumferential removable retainers (upper and lower) was indicated 24hours a day.
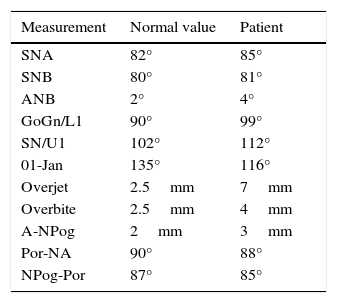
TREATMENT RESULTSThe existent defect between the upper central incisors was significantly reduced; however, due to its severity and extension, it could not be corrected entirely (Figures 7 to 10). The rest of the treatment goals were achieved in a satisfactory manner; however, the class II molar and canine relationship was not resolved in its entirety due to the fragility of the periodontal tissues (Table II).
Initial and final cephalometric values.
| Measurement | Normal value | Initial | Final |
|---|---|---|---|
| SNA | 82° | 85° | 85° |
| SNB | 80° | 81° | 81° |
| ANB | 2° | 4° | 4° |
| GoGn/L1 | 90° | 99° | 101° |
| SN/U1 | 102° | 112° | 109° |
| 01-Jan | 135° | 116° | 117° |
| Overjet | 2.5mm | 7mm | 3mm |
| Overbite | 2.5mm | 4mm | 3mm |
| A-NPog | 2mm | 3mm | 3mm |
| Por-NA | 90° | 88° | 91° |
| NPog-Por | 87° | 85° | 88° |
The patient was very satisfied with the obtained aesthetics; masticatory function was improved as well as the teeth stability. The integrity of the periodontal tissues was optimized (Figures 11 to 15).
DISCUSSIONThere is clinical evidence that demonstrates that the correct interdisciplinary management of patients with sequelae of periodontal disease provides beneficial effects to the support tissues.4-7 The management of these patients must be done carefully, maintaining an adequate monitoring by the periodontist, who must perform a correct control of the periodontal status before, during and after orthodontic treatment.3,6,8 Cirelli (2006) demonstrated good results in interdisciplinary treatment between Orthodontics and Periodontics where periodontal monitoring was carried out at intervals of 3 months during active orthodontic treatment. Levelin (2012) and Tortolini (2011) mention this as well.6
On the contrary, to perform orthodontic treatments in patients with active periodontal disease, without having been previously treated, contributes to the progression of tissue decay due to the forces generated by the appliances and the plaque retention they produce thus resulting in greater destruction of periodontal tissue.9
Different authors such as Corrente (2002), Cirelli (2006) and Scaf (2014) show that it is possible to reduce bony defects generated as a result of periodontal disease through orthodontic treatment and that there is also an increase in gingival insertion and a decrease of the probing depth in the area of the lesion at the end of the orthodontic treatment.5–7 By maintaining good periodontal control, providing light orthodontic forces and performing dental movements in the right direction, the correction of these kinds of defects is favored, as affirmed by Tortolini (2011), Boyer (2011), Scaf (2014) and Melsen (1988).3,4,7,10,11
CONCLUSIONSThe ortho-perio relationship has been well established, as well as its benefits: it helps the orthodontist to achieve contemporary goals of treatment.
Among the goals of contemporary Orthodontics is the stability and integrity of the periodontal tissues in addition to function and aesthetics. Good communication between the orthodontist and the periodontist permits reaching these goals in patients with prior tissue damage and periodontal defects.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia