The objective of this case report was to show the correction of a class II division 1 malocclusion in an adult patient. A female patient of 20 years of age attended the Orthodontics Clinic of the Division of Postgraduate Studies and Research of the Odontology Faculty at the National Autonomous University of Mexico. Her main reason for consultation was: «When I removed the wisdom teeth I was told that I could have orthognathic surgery but first I needed braces»; this in order to correct the dentofacial disharmony. Upon facial clinical examination, the patient presented a mesofacial biotype with competent lips; vertically she presented an increased lower third. Her profile was convex with deficient chin projection. Intraorally, the patient exhibited upper and lower crowding, molar and canine class II, considerably increased overbite and overjet as well as noncoincident dental midlines. The cephalometric diagnosis showed a skeletal class II due to maxillary protrusion. It was suggested an orthodontic-surgical treatment in three phases: presurgical, surgical and postsurgical. In the presurgical phase the patient was decompensated in order to prepare her for surgery. During the surgical phase, mandibular sagittal osteotomies were performed to advance the mandible in combination with an advancement genioplasty. During the post-surgical phase, ideal occlusal relationships were achieved in terms of canine classes, overbite, overjet, dental midlines and final detailing of the case. Through the treatment, the occlusion and facial harmony of the patient were improved.
El objetivo de este caso clínico es demostrar la corrección de una clase II división 1 en un paciente adulto. Paciente femenino de 20 años de edad que acude a la Clínica de Ortodoncia de la División de Estudios de Posgrado e Investigación de la Universidad Nacional Autónoma de México. Su motivo principal de consulta es: «Cuando me quitaron las muelas del juicio me dijeron que me podían operar pero primero tenían que ponerme brackets»; esto para poder corregir la disarmonía dentofacial que presentaba. A la exploración clínica extraoral, se observa una cara mesoprosopa con labios competentes; verticalmente presenta el tercio inferior aumentado. Su perfil es convexo con una proyección deficiente del mentón. Intraoralmente, presenta apiñamiento dental superior e inferior, relación clase II molar y canina, la sobremordida vertical y horizontal considerablemente aumentadas y líneas medias no coincidentes. Su diagnóstico cefalométrico mostró clase II esquelética por protusión maxilar. El tratamiento propuesto ortodóncico-quirúrgico, en tres fases: ortodóncica prequirúrgica, quirúrgica y ortodóncica posquirúrgica. En la fase prequirúrgica se descompensó a la paciente para prepararla para la cirugía. En la fase quirúrgica se realizó una osteotomía sagital mandibular para realizar un movimiento de avance en combinación con una mentoplastia de avance. Durante la fase posquirúrgica se lograron relaciones oclusales ideales en cuanto a las clases caninas, sobremordida, resalte, coincidencia de líneas medias y el detallado final del caso. Con el tratamiento mejoró la oclusión y la armonía facial de la paciente.
Class II division 1 is one of the most difficult to correct malocclusions. It causes an important facial disharmony characterized by a deficient projection of the mandible, which leads to a convex profile, nonaesthetic facial proportions and occlusal disharmonies creating in the patient a negative psychological impact and a functional problem.1,2
The pathogenesis is of multifactorial origin but there are two fundamental components: genetics and extrinsic factors such as habits: digital suction, lip suction, abnormal deglutition, among others. 1,3 Treatment alternatives are different depending on the age of the patient and the severity of the case.
Orthognathic surgery is a good treatment approach for patients with severe skeletal discrepancies beyond the reach of conventional orthodontic treatment. Combined surgical-orthodontic treatment aims to obtain a more harmonious facial, skeletal and soft tissue relationship as well as to improve occlusal function. It has been demonstrated that facial and dental abnormalities that affect facial appearance may result in social disadvantage. Hence patients undergoing orthognathic surgery may experience psychosocial benefits and improve their selfconfidence, facial image and social adaptation.4
A very important factor to be considered for surgical-orthodontic treatment is the paradigm of the soft tissues. It establishes that both the objectives and limitations of modern orthodontic and orthognathic treatment and are determined by the facial soft tissues, not by teeth or bones.5
As a result, the main objective of treatment happens to be the relationship and adaptations of the soft tissues, and not the ideal occlusion. It is admitted that for the patient to be able to benefit fully from treatment, ideal occlusion not always represents the fundamental aspect of a treatment plan. Functional occlusion, becomes the secondary objective of the treatment.5
CASE REPORTA female patient, 20 years of age, attended the Orthodontics Clinic of the Division of Postgraduate Studies and Research of the Odontology Faculty of the National Autonomous University of Mexico. The main reason for consultation is «When I had my wisdom teeth removed, I was told that they could perform orthognathic surgery on me but first I had to have orthodontic treatment». This, in order to correct the facial anomaly that may be observed in the profile.
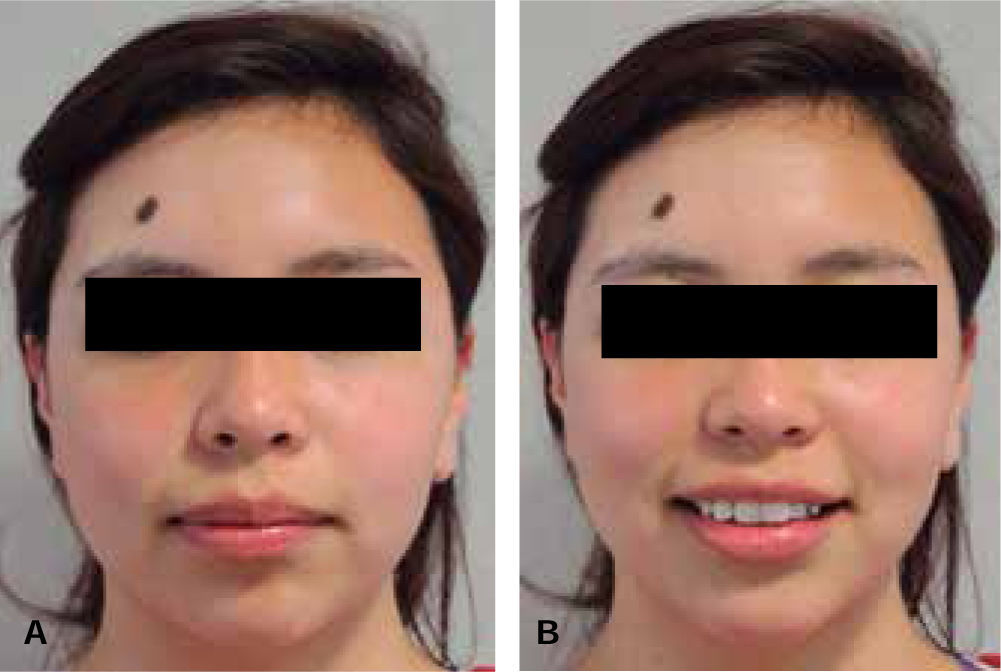
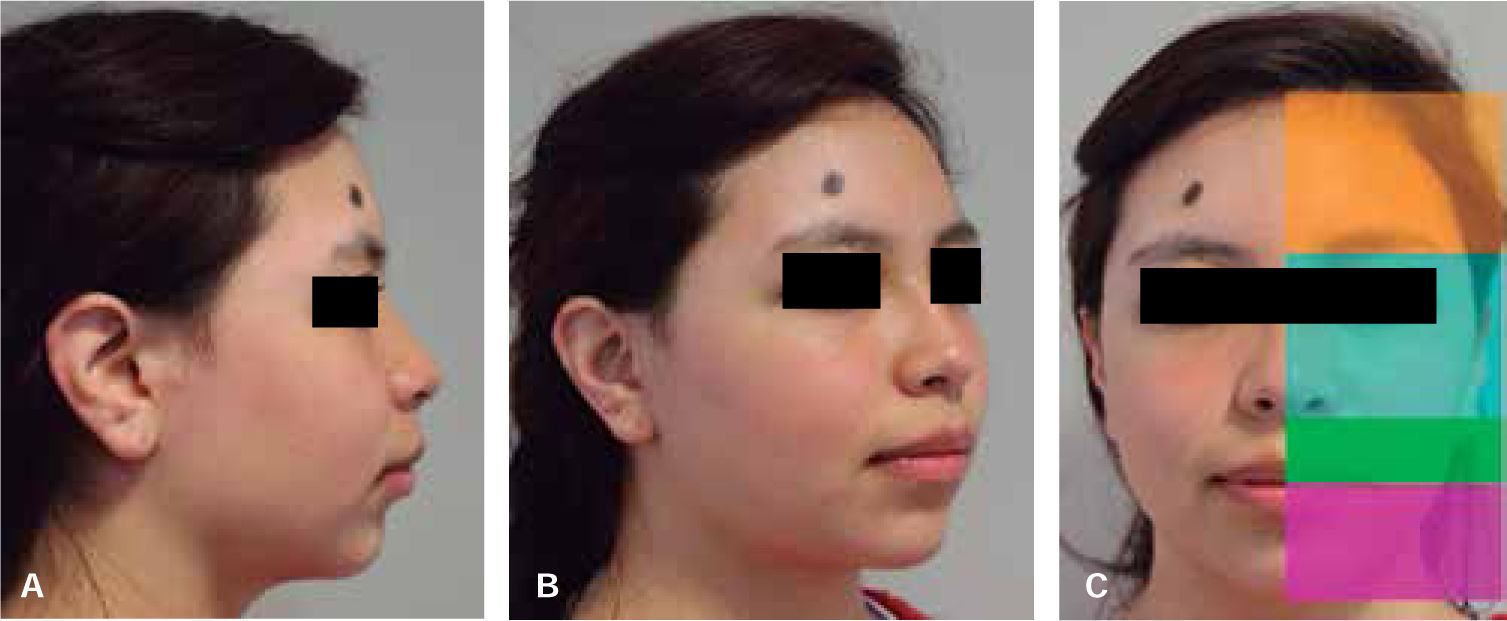
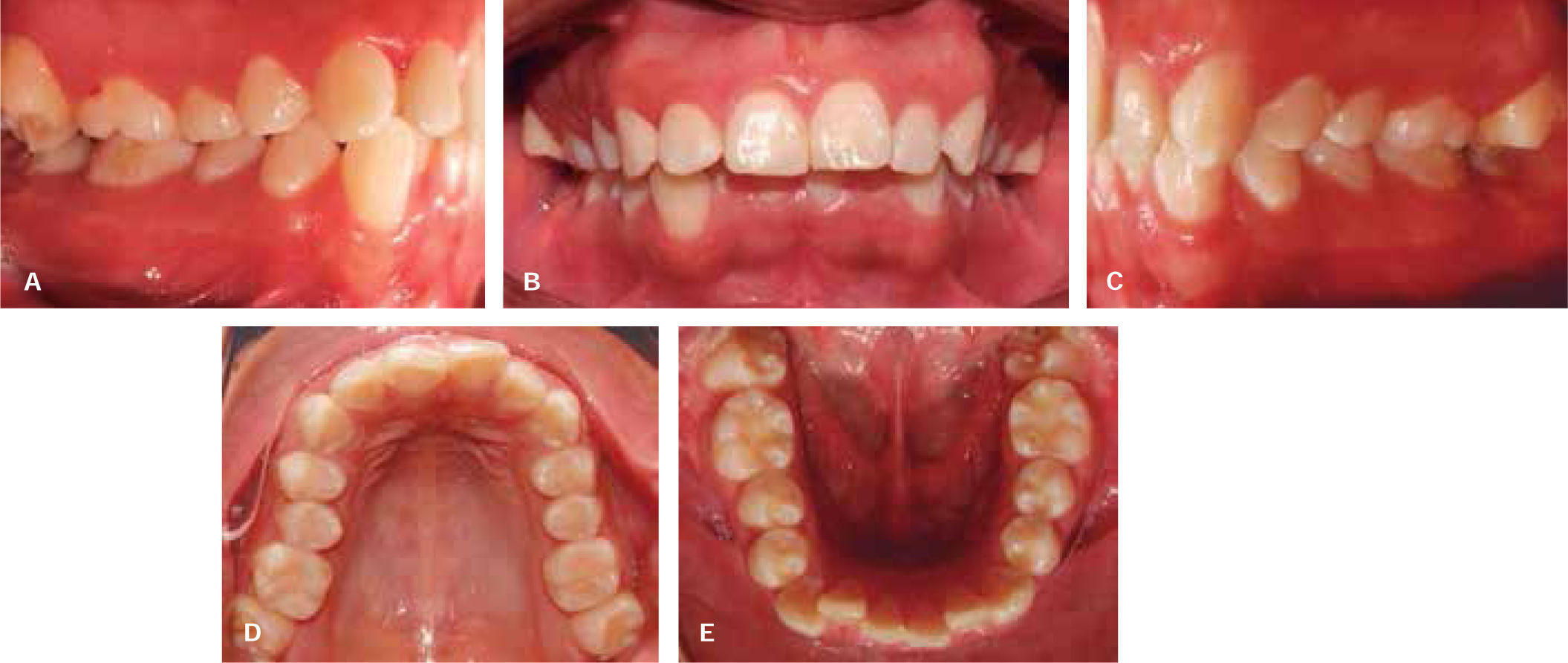
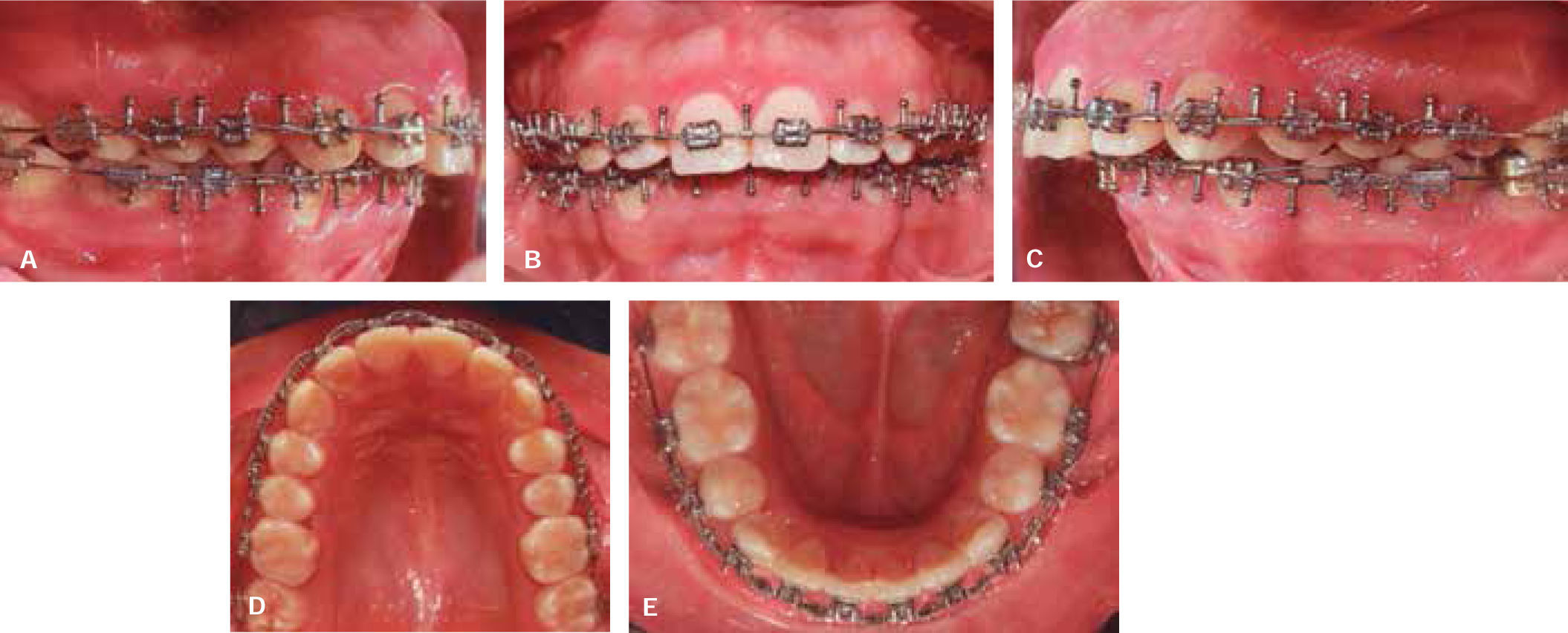
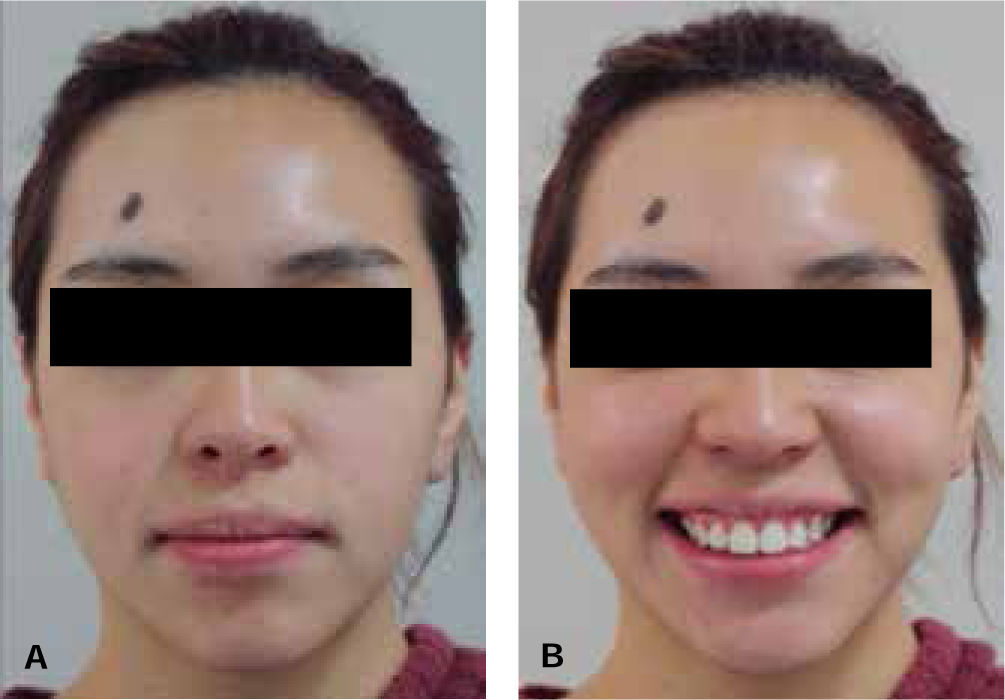
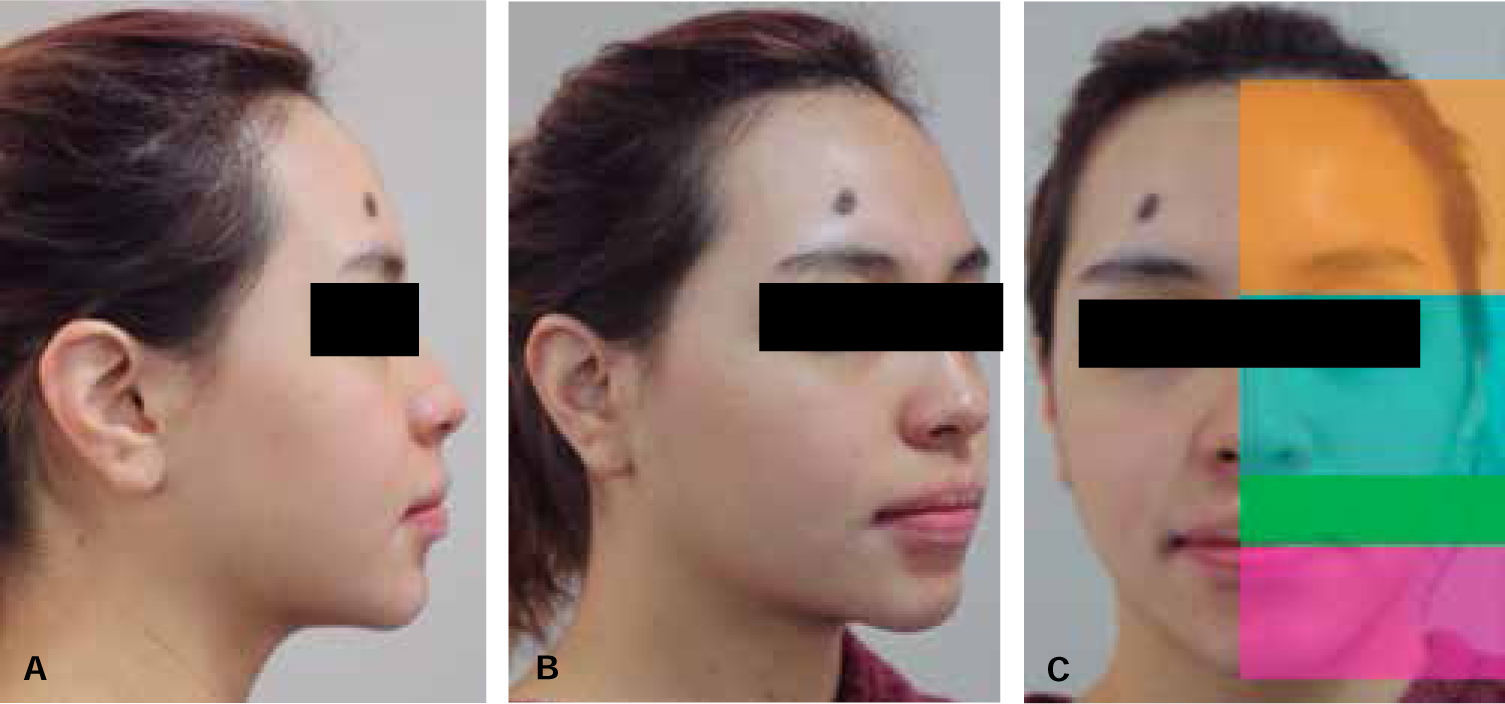
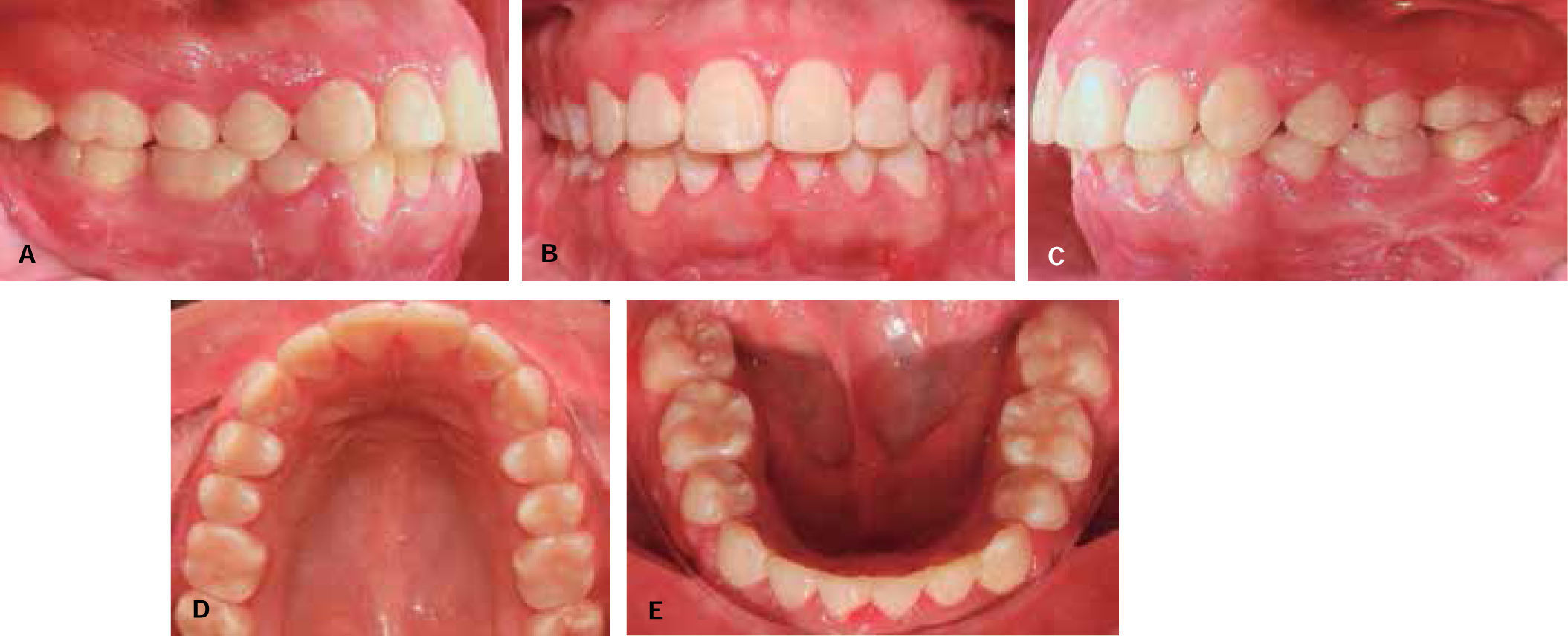
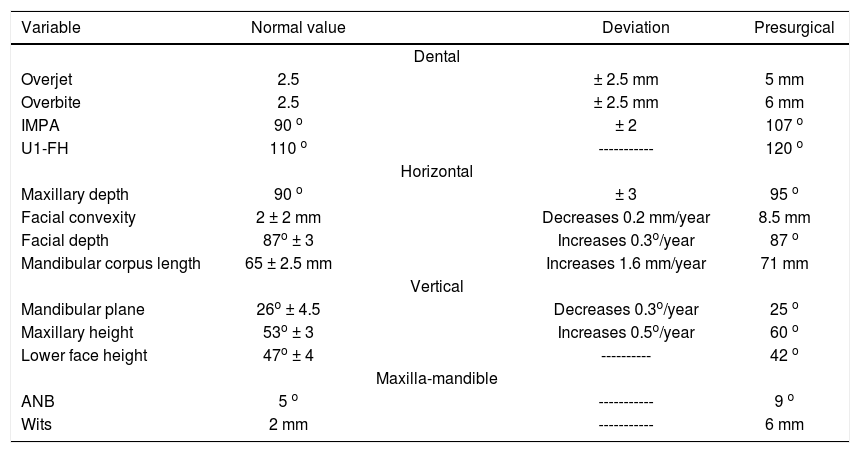
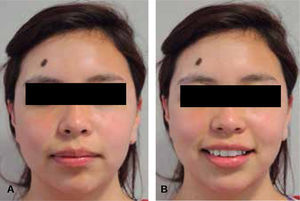
Clinical characteristics: at the facial clinical examination, in the front view the following characteristics were observed: a mesoprosope, round face, competent and thick lips and the facial midline coincides with the upper dental midline. The smile is neutral and shows nearly 100% of the clinical crowns of the upper teeth (Figure 1). The vertical analysis shows the lower third increased in relation to the middle third. The lateral view of the patient shows a convex profile, with an obtuse (open) nasolabial angle and a decreased occipital-cervical distance (Figure 2). Intraorally, the patient presented dental crowding, mismatched midlines, canine and molar relationship class II, an overjet of 6 and a 5 mm overbite (Figure 3).
Radiographic records were taken prior to treatment, including panoramic and lateral headfilm radiographs and a CBCT (Figures 4and5). In them, it was observed: 28 permanent teeth, good crownroot ratio (2:1), appropriate level of bony ridges, slight asymmetry of the mandibular ramus and no signs of TMJ disease.
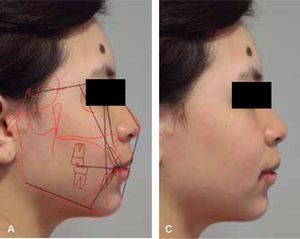
The cephalometric analysis revealed a skeletal class II due to maxillary protrusion and retrognathia, transversal micrognathism, vertical excess of the maxilla, upper and lower proclination and a neutral growth pattern (Table I).
Cephalometric values.
| Variable | Normal value | Deviation | Presurgical | |
|---|---|---|---|---|
| Dental | ||||
| Overjet | 2.5 | ± 2.5 mm | 5 mm | |
| Overbite | 2.5 | ± 2.5 mm | 6 mm | |
| IMPA | 90 o | ± 2 | 107 o | |
| U1-FH | 110 o | ----------- | 120 o | |
| Horizontal | ||||
| Maxillary depth | 90 o | ± 3 | 95 o | |
| Facial convexity | 2 ± 2 mm | Decreases 0.2 mm/year | 8.5 mm | |
| Facial depth | 87o ± 3 | Increases 0.3o/year | 87 o | |
| Mandibular corpus length | 65 ± 2.5 mm | Increases 1.6 mm/year | 71 mm | |
| Vertical | ||||
| Mandibular plane | 26o ± 4.5 | Decreases 0.3o/year | 25 o | |
| Maxillary height | 53o ± 3 | Increases 0.5o/year | 60 o | |
| Lower face height | 47o ± 4 | ---------- | 42 o | |
| Maxilla-mandible | ||||
| ANB | 5 o | ----------- | 9 o | |
| Wits | 2 mm | ----------- | 6 mm |
Treatment plan: once the objectives of treatment were established, a consultation was held with the Department of Maxillofacial Surgery of the Hospital Juarez in Mexico. It was suggested a sagittal surgery for mandibular advancement and an advancement genioplasty. Presurgical orthodontic treatment was planned for the surgical preparation of the patient.
Presurgical orthodontic phase: extraction of lower first premolars. 0.022” x 0.028” Roth appliances were placed. Alignment and leveling is done with light archwires.
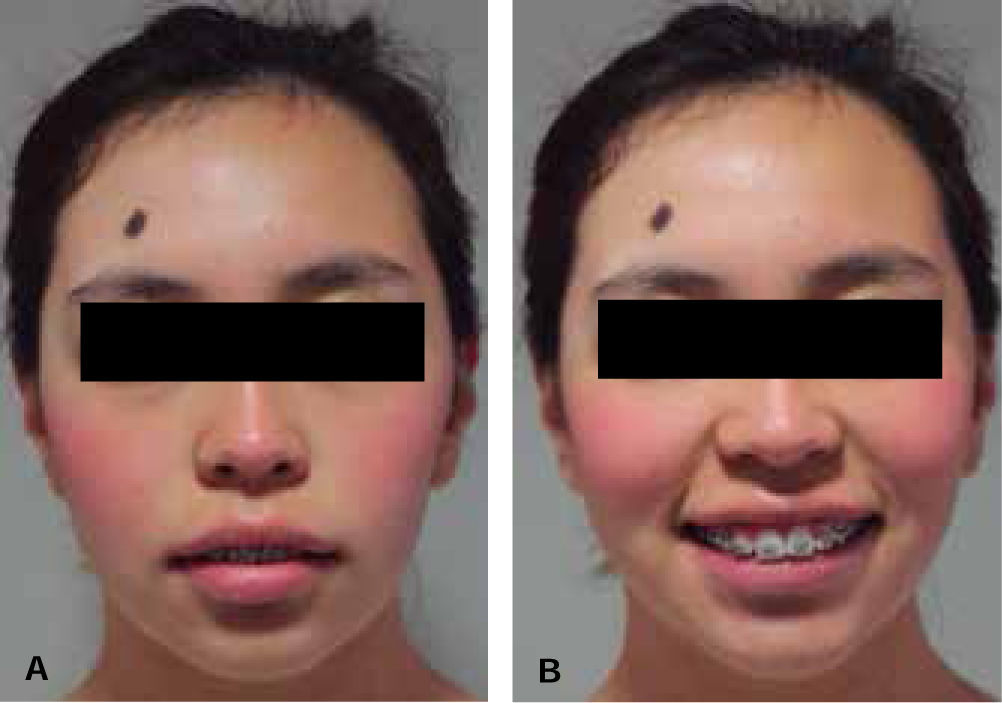
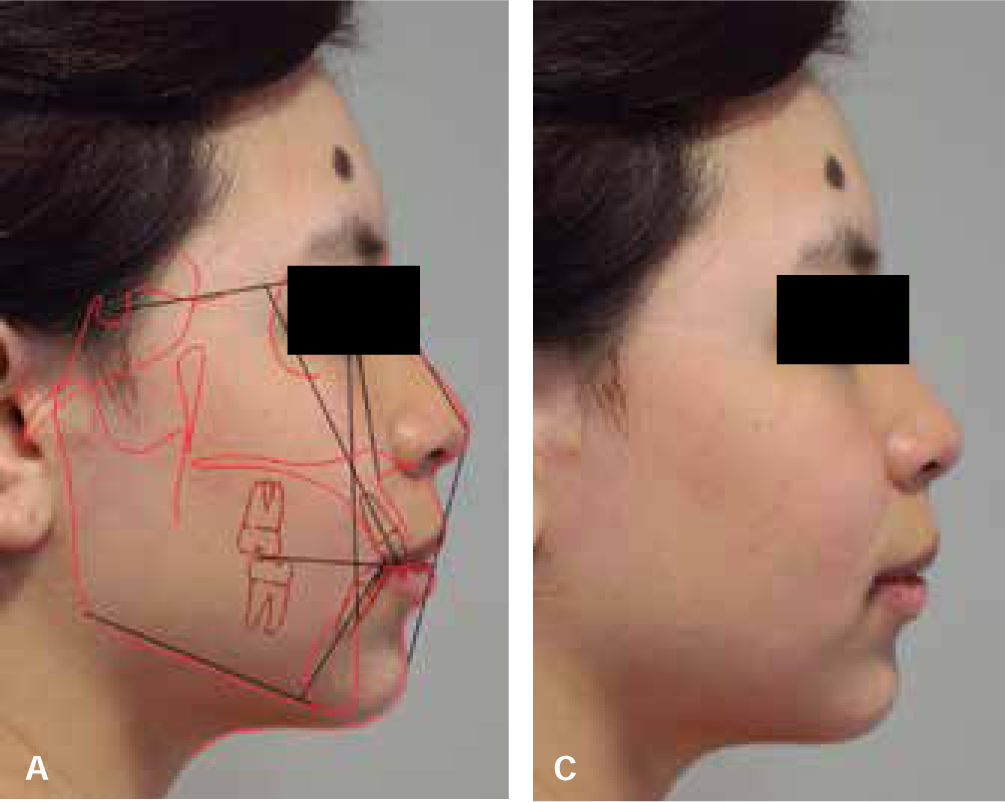
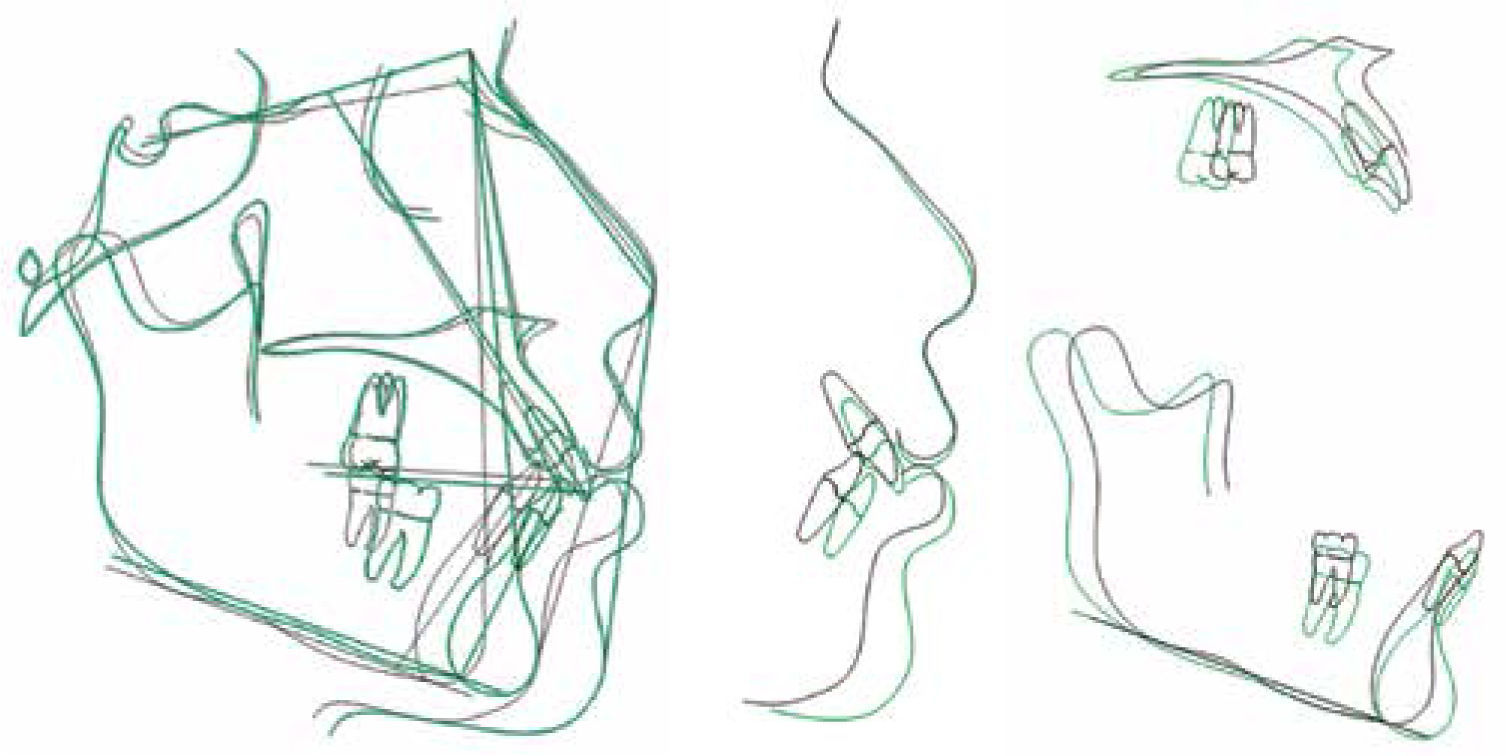
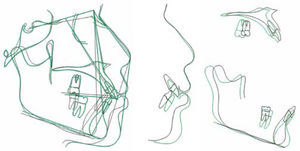
Presurgical decompensation was seen in the dental and facial features (Figures 6and7). Second and third order movements were carried out with the following archwire sequence: 0.016” x 0.016” NiTi up to 0.019” NiTi x 0.025” stainless steel (Figure 8). Prior to surgery radiographic records were taken (Figures 9and10) for cephalometric tracings and surgical prediction (Figure 11). Measurements and analysis were performed with the Dolphin Imaging 9.0 program. Surgery of models and the fabrication of the necessary occlusal splints for the surgery were performed in a semi-adjustable articulator.
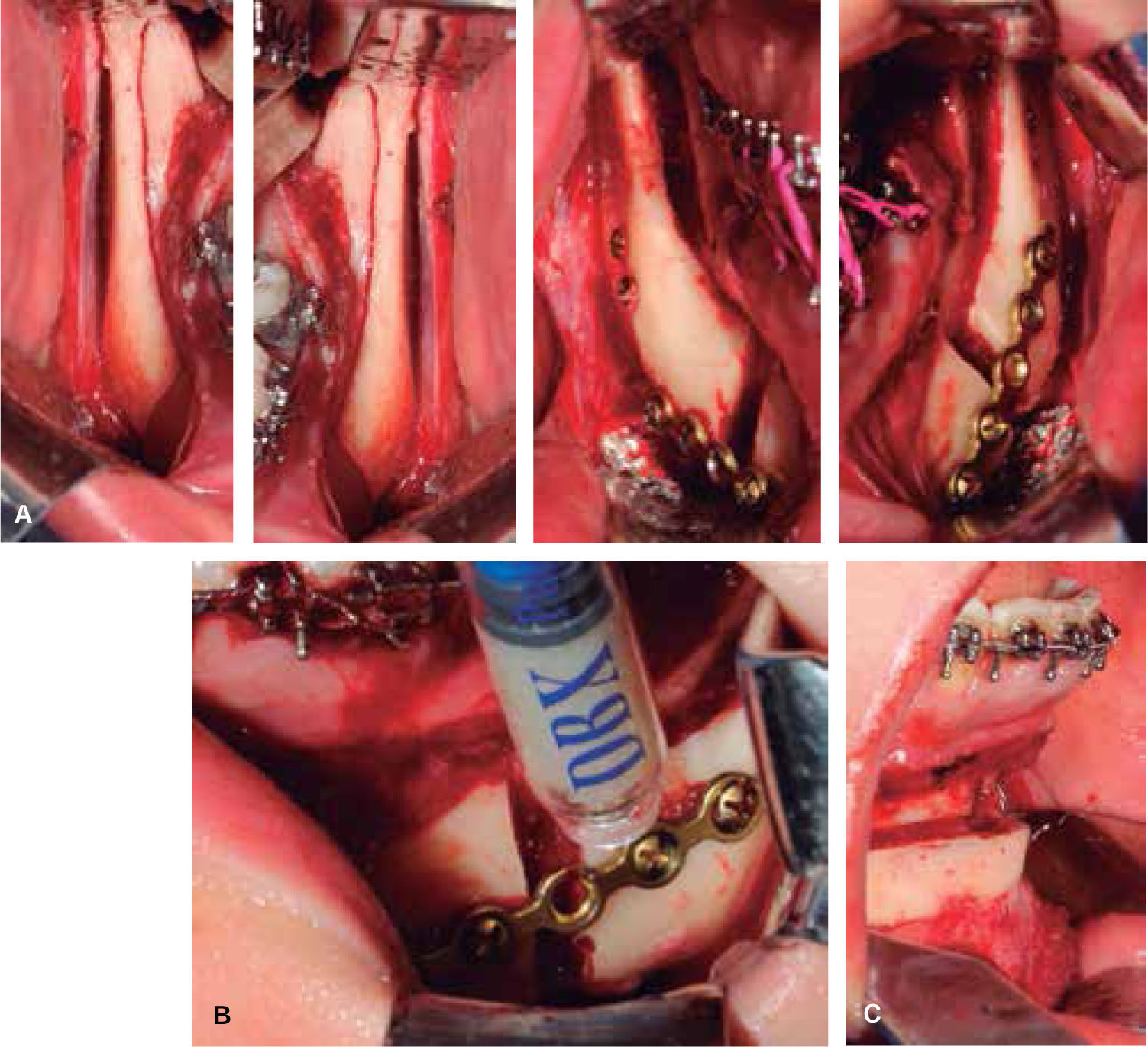
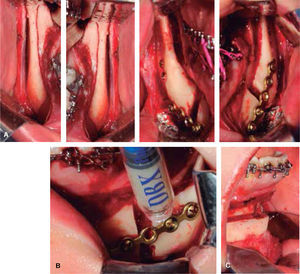
Surgical procedure: the surgery was performed with the aid of the Department of Maxillofacial Surgery of the Hospital Juarez in Mexico. A bilateral sagittal osteotomy was performed advancing the mandible 10 mm with bone graft using an intermediate splint for stabilizing the mandible in the correct position (Figures 12Aand12B). An advancement genioplasty of 6 mm was also conducted (Figure 12C). At the end of the surgery, the final splint was placed and elastic chain as intermaxillary fixation (Figure 13).
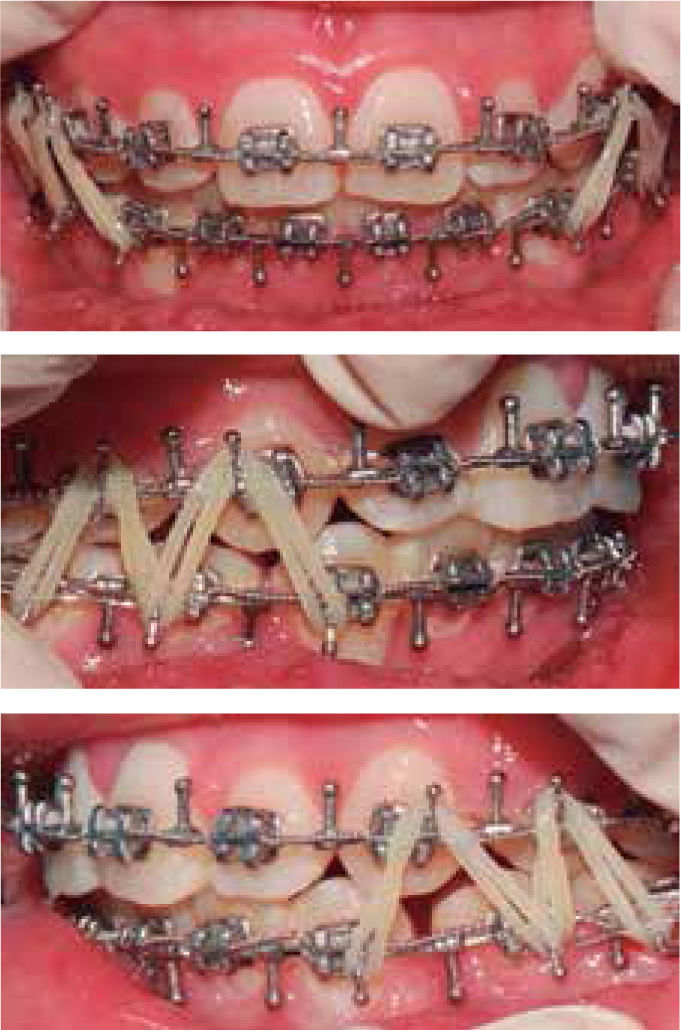
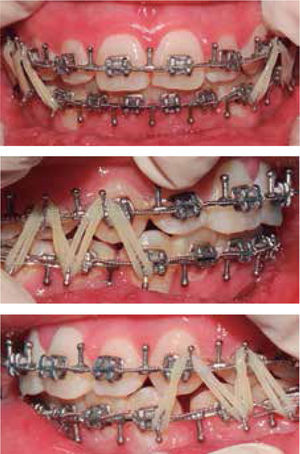
Postsurgical orthodontic phase: orthodontic treatment was resumed three weeks after surgery using up & down elastics for muscle control (Figure 14). The objective of this phase was to achieve an ideal occlusion in terms of Canine Class, overjet and overbite and the coincidence of dental midlines. 0.018” x 0.025” NiTi archwires were used and the use of elastics was continued. Subsequently, 0.019” x 0.025” archwires SS were placed for closure of residual spaces and finally 0.019” x 0.025” braided archwires were placed for refinement of intercuspation through elastics.
Twenty weeks after surgery the appliances were removed. Upper and lower circumferential retainers were Indicated for use during the day and a basic Bionator appliance of nocturnal use (Figures 15 to 17). Orthopantomography and lateral headfilm were taken after treatment (Figures 18and19), and the changes were assessed by superimposition (Figure 20). Additionally, cephalometric values were compared with the initial X-rays.
Total treatment time was 21 months. The profile was improved increasing the aesthetics and facial harmony of the patient.
DISCUSSIONIt is of the utmost importance to have an interdisciplinary approach during the planning of the surgical-orthodontic treatment for establishing objectives and obtain good results. Success in the surgical correction of dental-skeletal anomalies is determined by both the presurgical orthodontic treatment that eliminates dental compensation, and the correct surgical planning.6
After the evaluation and considering the soft tissues of the patient, the decision was made to start presurgical orthodontic treatment with the aim of achieving a good decompensation and preparing for surgery. In addition, a cephalometric prediction at the end of the presurgical phase was performed to corroborate the aims to be achieved during the surgical phase.
Sagittal osteotomies of the mandible in combination with pre- and post-surgical orthodontics are a consistent and effective method for the correction of class II division 1 malocclusions and for straightening of the facial profile. However, a negative effect of the treatment, counteracting the correction of class II, is an increase in the mandibular plane, as well as an increase of anterior face height and a decrease in posterior face height.7
In this case, by assessing and comparing the initial and final cephalometric data of the patient, it was noted that there was an increase in anterior face height, a decrease in the posterior face height and an increase in the mandibular in relation to SN plane.
The performed surgical movements have demonstrated to have a good post-surgical stability in addition to improving and harmonizing the facial aesthetics. The osteotomy for mandibular advancement and the advancement genioplasty significantly improved the profile of the patient.
The duration of the postsurgical orthodontic phase depends on the degree of preparation that was achieved during the presurgical phase.8 In this case, it had a duration of 20 weeks, during which light elastics were used to counteract the proprioceptive impulses of the teeth and have a proper neuromuscular control which led to finish with an adequate dental retention which in turn contributes to the occlusal stability in the long term.
Having knowledge of the occlusal and facial changes that surgical movements produce, is the key to improving the facial harmony of patients who undergo this type of treatment.
CONCLUSIONSThe decision of how to conduct an optimal treatment for a class II adult patient is based on a wide range of research including clinical, radiological, study models and photograph examinations. A detailed analysis of these photographs is a useful way of quantifying the facial features that are important for diagnosis and treatment plan.
Surgical-orthodontic treatment leads to produce harmonious facial, skeletal and soft tissue relationships and to improve occlusal function.
Sagittal osteotomies of the mandible in combination with pre- and postsurgical orthodontics is an excellent treatment alternative for adults with a class II division 1 malocclusion since occlusal sagittal relations are corrected and the hard and soft profiles are straightened in a harmonious way, which is the main objective of the treatment in patients with class II with a convex facial profile.
Malocclusions may lead to social disadvantages and affect the life of the patient. It has been proven that attractive people are considered more intelligent, socially competent, with a positive personality, have better social interactions and have a better professional development. One of the main reasons why an adult class II patient seeks treatment is dental and facial aesthetics. The more dissatisfied patients are with their facial appearance, the more likely it is for them to choose surgical treatment instead of an orthodontic treatment only.
Regardless of the type of malocclusion in question, the patient's cooperation is essential to achieve the objectives and satisfactory results at a dental, facial and psychological level.