Male patient of 13 years of age, skeletal class II with horizontal growth and prominent chin, whose main reason for consultation was his prominent chin who presented a concave profile, brachifacial biotype, lower retrocheilia, prominent chin, horizontal growth, deep mentolabial fold. He had a class II division 2 malocclusion, a 4mm overjet and a 6mm overbite. The treatment objectives were to improve the facial and dental aesthetics, coordinate dental arches and establish a functional occlusion. Interdisciplinary treatment was performed (orthodontic-orthognathic surgery), beginning with a pre-surgical phase by placing .022 slot MBT fixed appliances. In the surgical phase, a triple surgery was performed and subsequently, a postsurgical stage. Treatment results were satisfactory since the set out objectives were achieved thus improving the patient's facial aesthetics. Interdisciplinary communication is important as well as to recognize the patient's expectations in order to perform a good diagnosis and select the treatment alternative that best favors function, aesthetics and improves the patient's self-confidence.
Paciente masculino de 13 años de edad, clase II esquelética, con crecimiento horizontal y mentón prominente, cuyo principal motivo de consulta era el mentón prominente existente. Presenta perfil cóncavo, braquifacial, retroquelia inferior, mentón prominente, crecimiento horizontal, surco mentolabial muy marcado, dentalmente es clase II división 2, sobremordida horizontal 4mm y sobremordida vertical 6mm, mordida profunda. Los objetivos fueron mejorar la estética facial y dental, relacionar arcadas, establecer una oclusión funcional. El tratamiento realizado fue interdisciplinario (ortodóncico-quirúrgico), se inició con la fase prequirúrgica colocando aparatología fija MBT slot .022. En el tiempo quirúrgico se realizó una cirugía triple y posteriormente la fase postquirúrgica. Los resultados del tratamiento fueron satisfactorios, debido a que se consiguieron los objetivos planteados, mejorando estética y facialmente al paciente. Es importante la comunicación interdisciplinaria y las expectativas del paciente para llevar a cabo un buen diagnóstico y tomar la mejor alternativa de tratamiento; favoreciendo la función, estética y proporcionando seguridad personal al paciente.
Aesthetics is the main motivational reason for patients seeking orthodontic treatment due to the fact that perception of the facial profile and dental aesthetics are essentially based on how people perceive themselves, however, people's emotions, thoughts and behavior may vary and these differences create individuality.1 Some studies have argued that psychological factors may have certain effects on facial perception and dental aesthetics among young adults.1,2
Class II malocclusions can pose a challenge for the diagnosis and treatment plan due to the fact that clinical features may hinder the cause of the malocclusion, and this may be because the maxilla is narrower than in adults with normal occlusion.3,4 The literature has mentioned that in patients with dentoskeletal disharmonies (class II), growth is different compared to patients with a normal dentoskeletal relationship, both in quantity as well as in direction of the craneofacial structures.5
In 1899, class II division 2 malocclusion was defined by Angle. It has a relatively low prevalence in comparison with other malocclusions. This malocclusion is generally characterized by retroclined upper central incisors, deep bite and molars and canines in distocclusion.6–10
Etiology is multifactorial as there may be genetic or environmental factors involved or it may be due to a high lip line, lip hyperactivity or increased masticatory forces.10–13
Usually, patient's with this malocclusion have a mesofacial or braquifacial biotype, many show a normal facial convexity and a straight or convex profile. Although they may have anti-aesthetic facial proportions and occlusal disharmonies, their mandibular ramus is normal or long and they have good growth potential of the mandible, sometimes even similar to patients with class I malocclusions.9,11–13
However, the maxilla and mandible are the main bony bases of facial composition, therefore, the relationship between them, their occlusion and soft tissues define facial esthetics.14
Likewise, assessment of facial balance and harmony includes an analysis of the facial profile, therefore, the relationship between nose, lips and chin may be altered by growth and is important for a proportionate facial appearance.14,15
This article describes the clinical case of a male patient of 13 years of age, who presented a class II division 2 malocclusion and a very prominent chin being the latter the main reason for consultation.
CLINICAL CASEMale patient, 13 years of age who attended the Orthodontics Department at the Division of Postgraduate Studies and Research (DEPeI) of the National Autonomous University of Mexico (UNAM) and whose main reason for consultation was «I have a very large chin».
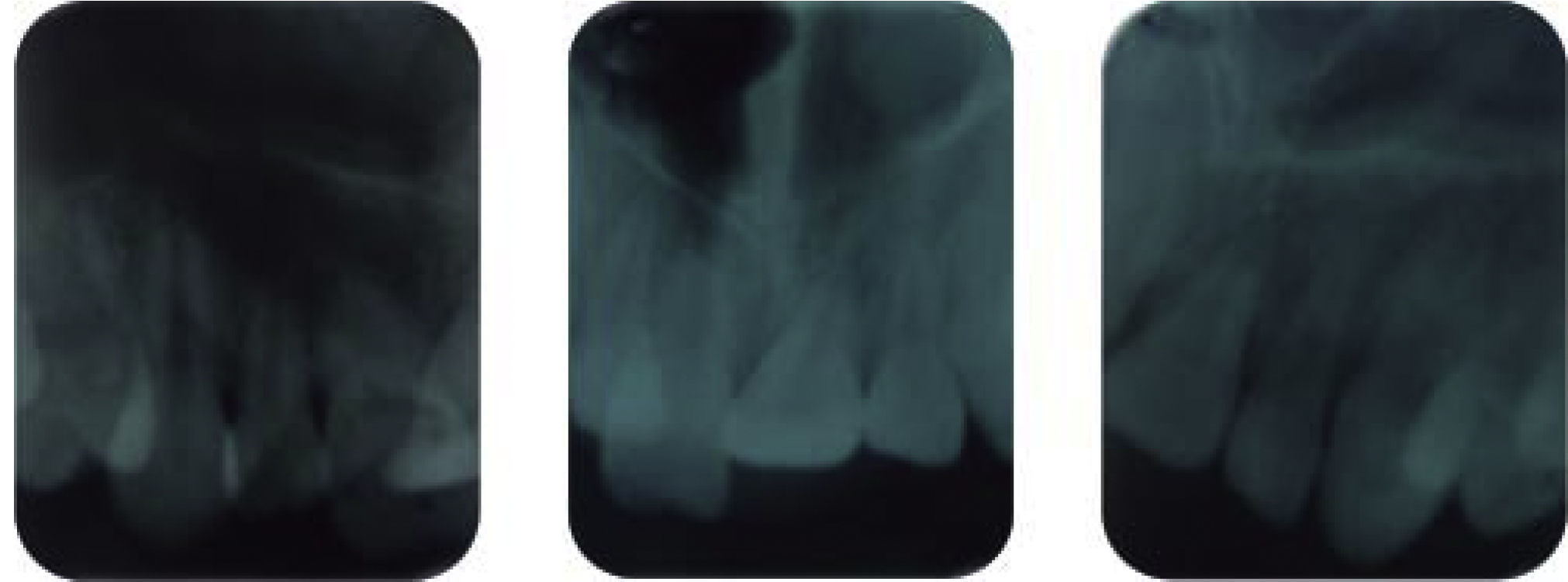
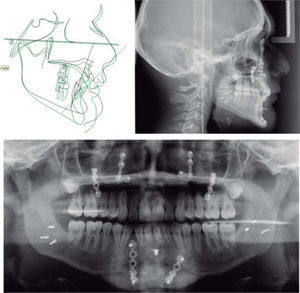
Cephalometrically, he was a brachycephalic skeletal class II and presented a retrusive lower lip, concave profile, prominent chin, short anterior cranial base, horizontal growth, upper incisor proclination and protrusion and lower incisor retroclination and retrusion (Figure 1). The panoramic radiograph (Figure 2) reveals a 2:1 crown-root ratio, adequate alveolar ridge height, presence of four third molars and short roots in the upper anterior teeth which was confirmed with periapical radiographs (Figure 3).
Facially, the patient had a concave profile, prominent chin, straight nose, deep mentolabial fold, protrusive upper lip, wide buccal corridors, upper incisor display when smiling (Figure 4).
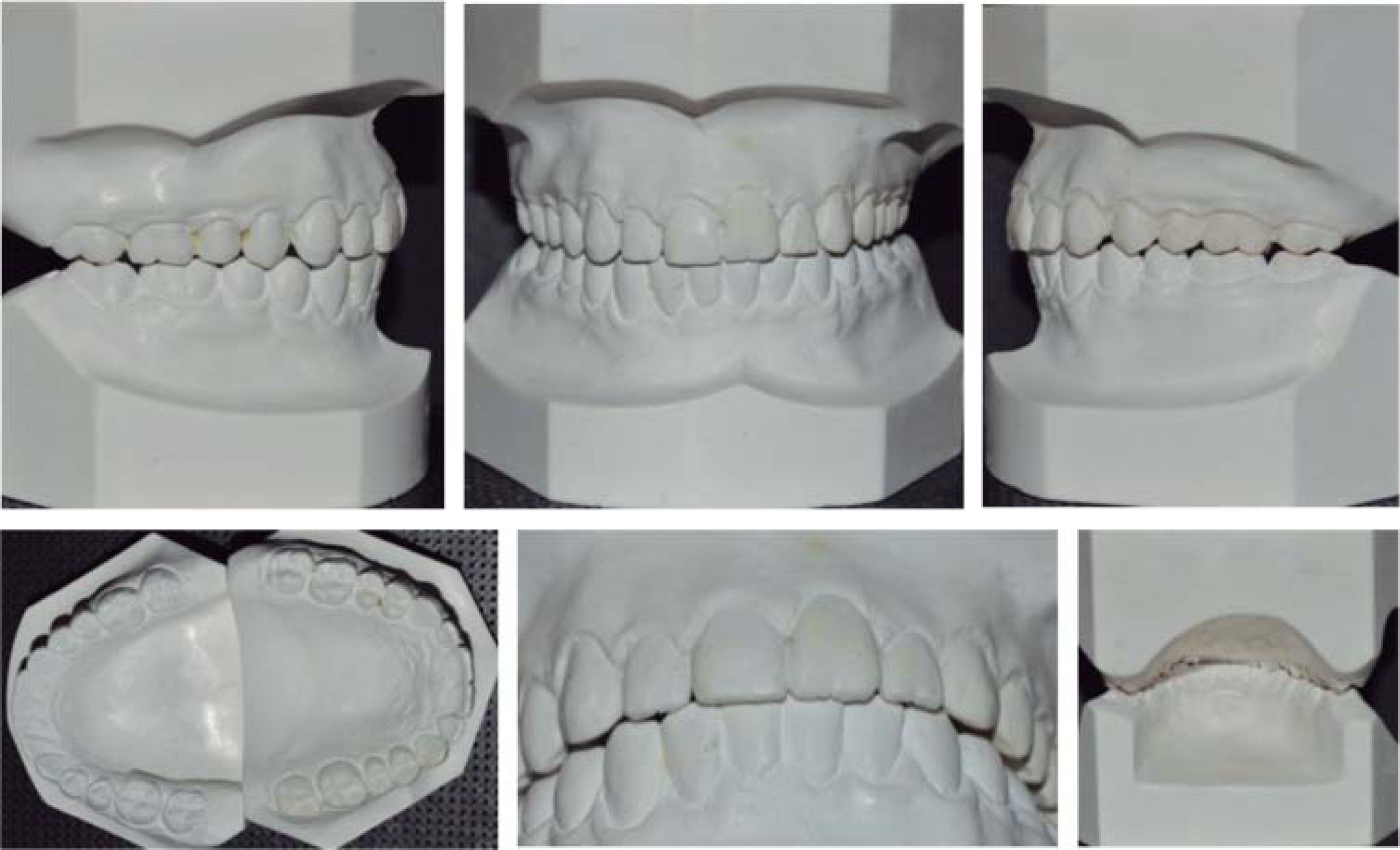
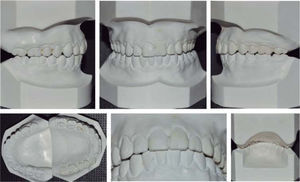
At the intraoral clinical examination and orthodontic analysis, the patient presented a class II division 2 malocclusion, upper incisor proclination and protrusion, lower incisor retroclination and retrusion, bilateral molar class II and canine class I, increased overbite and overjet, squared dental arches, molar rotation, excessive curve of Spee, severe upper and mild lower crowding, negative discrepancies between basal bone length and tooth material, bilateral molar and canine class II, increased overbite and overjet (Figure 5).
Treatment objectivesSkeletal class I with as much improvement of the profile as possible, eliminate dental crowding, coordinate arches, achieve molar and canine class I as well as establish an adequate overbite and overjet and correct the dental midline.
Treatment planOrthodontic-surgical treatment, 0.022 slot MBT fixed appliances with bands in first and second upper and lower molars were placed.
Presurgical phase: initial leveling and alignment, coordination of dental arches, root correction and parallelization, closure of spaces.
Surgical phase: surgical prediction in conjunction with the department of surgery.
Postsurgical stage: re-leveling, bracket re-position, consolidation, stabilization, smile detailing and retention.
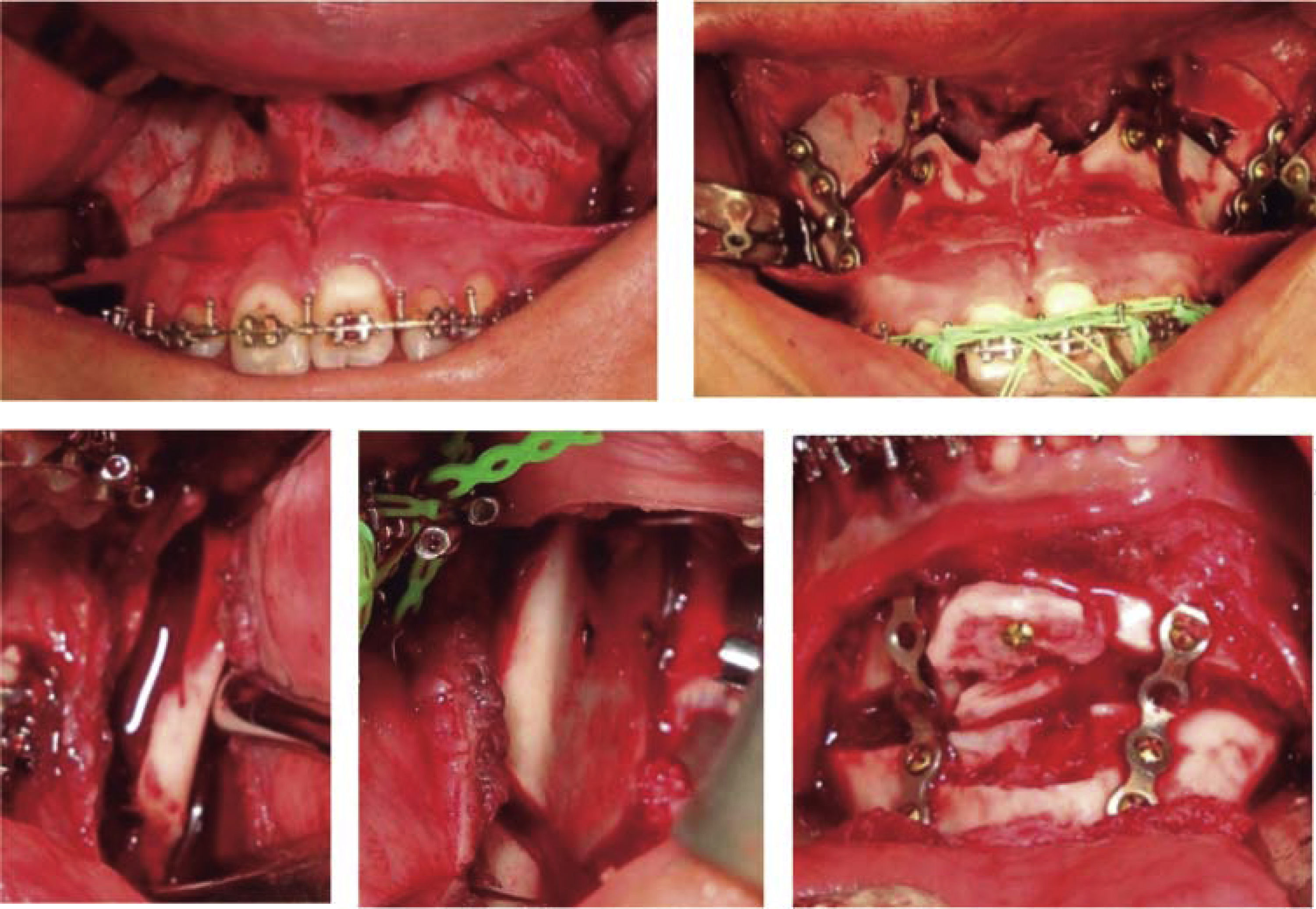
Course of treatmentTreatment was begun with the placement of 0.022 slot MBT fixed appliances, starting with the leveling and alignment (Figure 6A), the dental organ #22 was gradually incorporated, conforming the dental arches.
Upper expansion was performed with a 0.032 wire in the accessory molar tubes (Figure 6B). The patient was referred to the Department of Surgery, where the case was assessed and the surgical prediction and model surgery were performed in an interdisciplinary way (Figure 6c).
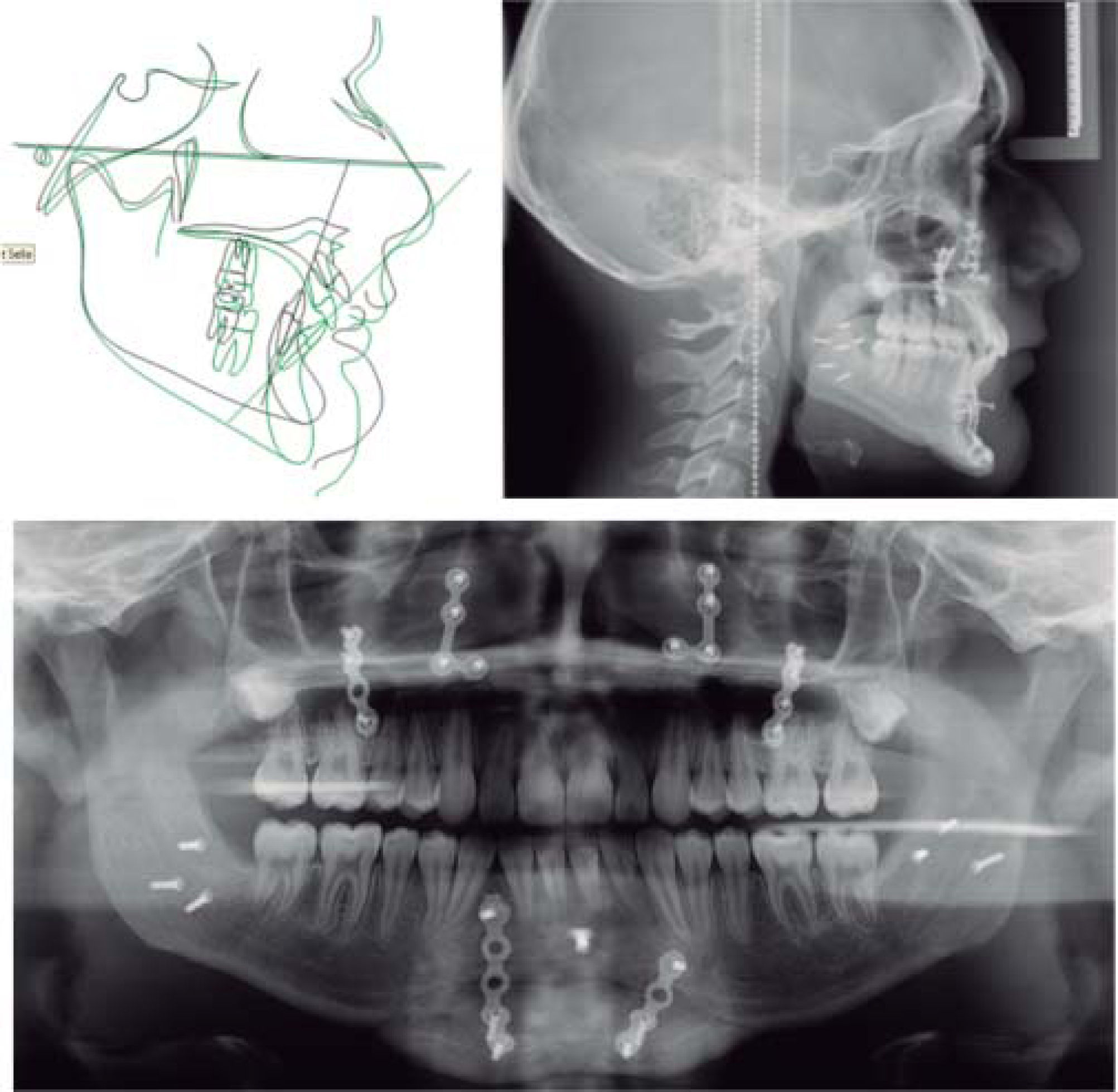
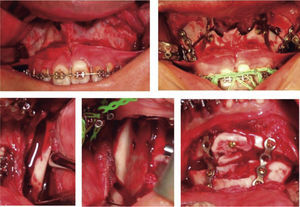
In the maxilla, a Le Fort I osteotomy with a downward reposition was performed. The maxilla was segmented into three parts (3mm); in the mandible, a 3mm advancement was made and the chin was repositioned downwards 6mm (Figure 7).
Follow-up appoinments were scheduled at day 7, 15 and a month after the surgical procedure (Figure 8). 3.5 ounces, 5/16” intermaxillary elastics were used for 3 months for fixation, and afterwards, class II ¼” 3.5 ounces elastic were used. Subsequently, brackets of the dental organs #11, 22 and 12 were repositioned. Three months after the reposition appointment, fixed appliances were removed (Figure 9).
Retention: upper and lower circumferential retainers were placed.
RESULTSTreatment objectives were accomplished: cephalometrically, skeletal class I was achieved; facially, the profile improved. Occlusally dental crowding was eliminated; molar and canine class I was achieved; an adequate overbite and overjet, maximal intercuspation and canine guidance were obtained (Figures 10 to 12andTable I).
UNAM analysis.
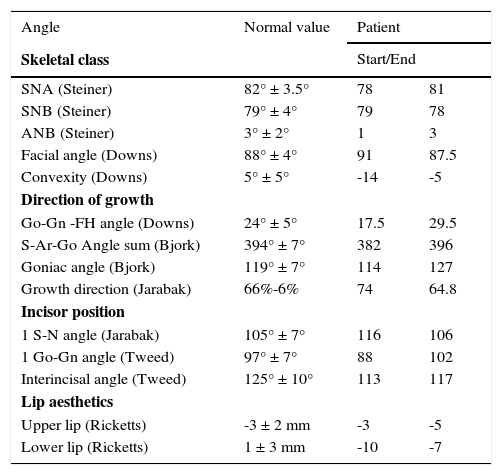
| Angle | Normal value | Patient | |
|---|---|---|---|
| Skeletal class | Start/End | ||
| SNA (Steiner) | 82° ± 3.5° | 78 | 81 |
| SNB (Steiner) | 79° ± 4° | 79 | 78 |
| ANB (Steiner) | 3° ± 2° | 1 | 3 |
| Facial angle (Downs) | 88° ± 4° | 91 | 87.5 |
| Convexity (Downs) | 5° ± 5° | -14 | -5 |
| Direction of growth | |||
| Go-Gn -FH angle (Downs) | 24° ± 5° | 17.5 | 29.5 |
| S-Ar-Go Angle sum (Bjork) | 394° ± 7° | 382 | 396 |
| Goniac angle (Bjork) | 119° ± 7° | 114 | 127 |
| Growth direction (Jarabak) | 66%-6% | 74 | 64.8 |
| Incisor position | |||
| 1 S-N angle (Jarabak) | 105° ± 7° | 116 | 106 |
| 1 Go-Gn angle (Tweed) | 97° ± 7° | 88 | 102 |
| Interincisal angle (Tweed) | 125° ± 10° | 113 | 117 |
| Lip aesthetics | |||
| Upper lip (Ricketts) | -3 ± 2 mm | -3 | -5 |
| Lower lip (Ricketts) | 1 ± 3 mm | -10 | -7 |
It is important to take into consideration aesthetics and facial and dental harmony since currently, facial esthetics is highly valued by society in general and we must consider the therapeutic options for treating class II malocclusions as well as their effect on the patient's profile.1,2
Profile changes are subjective, because the point of view varies from person to person, depending on the sociocultural environment. Therefore, it is recommended to study facial and dental proportions to balance such aesthetics.14
To perform a proper interdisciplinary diagnosis, taking into consideration the patient's expectations and carefully assessing the treatment plan is important for achieving the set objectives and for being able to improve the patient's social setting.1,2,14
CONCLUSIONInterdisciplinary communication and the patient's perception are important to perform a good diagnosis and select the best treatment alternative for the patient's benefit, favoring function, aesthetics and providing greater self-confidence for the patient to interact in their social environment.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia