To present a case report of the orthodontic management of an adult female patient with inactive periodontal disease, skeletal Cl II with proclination, protrusion, extrusion and multiple missing teeth.
MethodsAn interdisciplinary treatment plan with periodontics and prosthodontics was determined. MBT 0.022” fixed orthodontic appliances, light forces and contraction archwires were used to correct overerupted teeth, proclination, protrusion and spacing in the upper arch. Stripping was made to reduce interdental black triangles.
ResultsProclination, protrusion and extrusion decreased. Adequate overjet and overbite were achieved, tooth mobility was reduced and the periodontal condition was improved.
ConclusionsOrthodontic treatment in adult patients with periodontal disease is limited but it helps achieve better function, aesthetics and integrity of periodontal tissues as well as facilitates the management of future prosthetic rehabilitation.
Presentar el manejo ortodóncico de un paciente femenino adulto con enfermedad periodontal inactiva, Cl II esquelética con proinclinación, protrusión, extrusión y múltiples pérdidas dentarias.
MétodosSe determinó un plan de tratamiento interdisciplinario con las Especialidades de Periodoncia y Prótesis Bucal e Implantología. La aparatología ortodóncica utilizada fue Roth 0.022”, se manejaron fuerzas ligeras, se colocaron arcos de contracción, dobleces de intrusión para corregir la extrusión, proinclinación, protrusión y los espaciamientos en la arcada superior. Se realizaron desgastes interproximales para reducir triángulos negros interdentales.
ResultadosDisminuyó la proinclinación, protrusión y extrusión. Se consiguió mejor sobremordida tanto vertical como horizontal, se redujo la movilidad dentaria y mejoró su condición periodontal.
ConclusionesEl tratamiento de ortodoncia en pacientes adultos con secuelas de enfermedad periodontal es limitado pero ayuda significativamente a conseguir mejor función, estética, integridad de los tejidos periodontales y facilita el manejo de una futura rehabilitación protésica.
Orthodontic treatment is increasingly common in adult patients in whom chronic periodontitis, decreased bony support, tooth movility or loss as well as attachment lossmay appear more frequently than in younger patients.1,2 This is why the collaboration of specialists of different dental areas should be taken into consideration when performing a multidisciplinary treatment plan for the management of these cases.
It is of outmost importance that before orthodontic treatment begins, active inflammation of the supporting tissues is eliminated and maintained inactive during and after orthodontic treatment.3
Studies show that orthodontic treatment is not a contradiction in the treatment of severe adult periodontitis in fact orthodontics improves the possibilities of saving and restoring a deteriorated dentitionin many cases.4
ObjectiveTo show the orthodontic management of an adult female patient with inactive periodontal disease, skeletal Class II with proclination, protrusion, extrusion and multiple extracted teeth.
METHODSA 54 year-old female patient attended the Orthodontics Clinic of the Postgraduate Studies and Research Division of the Faculty of Dentistry of the National Autonomous University of Mexico. She was referred from the Periodontics Clinic where conventional treatment for chronic periodontitis was performed. Periodontal treatment included root scaling and planning and plaque control. The patient attended the Orthodontic clinic with inactive periodontal disease and with the aim of improving her teeth's position.
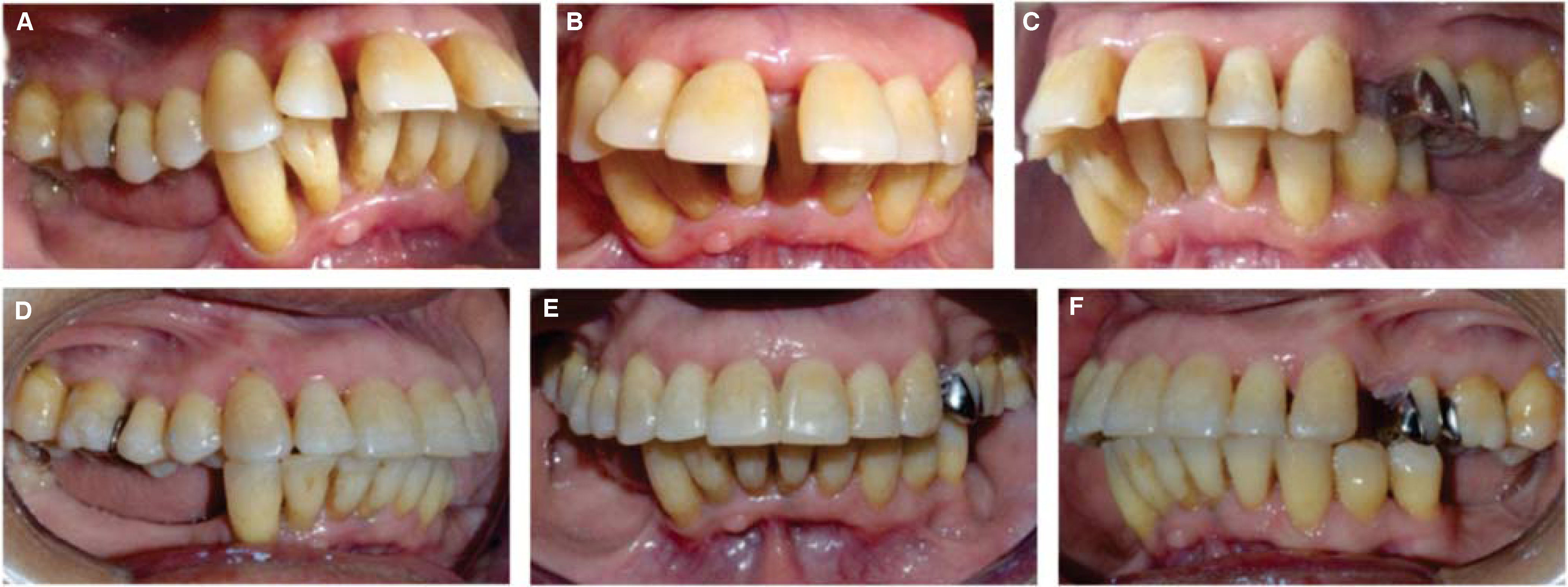
Facial photographs analysis revealed a convex profile, upper and lower lip protrusion, decreased nasiolabial angle, narrow buccal corridors, upper and lower incisor extrusion (Figure 1).
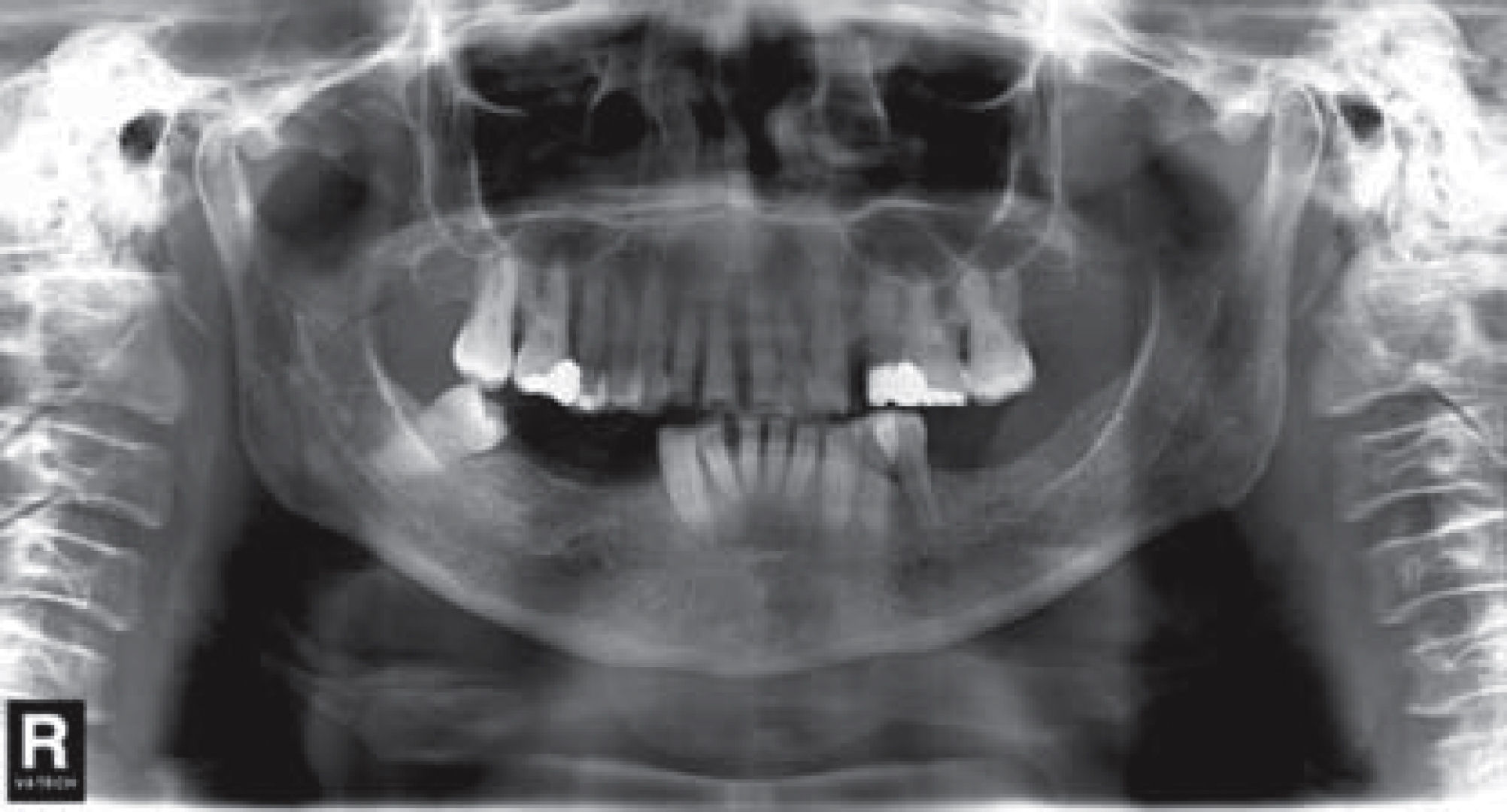
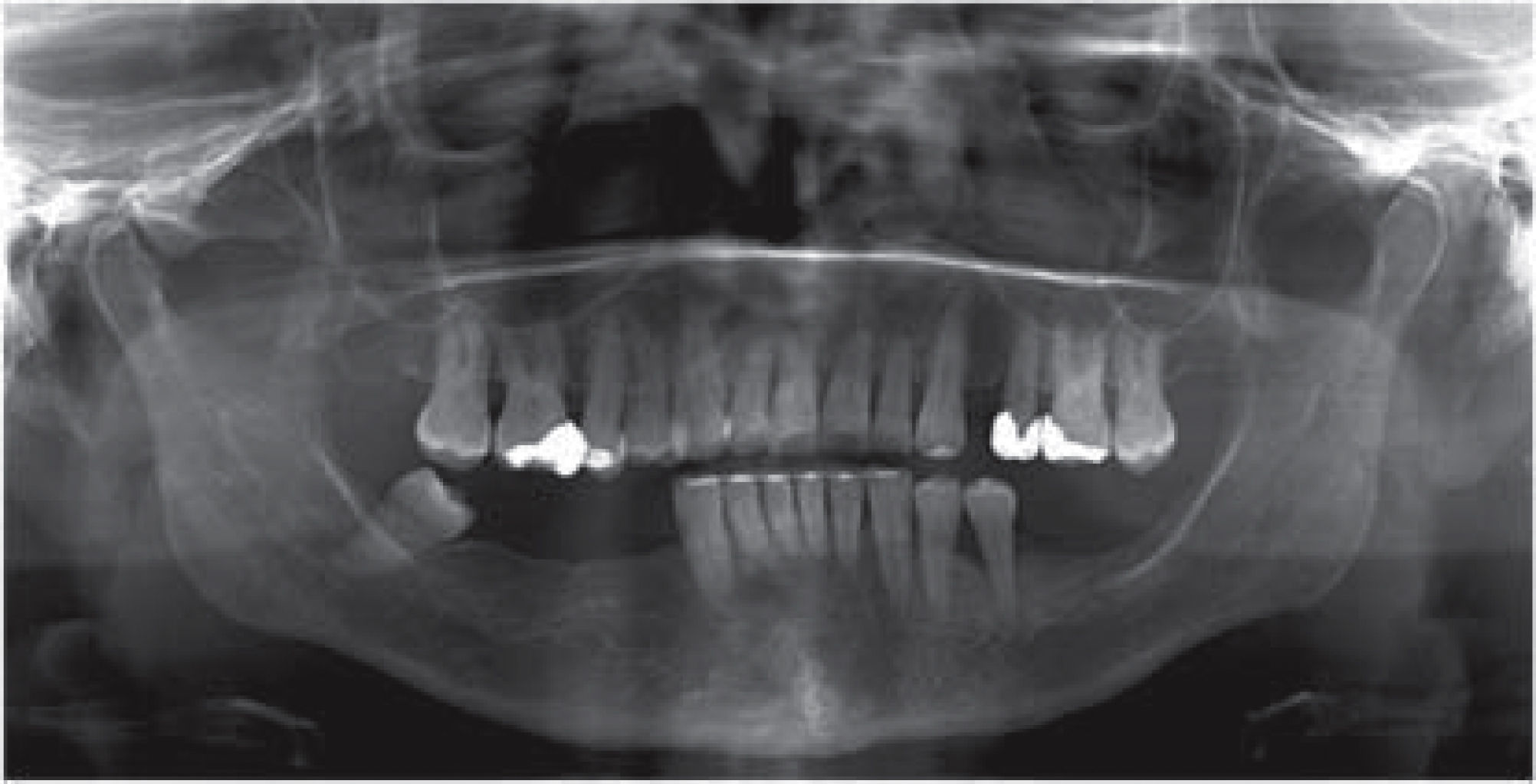
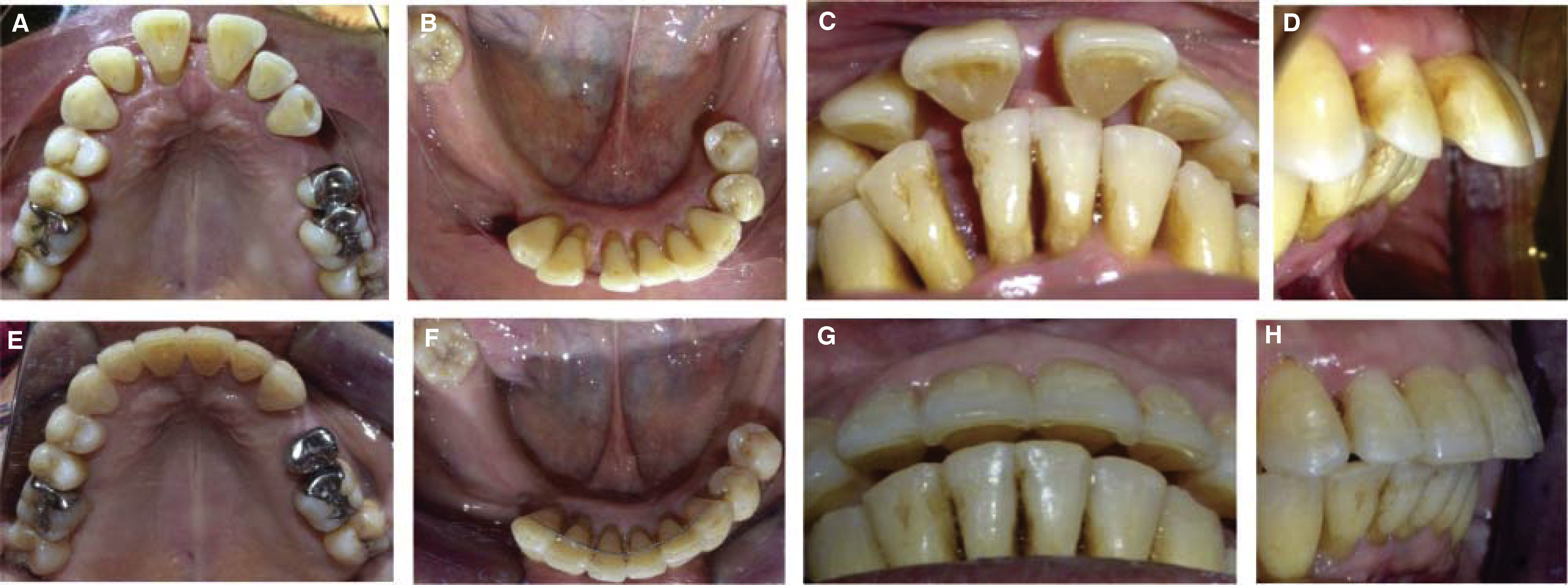
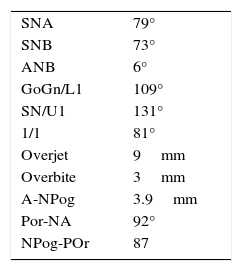
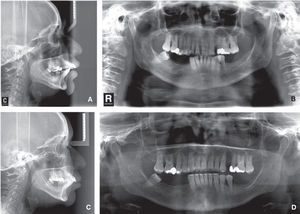
Her dental photographs and radiographs show upper and lower incisor proclination and protrusion, spacing, increased overbite and overjet, canted occlusal plane, loss of multiple teeth, telescopic bite of the upper left second premolar and extrusion of upper and lower teeth (Figures 2 to 4)
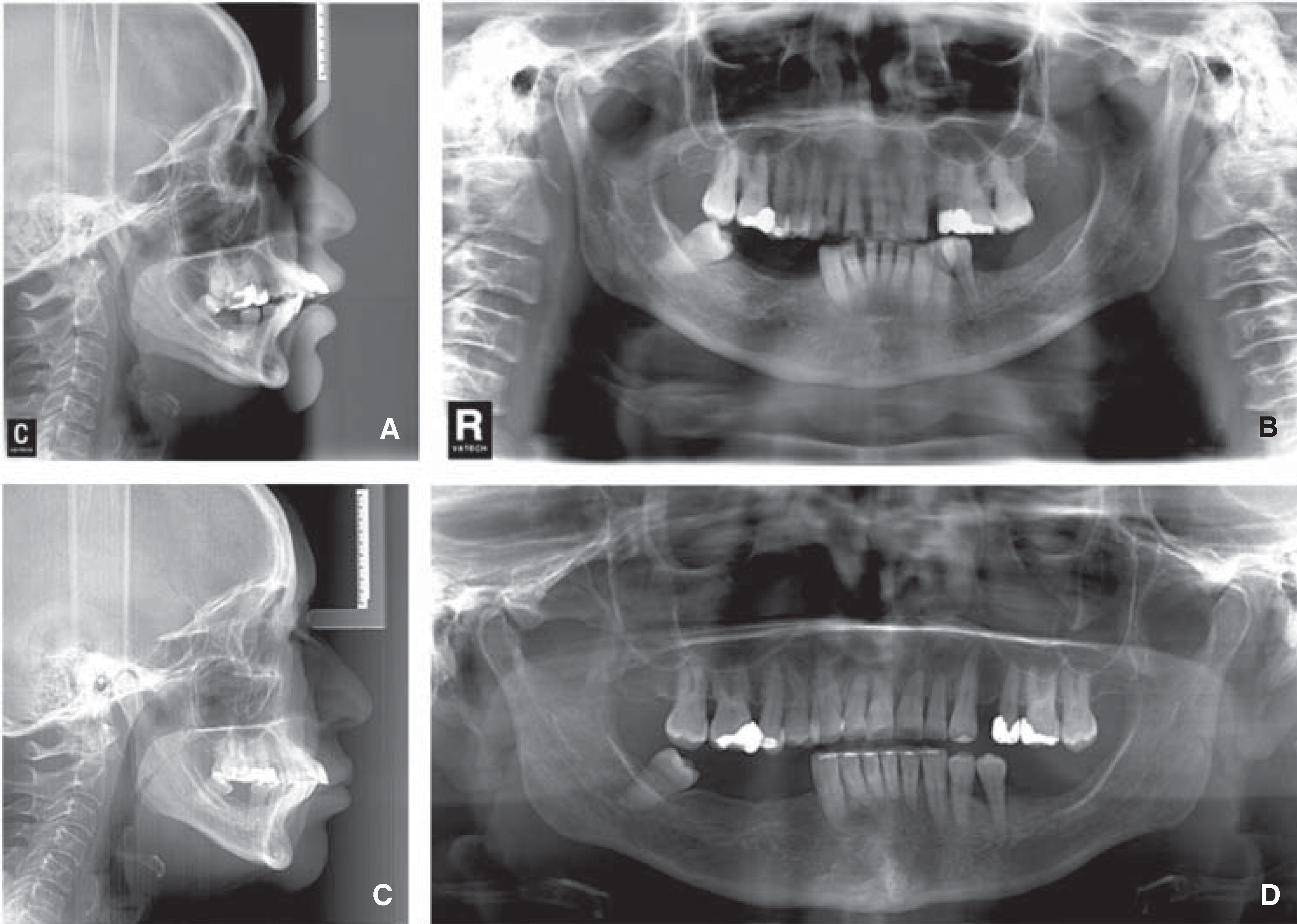
With the results obtained from the measurements of Jarabak, Downs, McNamara, Steiner, Ricketts and UNAM cephalometric analysis, the following cephalometric diagnosis was determined: skeletal class II due to maxillary protrusion and mandibular retrusion with upper and lower dental proclination and protrusion and vertical growth (Table I).
Treatment objectives were aimed at improving the patient's periodontal health, stability, function and esthetics. Among these objectives were the following: to maintain periodontal disease inactive, to improve the patient's soft tissue profile, to reduceupper and lower protrusion and proclination, intrude upper anterior teeth, close spaces, to improve the overbite and overjet and correct dental rotations.
Treatment sequence0.022” sloth Roth metal brackets and 0.014” NiTi archwires were placed to begin alignment and leveling. Retraction of the upper anterior segment was initially undertaken with 0.014” stainless steel arches with contraction bends. Then 0.016” stainless steel archwires were used with contraction and intrusion bends for the central and lateral incisors. In the lower arch, 0.014” stainless steel archwires were used with half- T bends to correct the lower left second premolar.
Interproximal reduction was performed in the upper arch and closed elastic chains were placed from lateral incisor to lateral incisor. The remaining space was closed with 0.016” SS archwires with contraction bends. Lingual buttons were placed on the upper right second premolar and lower right second premolar with 3/16 inches and 3.5 ounces elastics to uncross the bite. In the lower arch, afixed retainer from canine to canine made with 0.175” twisted wire was placed and on the upper arch, a removable circumferential retainer (Figures 5 and 6). The patient was sent to the Department of Oral Implantology and Prosthetics at the Faculty of Dentistry of the UNAM for the final rehabilitation.
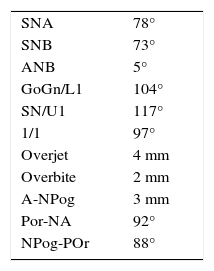
RESULTSAt the end of treatment, which lasted 23 months, the results were satisfactory. The objectives posed at the beginning of the treatment were achieved, both facial and dental: the facial soft profile was improved due to a reduction of the biprocheiliaand an increase in the nasolabial angle that went from 61° to 80°.
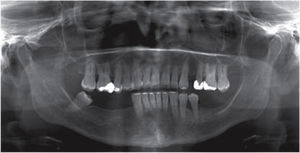
The upper and lower protrusion and proclination was reduced, interdental spaces were closed, both the overbite and overjet were reduced and the rotations, corrected. The upper and lower dental extrusion improved and the unilateral left posterior crossbite was corrected (Figure 7).
The supporting tissues showed a healthier appearance. Neither the gingival recessions nor the bone loss increased (Figures 6, 8 to 10). The expression of the smile improved considerably (Figures 11 and 12).
There were improvements in the results of the final cephalometric analysis since the values approached normal standards (Table II). It must be taken into consideration that the case was limited due to the existing periodontal condition at the beginning of the treatment (Figure 13).
Several articles claim that during orthodontic treatment it is common to onset or worsen certain periodontal pathologies because of the effects produced by fixed appliances in the oral environment.5 In a study by Bollen, Cunha-Cruz, Bakko, Huang and Hujoelit was concluded that orthodontic therapy causes minor damage to the periodontium and in their systematic review they did not find evidence of a positive effect of orthodontics over periodontal health.6
However, proper orthodontic treatment in patients who maintain an excellent oral hygiene and who do not present periodontal disorders does not imply a significant risk.5 Authors such as Tortolini and Fernandez argue that periodontal patients benefit from orthodontic treatment specially when performing certain tooth movements which may be favorable for a reduced periodontium.3
Studies confirm that periodontal tissue destruction prior to orthodontic treatment is no contraindication for treatment. Orthodontic therapy increases the chances of preserving and restoring a damaged periodontium and relapse of activepathological process does not increase during therapy with orthodontic appliances.7 However, if orthodontic treatment isperformed without having treated the illperiodontium, it increases the rate of treatment failure, since orthodontic appliances and forces may contribute to an increased retention of dental plaque and further destruction of the periodontalsupport structures.5
The use of adequate orthodontic mechanics is necessary in patients with a compromised periodontium because it must be carried out differently than conventional orthodontics. Correct tooth positioning through intrusion, retrusion, alignment and leveling should be performed through the use of light forces throughout treatment. It has been shown that in addition to improving function and aesthetics, orthodontic tooth movement helps prevent inflammation and relapse of periodontal disease.8
CONCLUSIONSOrthodontic treatment in adult patients with sequelae of periodontal disease is limited but significantly helps achieve better function, aesthetics and preserve the integrity of periodontal tissues. It also facilitates future prosthetic rehabilitation.
These patients should have constant monitoring of periodontal tissues and keep under control the dentobacterial plaque. The Orthodontics-Periodontics relationship must be kept in all stages of orthodontic treatment.
Orthodontics based on evidence should be applied by orthodontists in all treatments, especially in complex cases that require a multidisciplinary team or where several areas of the stomatognathic system are compromised.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Student of the Orthodontics Specialty of the Division of Post-graduate Studies and Research, Faculty of Dentistry UNAM.
Professor of the Orthodontics Specialty of the Division of Post-graduate Studies and Research, Faculty of Dentistry UNAM.