To describe a case of an elder female skeletal Class I patient with chronic periodontitis after-effects who underwent orthodontic treatment.
MethodsAn interdisciplinary approach was established to rehabilitate the patient. In the orthodontic area, Roth 0.018 fixed appliances were used and stripping was performed in order to correct the spacing, protrusion and torque of the anterior teeth. Intrusion of the upper anterior segment was also performed. Retention on the upper and lower arch was fixed with individual bonding from canine to canine.
ResultsMolar class was maintained since the patient had fixed prosthesis on the posterior area. The after-effects of periodontitis were improved as well as the quality of the periodontal tissues.
ConclusionsThe treatment of the elder patient requires a close interdisciplinary approach with every area of competence due to the multiple conditions that they frequently suffer from. Although orthodontic treatment is limited, the living quality of these patients is improved.
Describir el caso de un paciente femenino adulto mayor clase I esquelética con secuelas de periodontitis crónica a quien se le realizó tratamiento de ortodoncia.
MétodosSe estableció un tratamiento interdisciplinario para rehabilitar a la paciente. En el área de ortodoncia, se utilizó aparatología Roth 0.018 y se realizaron desgastes interproximales para corregir el espaciamiento, la protrusión y la inclinación en los dientes anteriores. También se realizó intrusión del segmento anterior superior. La retención fue fija con bondeado individual de canino a canino superior e inferior.
ResultadosLa clase molar se mantuvo, debido a que la paciente presentaba prótesis fijas en el sector posterior. Se mejoraron las secuelas de periodontitis y la calidad de los tejidos periodontales.
ConclusionesEl tratamiento del paciente adulto mayor requiere una interdisciplina muy cercana en todas las áreas que le competen debido a las múltiples afecciones que generalmente los aquejan. Aunque el tratamiento ortodóncico presenta limitaciones, la calidad de vida de estos pacientes se ve mejorada.
According to the National Institute for Elderly Adults, an elderly person is the one that has a biological age of 60 years or more.1 According to the Informational File of 2005 of the National Population Council, the population aged 60 years or more is the one that grows more quickly since twenty years ago and presents a rate with the potential to double its size in less than two decades.2 In Mexico, there are currently 8.2 million elderly adults who represent 7.7 percent of the total population, but the rate of annual increase indicates that by the year 2050 there will be 36.2 million older people, i.e. one out of four Mexicans.2
It can be expected that the demographic acceleration presented by this population is reflected in the number of elderly patients seeking orthodontic care. It can also be expected that as life expectancy increases and health services improve, the population over 60 years will participate more actively in society and reveal the desire to preserve their dentition functionally and aesthetically on the long-term. Currently the challenge of an increase in the elderly population in a short period of time must be faced. The orthodontist, and every health care professional, must be trained to respond to these demands from society.
Biology of the periodontumAge itself is not a contraindication for orthodontic treatment. However, it is important to bear in mind that in elderly patients, tissue response to orthodontic forces is much slower. This is due to a decreased cellular activity and that to the fact that tissues become richer in collagen.
ObjectiveTo describe the case of a female elderly patient skeletal class I with sequelae of chronic periodontitis who underwent orthodontic treatment.
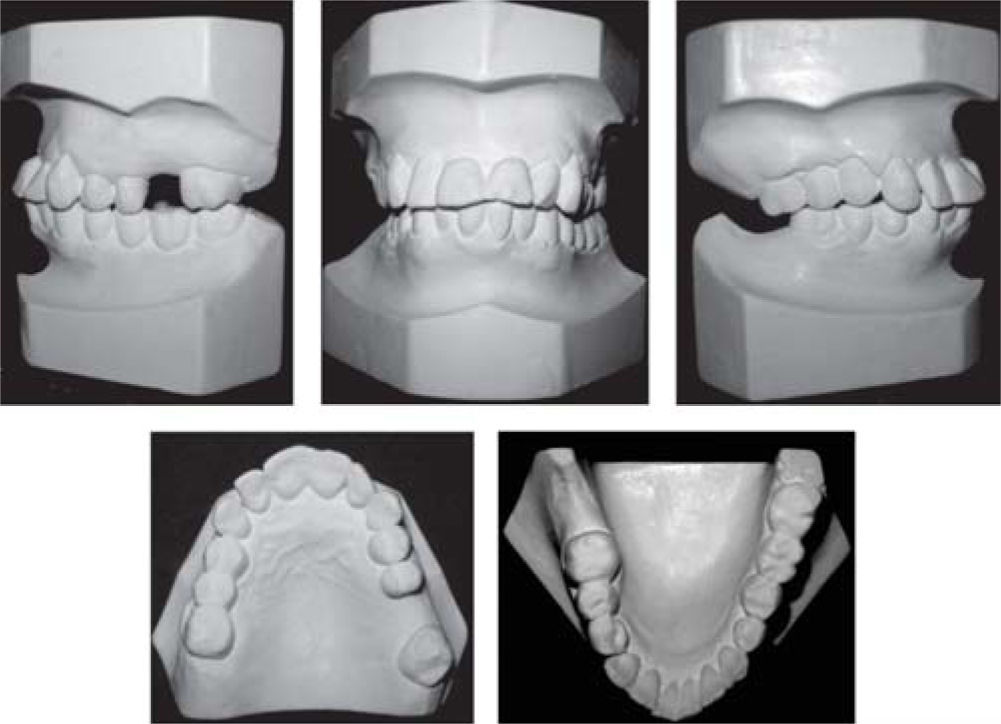
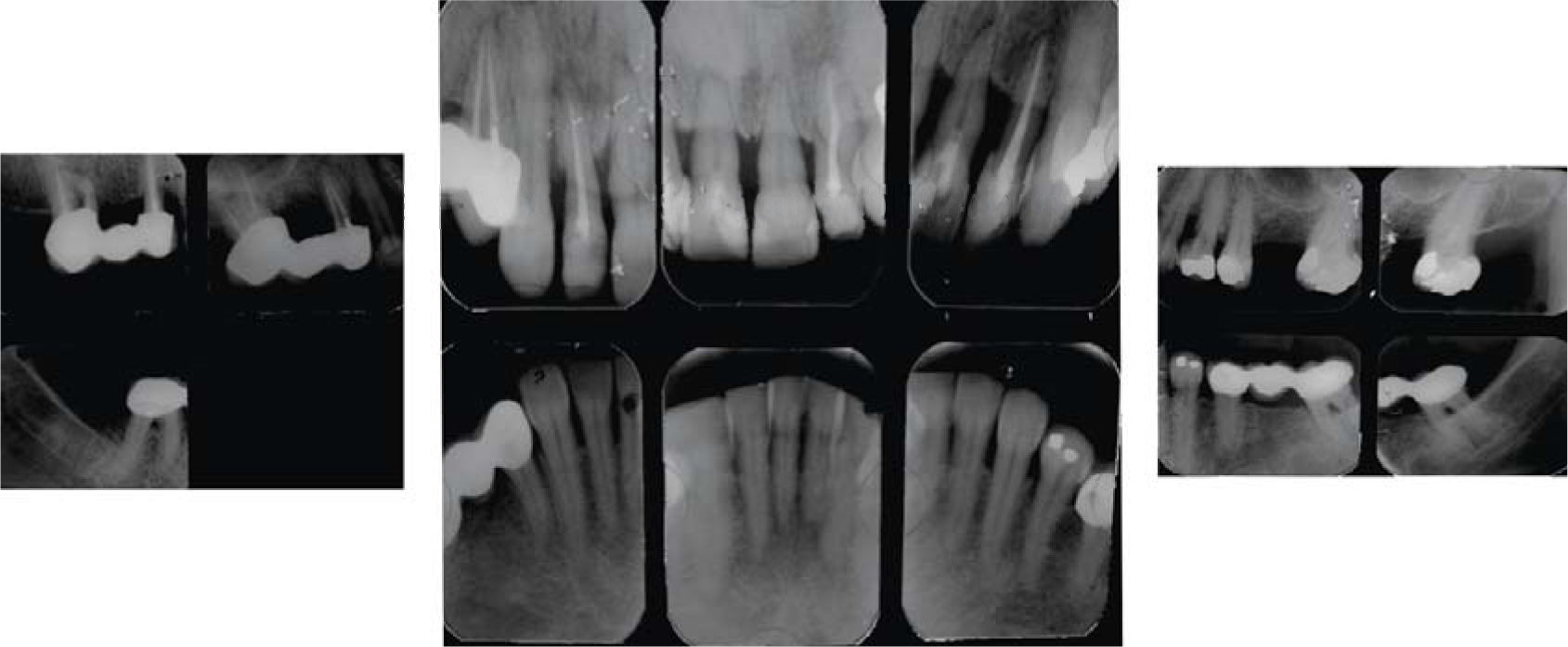
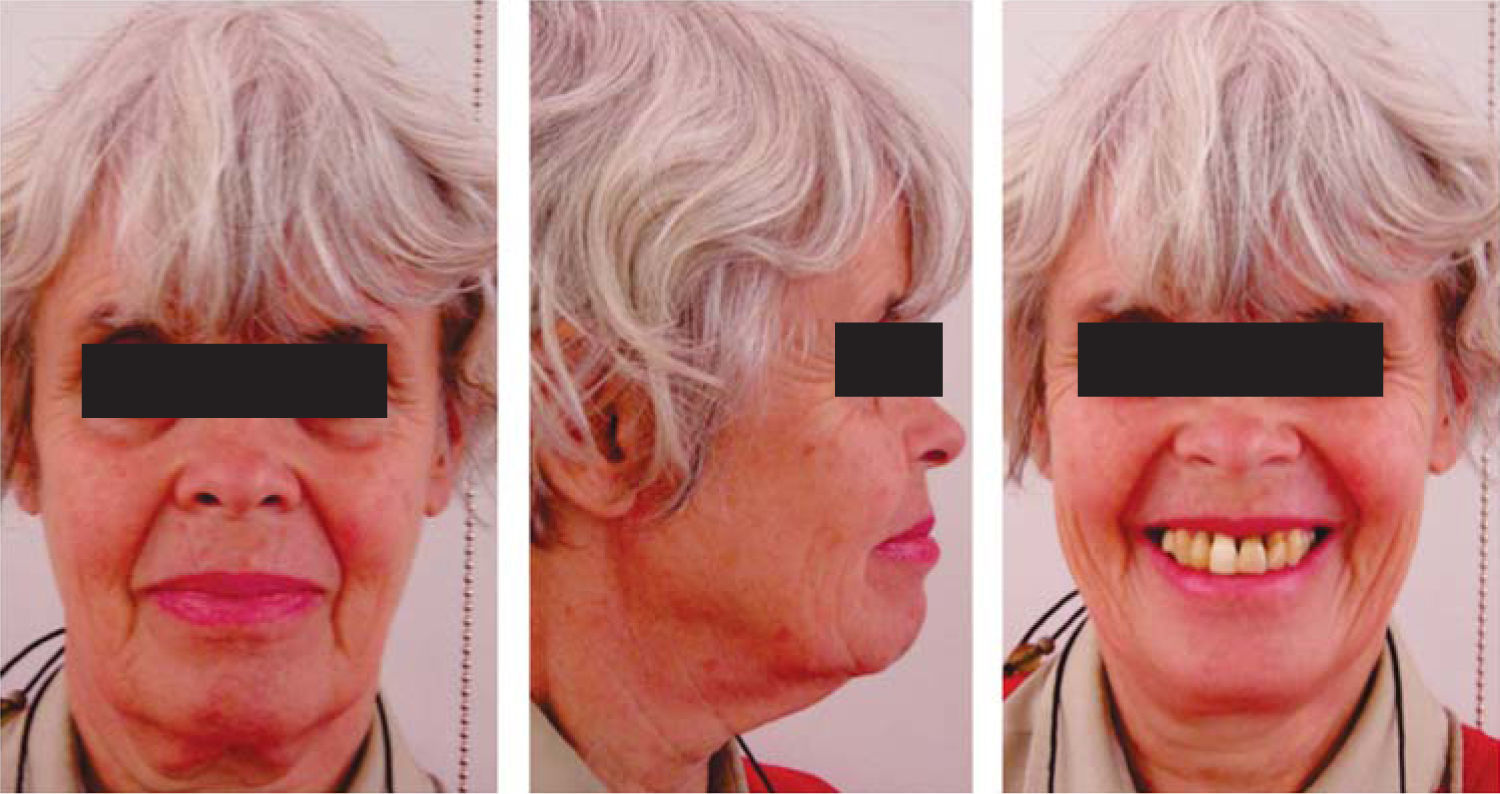
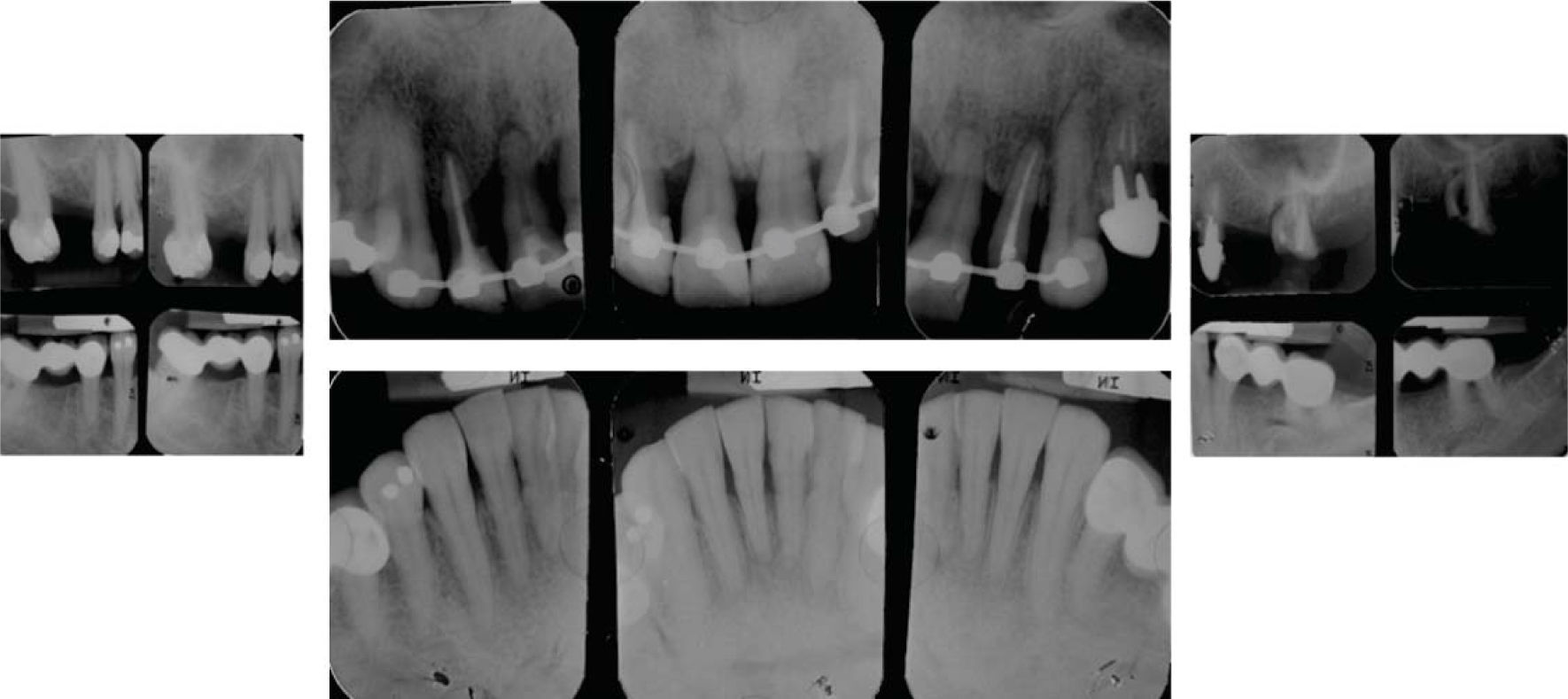
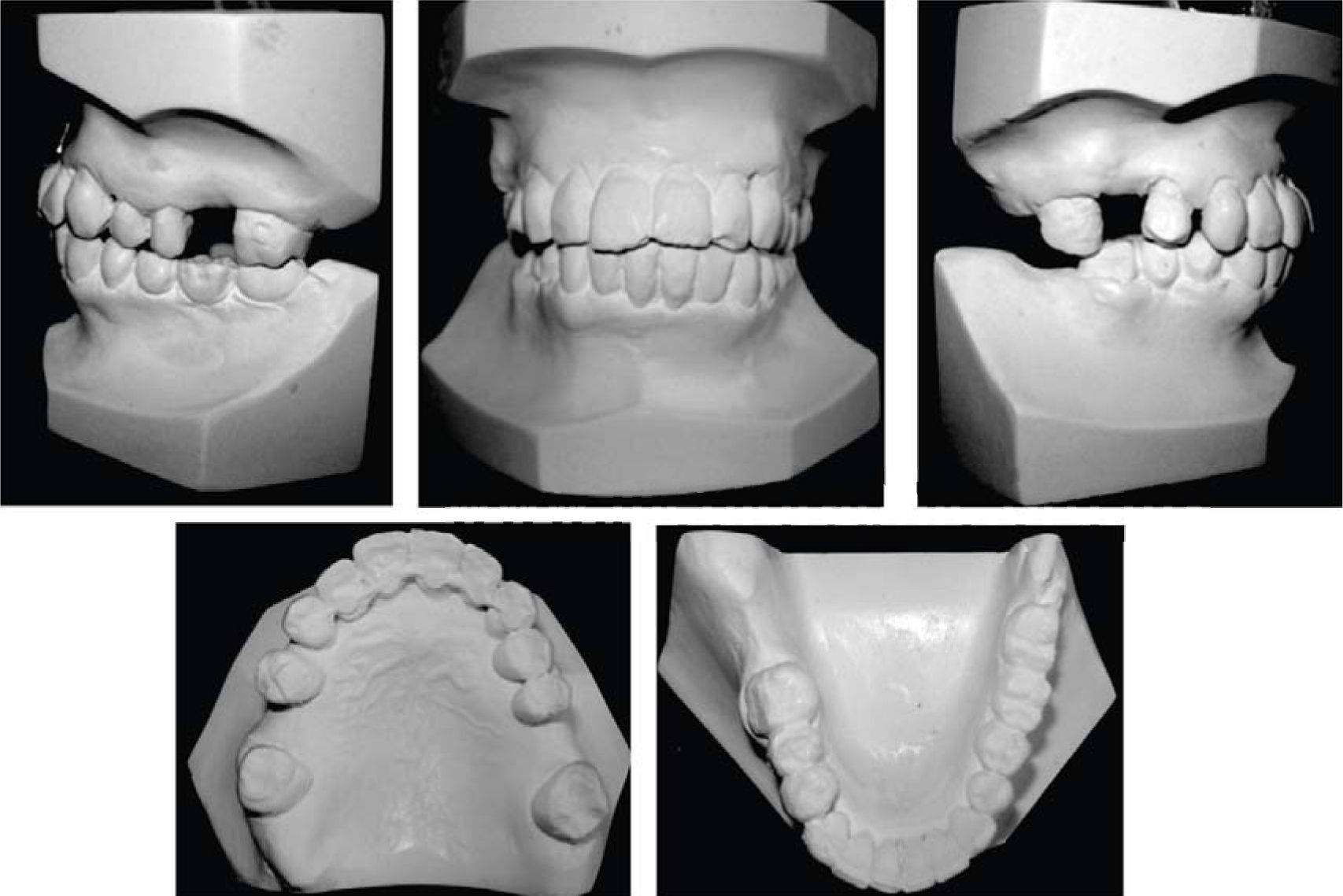
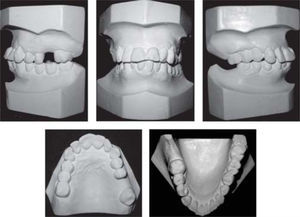
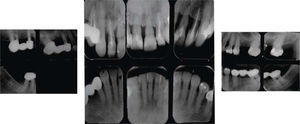
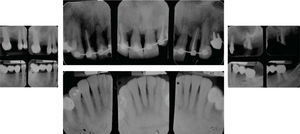
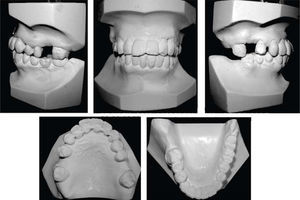
MethodsDiagnosis and etiologyA 60-year-old female patient attended the Orthodontics Clinic at the Postgraduate Studies and Research Division of the Faculty of Dentistry. The patient had been diagnosed with chronic periodontitis 30 years ago and remained in intermittent control with a private dentist, but when her economic situation worsened, she decided to attend the Periodontics clinic of the Faculty of Dentistry. In this clinic during four months, conventional periodontal treatment was performed which included scaling and root planing in the entire dentition and surgical periodontal therapy. The reason for orthodontic consult was to improve aesthetics and function, as well as to improve the quality of support tissues in the anterior maxillary area. During facial analysis, it was determined that the patient had mesofacial pattern with a harmonious balance and a straight profile (Figure 1). Upon initial intraoral exploration the following was noted: loss of multiple dental pieces; presence of restorations and fixed prostheses; several sequelae of periodontal disease such as recessions, loss of the interdental papilla, inclinations, extrusions and spacings (Figure 2). In the initial panoramic and dentoalveolar series, general bone loss was observed, especially in the upper anterior sector (Figures 3and4).
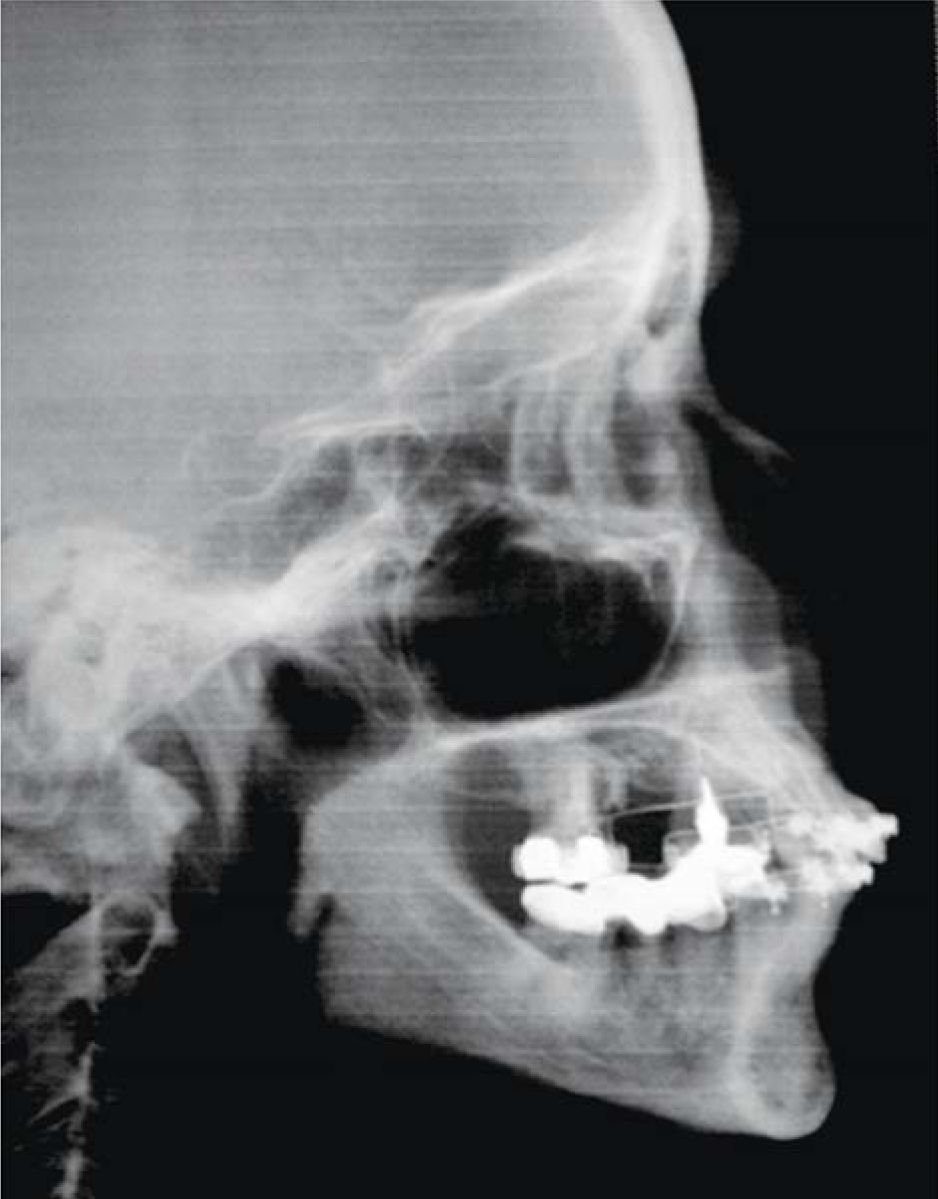
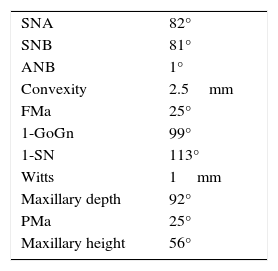
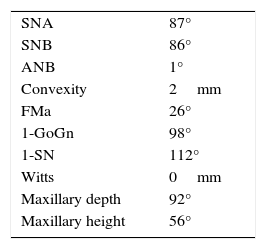
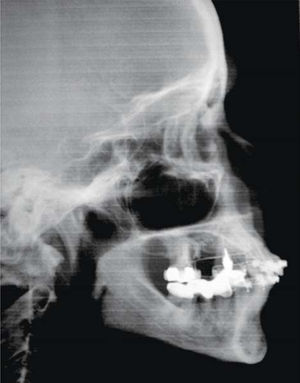
The patient was diagnosed as skeletal class I (Figure 5) with Class III molar, upper dental protrusion and proclination and interdental spacings in the upper and lower anterior area. The mandibular teeth showed slight crowding and loss of the interdental papilla (Figures 1 to 6). The cephalometric analysis showed an ANB angle of 1° and a mandibular plane angle of 23° (Table I).
Treatment goalsThe objectives for this patient were: to improve teeth position for subsequent prosthetic rehabilitation, to improve esthetics and periodontal health. For this purpose, it was decided to carry out the following: 1) improve dental protrusion, 2) Correct the axial axis of the upper incisors, 3) close spaces to create adequate interdental contacts that facilitate hygiene, and 4) intrude the upper front teeth in order to improve the vertical overbite.
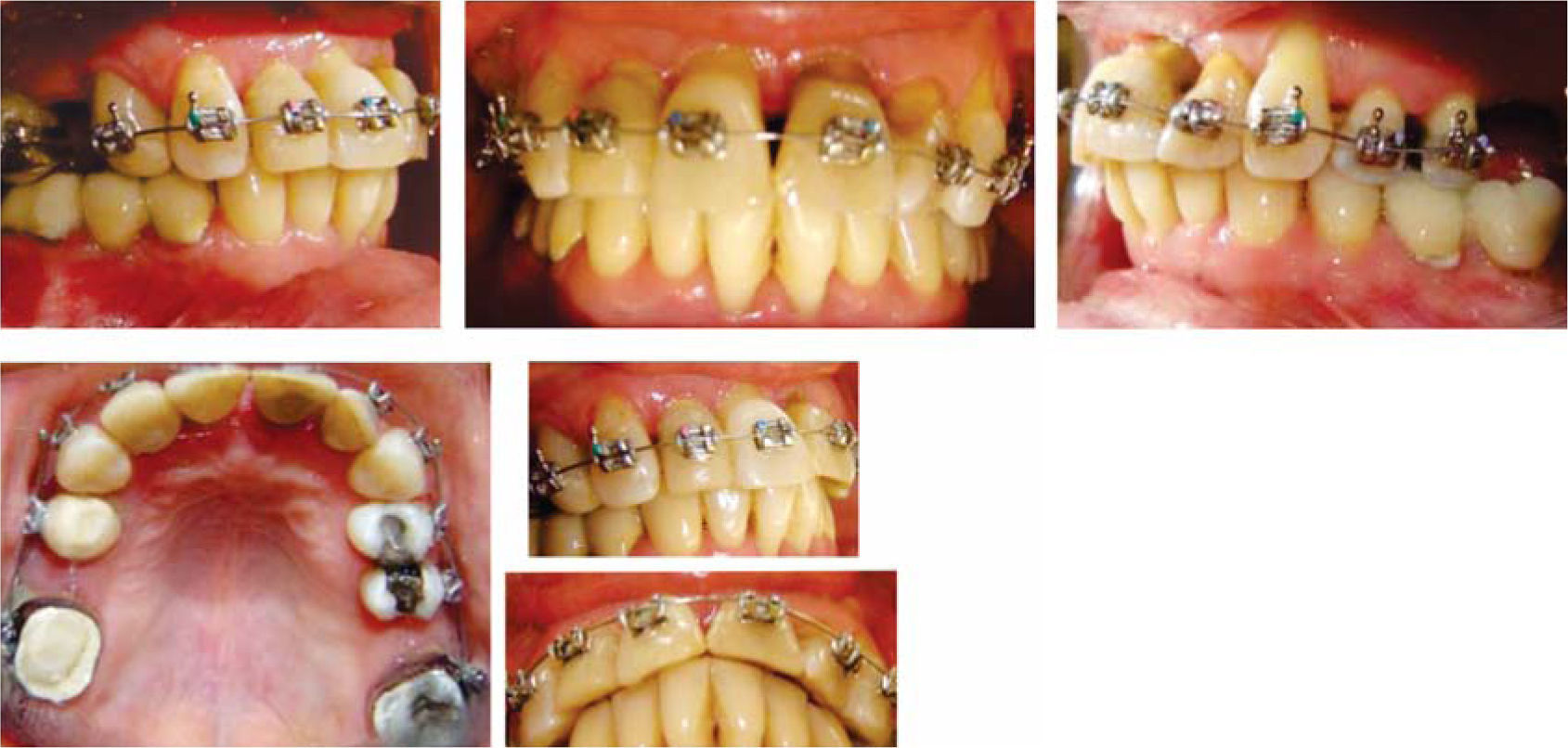
Treatment planThe patient signed an informed consent which informed her the diagnosis, therapy, potential consequences and complications. The treatment plan was considered without extractions and 0.018 Roth fixed appliances were placed (GAC International Inc. Knickerbocker Avenue 355, Bohemia, New York, USA) placing the brackets of the upper incisors at a height of 3.0mm from the incisal edge, to achieve greater intrusion. The initial alignment and leveling was carried out with 0,016 Nickel-Titanium arches (Borgatta Specialties. 55 Relaciones Exteriores St., Distrito Federal, Mexico) (Figure 7). Afterwards, interproximal recontouring was performed in the upper front teeth and subsequently on the lower. Space closure to reestablish contact points thus improving the loss of interdental bone crest and interdental papillae was obtained by using elastic chains and strand (Borgatta Specialties. 55 Relaciones Exteriores St., Federal District, Mexico).
Retraction and intrusion of the anterior segment was made with 0,016 stainless steel archwires (Borgatta Specialties. 55 Relaciones Exteriores St., Distrito Federal, Mexico) with contraction and intrusion bends (Figure 8). Once this was achieved, a 0.016×0.016 utility Blue Elgiloy® (Rocky Mountain Orthodontics, Denver, Colorado, USA) archwire was placed with intrusion activation in the upper anterior segment. In the lower arch, a 0.016×0.016 sectional Blue Elgiloy® was used to begin with slight movements of second and third order. Final settlement was carried out by 0.016×0.016 Blue Elgilloy® archwires (Figure 9). Retention was fixed from canine to canine in both the upper and the lower arch with Respond Dead Soft wire (ORMCO, Glendora, California, USA) bonded individually (Figure 10). Total time treatment was 20 months. The patient was referred to the Department of Prosthetics for rehabilitation of the posterior area.
ResultsTreatment for this patient respected her facial and skeletal features due to the fact that they were considered adequate (Figure 11,14and15). The molar class was left the same because it was determined by three-unit- fixed prostheses in the lower arch. An adequate overbite and overjet was achieved although the lower midline remained slightly diverted in order to preserve canine class I (Figure 10). The bucco-lingual inclination of the upper and lower anterior teeth was improved (Table II). The mesio-distal tipping of the upper right lateral incisor could not be corrected satisfactorily because it presented a provisional restoration which was evicted when attempting to apply second order movements (Figure 12). The amount of gingival recessions did not increase during treatment and periodontal pockets decreased (Figure 10). The amount of alveolar bone and root size did not suffer significant decrease (Figure 13).
In the literature, there are only a couple of reports of orthodontic treatments conducted in elderly patients.
In a report of three cases, Newman established that orthodontic treatment in elderly adults is complex and limited.3 Treatment in the elderly due to physiological and practical reasons typically includes limited orthodontic procedures and establishes the need for an interdisciplinary approach. In terms of physiological reasons, the following may be mentioned: periodontal disease, presence of restorations, dentures, absence of dental organs and physiological changes in the oral cavity that accompany old age. In this case, the patient had almost all of these conditions which resulted in a limited orthodontic treatment.
In a report by Newman,3 two of the cases showed sequelae of periodontal disease, while in the patient reported by Ryan and Hegarty,4 there were not. Pathological migration due to chronic periodontitis involved considerations in treatment. In the periodontally compromised dentitions, the loss of alveolar bone causes that the center of resistance to move apically and the net effect is that teeth are more likely to have a tilt movement instead of a bodily one.5 In the described case, second and third order movements were limited by the biomechanical considerations of the tissues that support.
The combination of intrusion and periodontal treatment has been shown to improve compromised periodontal conditions if oral hygiene is maintained and tissues are healthy.5 Ong and Wang recommend the use of lighter forces (5-15 g per tooth) to reduce the possibility of root resorption and reduce the delay in dental movement due to hyalinization.5 In this case, the patient was first submitted to conventional periodontal therapy and once health was restored, orthodontic treatment was started with light forces that remained the same throughout treatment time.
The evidence obtained by various authors6-8 shows that orthodontic treatment not only improves aesthetics and function but also helps to prevent inflammation and relapse of the periodontal collapse. The effectiveness of orthodontic treatment in patients with periodontal di’ sease is increased by eliminating inflammatory factors, facilitating oral hygiene and altering occlusal factors through dental alignment.9 It has also been reported that gingival tissues or alveolar bone topography can be improved by altering dental inclination or extrusion.10 In this patient, the proclination and extrusion of the upper incisors was significant, as well as the spacing between the upper and lower anterior teeth which made oral hy’ giene difficult, affected her aesthetics and compromised the final prosthetic rehabilitation. At the end of the treatment, all these conditions presented improvement, except bony support due to failures in hygiene control and in periodontal control.
Among the practical reasons that Newman mentions it is important to highlight the economic factor. According to the National Population Council,2 in Mexico, around half of the population of older adults is in a situation of poverty and only a third of them works mostly with a low income. This leads to the situation where many elderly patients cannot afford a multidisciplinary treatment. This was relevant in the case hereby presented.
Posterior occlusion could not be corrected because it required a prosthetic treatment that the patient at that time could not afford.
Treatment time was lengthened as a result of repeated failures in the adhesion of the appliances to the prosthetic restorations and because of consults with rehabilitation dentistry, prosthetics and periodontics.
ConclusionsTreatment of the elder patient requires very close interaction between all areas of responsibility due to the multiple conditions that generally suffer from. Patient cooperation is also a crucial factor for treatment success in the older patient.
For the orthodontist, treatment is challenging and has limitations however it provides the possibility for integral oral rehabilitation and improves the quality of life of elderly patients. In this article a clinical case of an elderly patient who underwent a limited orthodontic treatment and obtained satisfactory results was reported.