Dentofacial anomalies cause disharmony in the maxilla and the mandible with consequences in facial esthetics and masticatory function. As surgeries and osteotomies became more complex the need for cooperation between the orthodontist and the maxillofacial surgeon became more evident. A case report of a 1 year and 8 months treatment time of an 18-year-old patient, with skeletal class III malocclusion, anterior crossbite and posterior unilateral crossbite, upper incisor proclination and lower incisor retroclination, and vertical growth is hereby presented. A treatment plan was set out with surgical-orthodontic treatment which is divided in three phases: First presurgical phase with 0.022×0.028 Roth system and arch sequence, second surgical phase performing a triple surgery: Le Fort I for maxillary advancement, with segmental surgery on the left side and vertical osteotomy of the mandibular ramus for mandible repositioning. A good facial harmony and improvement of the skeletal and dental relationship were obtained but most importantly, neuromuscular regulation improvement and stomatognathic function.
ConclusionThe satisfactory results in combined orthodontic and orthognathic surgery treatments depend on a good diagnosis and treatment plan of the dentofacial deformity, as well as on good knowledge integration between the professionals involved in the case.
Las alteraciones dentomaxilofaciales propician una desarmonía en el maxilar y la mandíbula, distorsionando la estética facial y la función masticatoria. A medida que las intervenciones y osteotomías fueron siendo más complejas se hizo cada vez más evidente la necesidad de la colaboración del ortodoncista con el cirujano maxilofacial. Se presenta en este artículo el diagnóstico y tratamiento durante 1 año 8 meses de un paciente de 18 años con maloclusión esquelética clase III, mordida cruzada anterior y posterior uniteral, proinclinación dental superior y retroinclinación inferior, y crecimiento vertical. Se opta por un tratamiento quirúrgico-ortodóncico, el cual se divide en tres fases: Primera fase prequirúrgica con la colocación de aparatología sistema Roth 0.022×0.028 y secuencia de arcos, segunda fase quirúrgica realizando cirugía triple, Le Fort I maxilar de avance, con cirugía segmentaria del lado izquierdo y osteotomía vertical de las ramas mandibulares para reposición de la mandíbula. Se logró conseguir una buena armonía facial gracias a la mejora de la relación esqueletal y dental. Pero sobre todo se consiguió mejorar la regulación neuromuscular y la función del sistema estomatognático.
ConclusiónLos resultados satisfactorios en tratamientos combinados de ortodoncia y cirugía ortognática dependen de un buen diagnóstico, plan de tratamiento de la deformidad dentofacial y de una buena integración de los conocimientos entre los profesionales implicado en el tratamiento.
Anomalies in position, size and shape of the facial bones, especially the maxillary bones, usually appear in childhood and are known as growth disorders. They continue to grow in severity during adolescence until they become stable at the end of the growth period. Although these anomalies have an important genetic basis, they are usually growth problems. There are functional factors that can have an important influence over them such as thumb sucking or prolonged pacifier use, two habits that cause a bad position of the teeth more than skeletal discrepancies.1 Among these anomalies, prognathism is the most frequent disturbance, followed by the retrognathism, maxillary hypoplasia and mandibular asymmetry. All these alterations are conducive to a disharmony between the maxilla and the mandible, distorting facial aesthetics and affecting masticatory function.2
In this type of patients surgery is no substitute for orthodontics, but treatment must be properly coordinated in order to achieve acceptable overall results. The spectacular advances of recent years have made it possible to combine these treatments to correct many serious problems that were untreatable only a few years ago. Orthognathic surgery is an increasingly common practice due to its aesthetic and functional implications. As interventions and osteotomies became more complex the need for collaboration of the orthodontist with the maxillofacial surgeon became increasingly evident.
Surgical treatment of prognathism started at the beginning of this century. Edward Angle, talking about a patient who had been subjected to this kind of treatment, explained how results could have been improved if orthodontic appliances and occlusal splints had been used.3
Orthognathic surgery, as we know it nowadays, was developed in the mid-twentieth century, primarily by the work of the Germanic school, especially by doctors Trauner and Obwegeser. The initial indication for these procedures was the correction of moderate and severe dentofacial anomalies, with the accomplishment of a proper occlusion being the fundamental objective.4The sagittal ramus osteotomy initiated by doctors Trauner and Obwegeser marked the beginning of a new era for orthognathic surgery.5 In this technique an intraoral approach was used thus eliminating the need to perform a potentially disfiguring skin incision.
Sagittal osteotomies also represented a biologically appropriate method for elongating or shortening the mandible with the same bone cuts, which allowed treatment for mandibular deficiency or excess. During the sixties, Americans surgeons began to use and to modify the techniques developed in Europe for maxillary surgery and after a decade of rapid progress in maxillary surgery the development of the LeFort I horizontal fracture technique was accomplished by Bell,6 Epker and Wolford,7 which allowed maxillary reposition in the three space levels.
In the eighties, advances in oral and maxillo-facial surgery allowed repositioning of one or both jaws, the displacement of the chin in the three planes of space and the surgical relocation of segments according to dentoalveolar needs.7 In the nineties patients’ discomfort decreased considerably thanks to rigid internal fixation which eliminated the immobilization of the maxillae, and a better knowledge of the typical patterns of postsurgical changes thus obtaining more stable and predictable surgical results.
Among the latest developments that have revolutionized orthognathic surgery in Spain, the use of miniplates should be noted with the fact that once the bone is cut, it gets back together with a resorbable material thus replacing the old titanium plates that remained in the tissue.1,8
When a patient is selected to receive surgical orthodontic treatment in order to correct a dentofacial disharmony, it is convenient to know that the patient must comply with certain rules to be able to undergo surgery which are:
- a)
Ideal oral health.
- b)
No dental retentions.
- c)
Arch coordination.
- d)
Dental alignment.
- e)
Respected dental midlines.
- f)
Ideal anterior angulation according to basal bone.
- g)
Flat curve of Spee.
- h)
Occlusal tripodism (presurgical orthodontics 75%).
- i)
Heavy archwires four weeks before surgery.
- j)
Orthodontic fixed appliances suited for orthognathic surgery (no porcelain brackets, archwire ligated with steel ligature, soldered ball hooks).
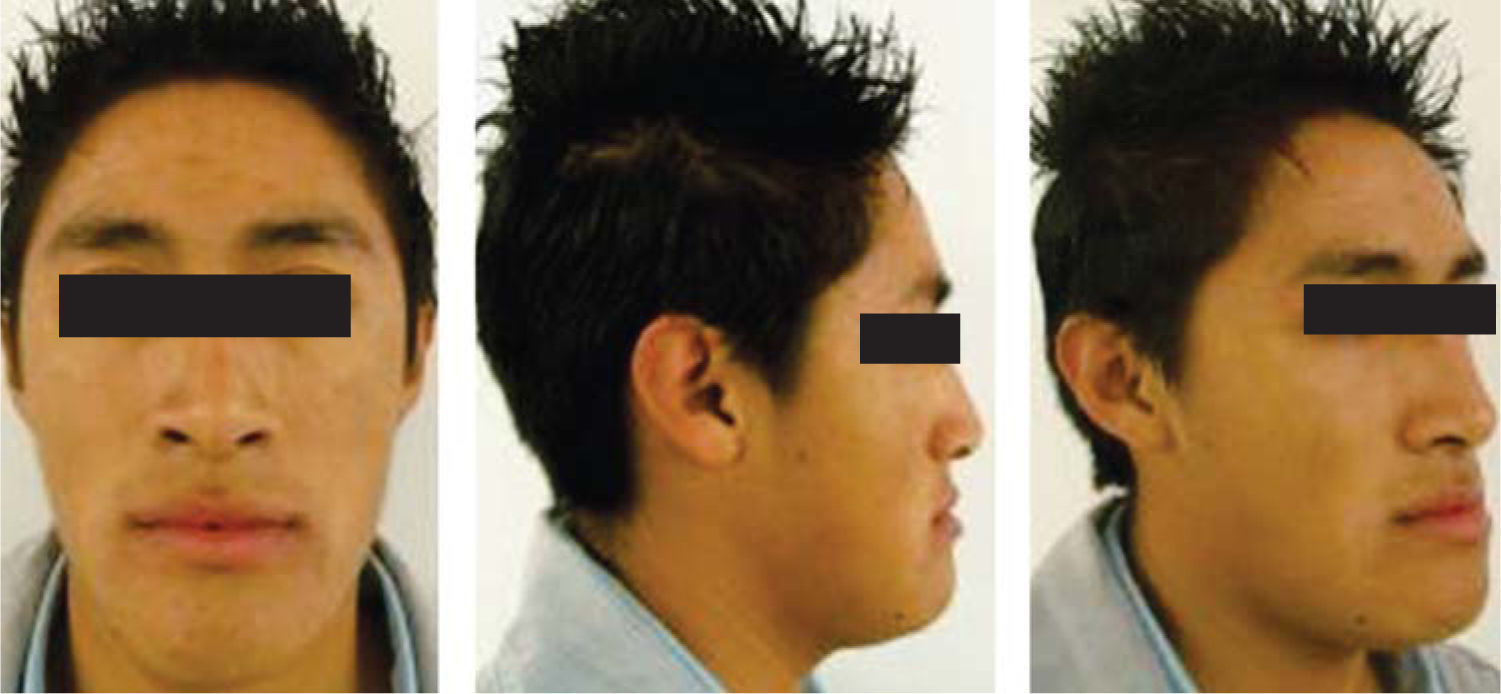
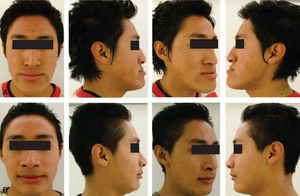
Male patient of 17 years of age, with an important maxillo-mandibular discrepancy caused by prognathism with unilateral left crossbite as well as a left and right concave profile (Figure 1).
Occlusion is completely altered as he presents anterior crossbite, poor anterior guidance, left and right canine Class III and bilateral molar Class III, slight crowding and upper and lower deviated midlines. Cephalometrically, the patient presents a skeletal Class III due to prognathism, proclined axial axis of the anterior teeth and retroclination of the lower teeth, and a vertical growth pattern (Figure 2).
On the basis of clinical, facial, dental, and functional characteristics, it was decided that the procedure of choice to achieve ideal goals was a surgical-orthodontic treatment,10 with use of 0.022×0.028 Roth fixed appliances, with bands in first and second upper and lower molars. The data from cephalometric analysis and from study models show that there is no need for extractions to eliminate crowding.11 The surgical- orthodontic treatment is divided into three phases:
Presurgical first phase: AVTO and pre-surgical tracings were performed. Subsequently, fixed appliances were placed to carry out the initial leveling and alignment, to achieve presurgical consolidation by means of second and third order movements and to express the system prescription having as main objective crowding correction and proper axial inclinations of all the dental organs regardless of their intermaxillary relations.12
The archwire sequence for the Roth system was: 0.014 NiTi, 0.016 NiTi, 0.016×0.022 NiTi, 0.016×0.022 stainless steel, 0.017×0.025 NiTi, 0.017×0.025 stainless steel, Arc 0.019×0.025 NiTi and 0.019×0.025 stainless steel with surgical hooks.
The last achwire was left in place for at least a week in order to take upper and lower impressions which were used in model surgery. Model surgery was performed after the surgical prediction and should be performed with the orthodontist and the maxillofacial surgeon together to reach an effective plan suited for the patient.
Model surgery was performed in accordance to the treatment plan goals. It was confirmed that the results were as desired. Two surgical splints were made, the intermediate and the final, for interventions on both jaws. These were transparent acrylic splints that were used to achieve a correct intermaxillary relationship during the surgical procedure.
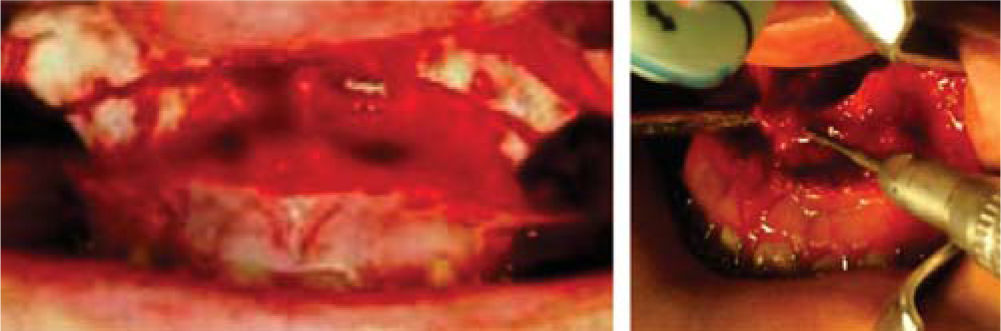
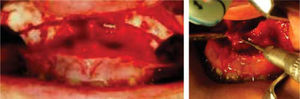
Surgical phaseOn the basis of the previously described analysis the decision was taken to perform a triple surgery: maxillary Le Fort I (Figure 3) with segmental surgery on the left side and vertical ramus osteotomy for mandibular repositioning (Figure 4).
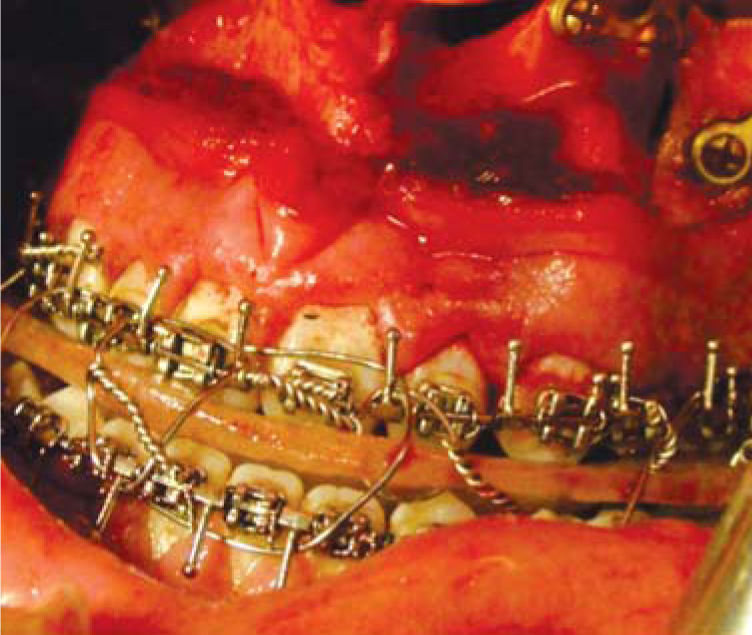
In a conventional bimaxillary surgery, an intermediate splint is required: it is used at half the intervention, to achieve a correct position of the maxilla with respect to the original situation of the mandible (Figure 5) and a final splint to place the mandible in the desired position with respect to the maxilla that has already been modified and fixed with osteosynthesis plates.13,14
Postsurgical second phasePostsurgical follow-up was six weeks in convalescence with intermaxillary splinting due to the type of mandibular surgery. Afterwards, surgical archwires were withdrawn and a re-leveling was performed. To that end, 0.016×0.022 NiTi archwires were placed and the patient was instructed to use M elastics. Subsequently, 0.019×0.025 NiTi upper and lower archewires were placed for three weeks. In the consolidation phase, 0.019×0.025 stainless steel archwires were placed for five weeks to fully express the system's prescription.15,16 Occlusal settlement was done with a 0.019×0.025 braided archwire.
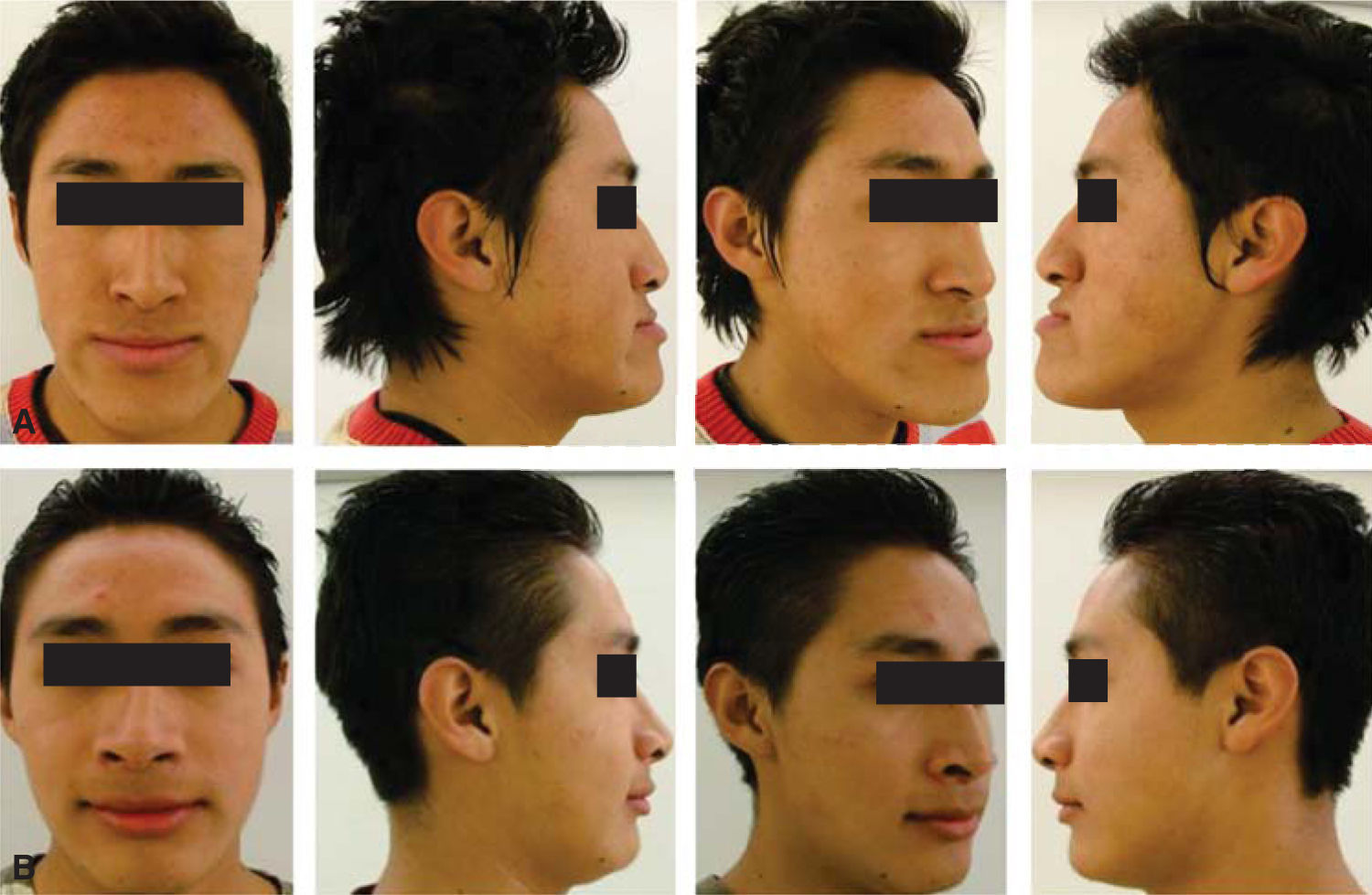
ResultsA good facial harmony was obtained thanks to the improvement of the skeletal and dental relationship. With maxillary advancement the midface depression was corrected and with mandibular retropositioning a decrease of the lower third was accomplished as well as a straight and harmonious profile (Figure 6). But above all we managed to improve the neuromuscular regulation and function of the stomatognathic system.17,18
In the dental aspect, an excellent occlusion was achieved. Left and right molar class l was obtained as well as a bilateral canine class l and a proper overjet and overbite (Figure 7). With segmental maxillary surgery the unilateral crossbite was corrected to a 100% thus achieving a proper posterior occlusion (Figure 8).
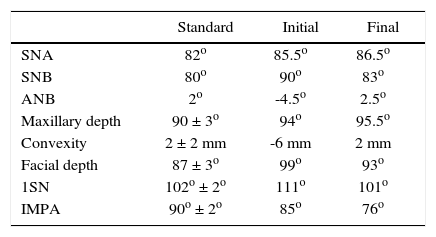
Cephalometric changes. Favorable changes were obtained in a class III. It was possible to reach the cephalometric norm and achieve an adequate positioning of the bony structures (Table I).19,20
DiscussionIn this article it is highlighted the need to assess the patient in a multidisciplinary way as a key factor for diagnosis since treatment is multidisciplinary. All dental specialties are involved with the same force and scientific rigor as well Pereda et al., declared.1
Stout et al.,13,14 reported that early diagnosis would lead to a functional orthopedic therapy-that would guide facial bone growth in a proper manner. Later diagnosis affects the orthodontist's decision-making, and especially the patient's, specifically on whether an orthodontic «camouflage» is to be performed or the correction of skeletal bases to achieve an adequate dental placement. According to the choice of the first or the second option, planned dental movements will be in opposite directions from the start.
There are still many authors that state that it is necessary to wait until body development is complete to perform maxillofacial surgery since it was usually conducted until the age of 14 or 15 years when the greatest vertical growth had stopped. However Wassmund et al demonstrated that the procedure could be performed at 10 to 14 years of age given that in a study conducted in this age group satisfying esthetic results were obtained with stable dental and skeletal occlusion.
Rodriguez and Soto, just like Pereda et al.,1,21 recommend that the decisive age for surgery is determined by the moment in which the patient identifies his or her problem along with the psychic and emotional involvement that he or she refers: when the functional disorder is a limiting factor for chewing or swallowing, when joint and muscular pains appear etc.
As refered by Gregoret and Trujillo,9 it is of the utmost importance to meet 100% of the pre-surgical orthodontic requirements to obtain optimal results during surgery.
In the same way, no surgical technique should be ruled out no matter how old it is because there will always be a patient with such a deformity that must be dealt with by some of these techniques.
ConclusionsSatisfactory results in orthodontic and orthognathic surgery combined treatments depend on a good diagnosis and treatment plan for the dentofacial deformity,as well as a good knowledge integration among the professionals involved in the treatment.
A good coordination between the maxillofacial surgeon and the orthodontist is essential for an optimal result in the treatment of patients who require orthognathic surgery. The maxillofacial surgeon should understand the treatment plan from the orthodontic point of view and the orthodontist should be able to identify the objectives of the pre-surgical orthodontic treatment and know the limitations of orthognathic surgery.