Anterior cross-bites are common in growing patients due to different etiological factors such as: injury to the primary incisors with displacement of the permanent teeth; exfoliation of permanent incisors and palatal deviation because of a collapse in the premaxilla; supernumerary teeth and arch length deficiency.
ObjectivesTo present a case of an anterior crossbite orthopaedic correction.
Case reportAn 11- year- old male patient was referred to the Orthodontics Clinic with an anterior crossbite and dental avulsion of a mesiodens due to trauma. The patient presented a dolichofacial pattern, a skeletal Class I relationship, horizontal mandibular growth, Class I molar relationship and retrusive maxillary and mandibular incisors.
TreatmentFirst phase: Orthopaedics. Second phase: Orthodontics. An appliance similar to the Bite Block with a hyrax expansion screw placed parallel to the mid-palatal suture and a facial mask were constructed.
ResultsThe patient¿s anterior crossbite was corrected. Maxillary parameters were evaluated in relation to the Steiner, Jaraback and Ricketts analysis; SNA angle was increased by 4°, the convexity increased by 3mm and the SNB angle, by 1°. Dental parameters showed that the interincisal angle decreased by 1° whereas SN/1 sup angle was increased by 8°. The patient¿s soft tissues showed a positive change, which favoured the profile.
La mordida cruzada anterior es común en pacientes en crecimiento, dentro de su etiología tenemos: trauma a los incisivos primarios con desplazamiento del brote del diente permanente, exfoliación de los incisivos primarios con la desviación a palatino del incisivo permanente ocasionando el colapso de la premaxila, dientes anteriores supernumerarios y perímetro de arco deficiente.
ObjetivosCorrección de la mordida cruzada anterior e incrementar el perímetro del arco maxilar.
Presentación del casoPaciente masculino de 11 años de edad referido a la clínica de ortodoncia de DEPeI con mordida cruzada anterior y con la avulsión dentaria de un mesiodens por un traumatismo. El diagnóstico fue: leptoprosopo, clase I esquéletica, crecimiento horizontal mandíbular, clase I molar y biretroclinación dental.
Tratamientoprimera fase ortopédica y segunda fase ortodóncica: Se construyó un dispositivo tipo bite-block y tornillo sagital combinado con una máscara facial.
ResultadosLa mordida cruzada anterior fue eliminada. En relación a los análisis de Steiner, Jaraback y Ricketts los parámetros para el análisis esqueletal fueron: ángulo SNA donde se observó un incremento de 4°, en el caso de la convexidad se registró un incremento de 3mm y un aumento de 1° en el caso del ángulo SNB. En relación con los parámetros dentales se obtuvo una disminución de 1° en el ángulo interincisal y un aumento de 8° en el ángulo SN/1 sup. los tejidos blandos se modificaron favoreciendo el perfil.
Anterior cross-bites are one of the most common orthodontic problems in growing patients. Usually, it develops during the primary and mixed dentition as a result of an anomaly in the skeletal, functional or dental components of the stomatognathic system if the child. Among the most common etiologic factors are: incisor interference causing an anterior mandibular displacement, trauma to primary incisors with a palatal displacement of the permanent incisor, supernumerary anterior teeth, odontomas, abnormal eruption paths and insufficient arch perimeter.
When this malocclusion continues uncorrected in the permanent dentition, it reduces treatment options and provides a less favorable environment for an adequate growth.
Anterior cross-biteIt is more commonly observed in a skeletal class III relationship. It is defined by one or more upper anterior teeth occluding on the lingual surface of the lower anterior teeth.1
EtiologyAbnormal eruption of the permanent incisors which causes interferences, supernumerary teeth in the anterior segment, odontomas, congenitally abnormal eruption path, arch perimeter deficiency, upper anterior crowding.2 It is important to determine whether the anterior cross-bite is a functional displacement of the mandible or a skeletal problem.
Cross-bite classification- •
Dental anterior cross-bite:
The most common etiologic factor is lack of space for the permanent incisors; the upper incisors adopt a lingual position in relation to the dental arch line and erupt in cross-bite. It usually involves one or two teeth; the facial profile is straight in centric occlusion and centric relation and there is a class I molar and canine relationship. In the cephalometric analysis, the SNA, SNB and ANB angles are normal.2
- •
Functional anterior crossbite (pseudo-class III):
It is defined as the movement in which the mandible achieves final occlusion by an anterior displacement in a Class III molar relationship in centric occlusion and a molar Class I in centric relation. An edge to edge position can be achieved in centric relation. A straight facial profile may be observed in centric relation and a concave one in MIC. In the cephalometric analysis a normal false ANB angle may be present.1,2
- •
Skeletal anterior cross-bite:
Prognosis is unfavorable. Molar and canine class III relationships, both in centric occlusion as in centric relation; edge to edge relationship is not achieved in centric relation; the profile is concave with upper retrocheilia, prominent chin and decreased lower third. The cephalometric analysis shows a decreased SNA angle, increased SNB and a negative ANB angle. The direction of growth is horizontal.
The soft tissue profile affects the appearance but does not always correspond with the anteroposterior anatomy of the bony structures.
The concave soft tissue profile suggests a class III sagittal intermaxillary relationship and the chin soft tissues are too far forward in relation to the subnasale point.2
Adequate therapeutic strategiesWhen diagnosing a class III malocclusion patient in the permanent dentition treatment options are limited, particularly when there is a skeletal component. The treatment includes orthodontics, extractions and /or orthognathic surgery.
In patients with mixed or deciduous dentition with a class III malocclusion diagnosis the most common treatment is the orthopedic facemask popularized by Delair (1971-1976) and modified by Petit (1982-1983). The facemask produces good results in a short period of time for the majority of Class III patients.
Jean Delaire and P. Verdon developed the facial mask in 1969. Initially intended to compensate for shortcomings in the maxilla consecutive to a cleft palate, it was used afterwards to correct class III's. It was found that the mask was effective for the majority of the patients between 5 and 8 years of age, due to the fact that the device system affects almost all areas that contribute to the class III malocclusion such as skeletal maxillary retrusion, prognathism and lower anterior height decrease. It therefore applies to the majority of developing class III patients independent of the specific etiology.
The initial treatment plan includes a maxillary disjunction device in order to perform a rapid maxillary expansion (RME) combined with maxillary protraction using a Petit face mask, which is placed 10 days after the expansion has commenced. The elastics with which the protraction will be achieved should be directed in a slightly descending horizontal direction. Petit recommends the use of 800g elastics per side or even 1,500g per side, i.e. 3,000g in total. The use of a face mask will be from 3 to 6 months to obtain a 2-5mm overjet and subsequently it is recommended an additional period of 3 to 6 months.
The facial mask produces a postero-anterior skeletal protraction of the maxilla, helps to improve growth in the anterior portion of the maxilla and premaxilla, with a mesial movement of the upper dental arch in relation to the maxillary base. In the mandible it modifies the direction and amount of growth of the condylar cartilage and remodels the chin and lingual inclination of the lower incisors.3
S. Sari et al,4 conducted a study to assess a passive method to correct the anterior crossbite of a single incisor by means of a resin inclined plane. In a sample of 35 children from 7 to 11 years in which it was built an inclined plane of 3-4mm and 45° with respect to the longitudinal axis of the tooth on the incisal edges of the mandibular incisors, verifying that there is a single point of contact between the two arches at the level of the incisors. At the end of a week, 33 cases of crossbite were corrected by this method and the two cases that were not corrected, one had vertical deep overbite and the second had a rotated incisor along with the crossbite. The authors conclude that an inclined plane is a technique for correcting the anterior crossbite single incisor tooth.
In 2004 A. Osman Bengi et al,5 used a bite blocktype device with a hyrax -type screw placed parallel to the median palatal suture and welded to the bands of the first molars to carry out a successful distraction osteogenesis in the premaxilla as an alternative treatment in adult patients with hypoplastic maxilla and retrognathic mandible in a 18.2 year-old female patient with a skeletal class III with hypoplasia of the premaxilla and retrognathic mandible; the device was cemented in the mouth after surgical procedures (maxillary segmental osteotomy), the patient was observed during the latency period (seven days) after which the 0.5mm screw was activated every 12hours thus eliminating the crossbite in a week.
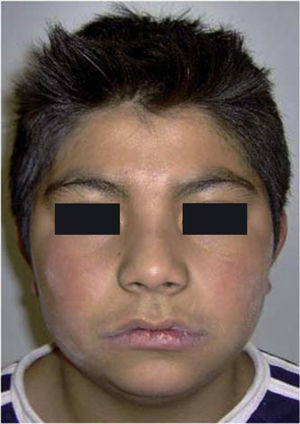
CASE PRESENTATIONMedical historyMale patient of 11 years of age referred to the clinic of the DEPeI with anterior crossbite and convex profile. According to his medical history, he suffered a tooth avulsion of a mesiodents by trauma; no pathological background information was reported. His parents and brothers do not exhibit Class III features. His mother is concerned about appearance.
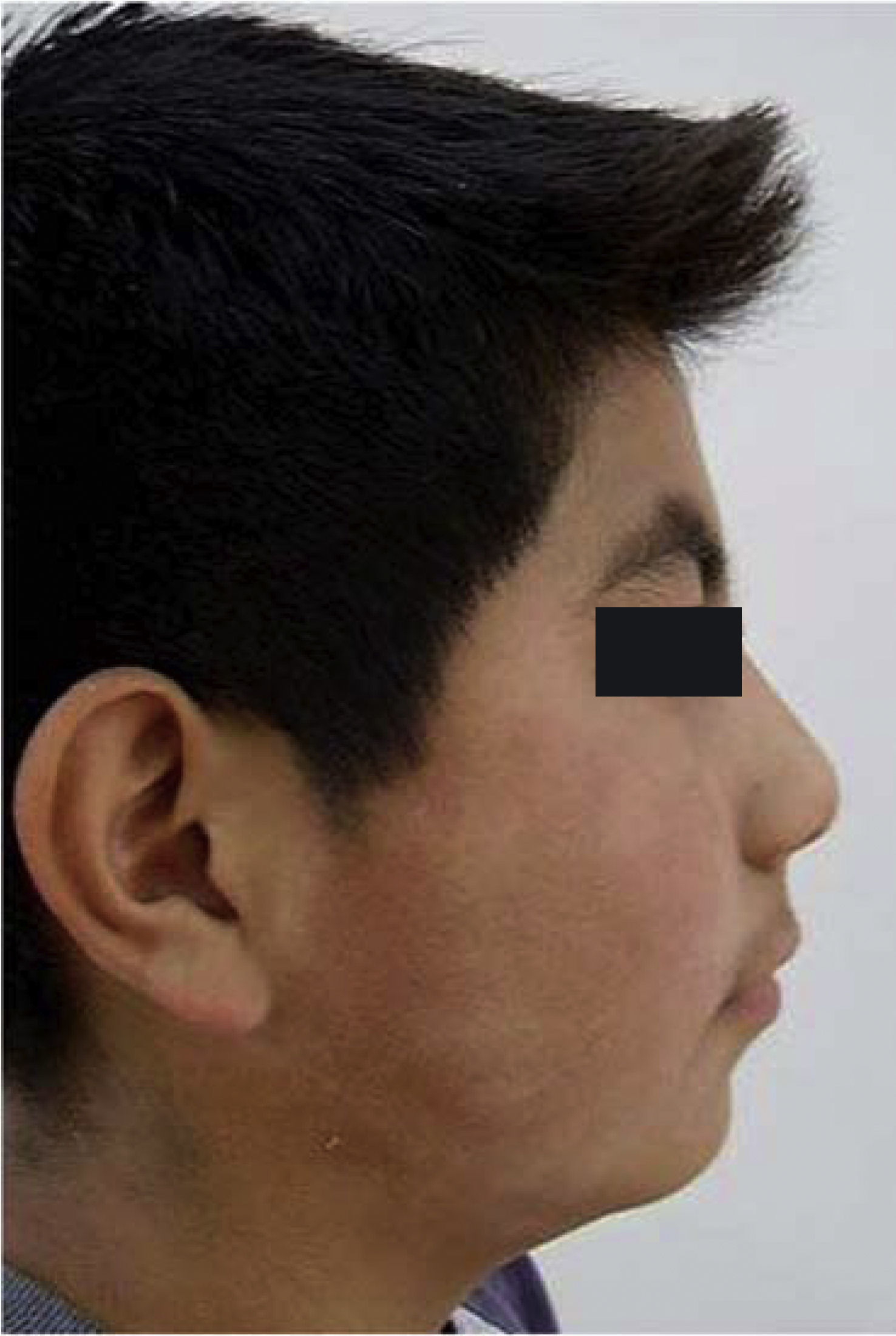
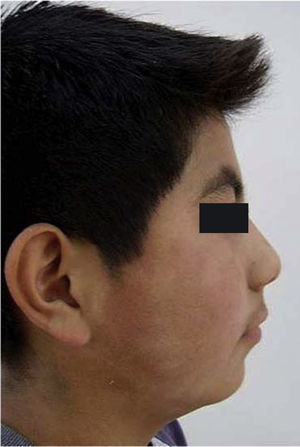
Facial analysis. The patient presented a leptoprosopic pattern with facial asymmetry and deep nasolabial and subnasal folds due to the depression of the upper portion of the lower third. The profile was convex with a non-prominent chin, curled upper lip, and protruded lower lip in relation to the aesthetic line.
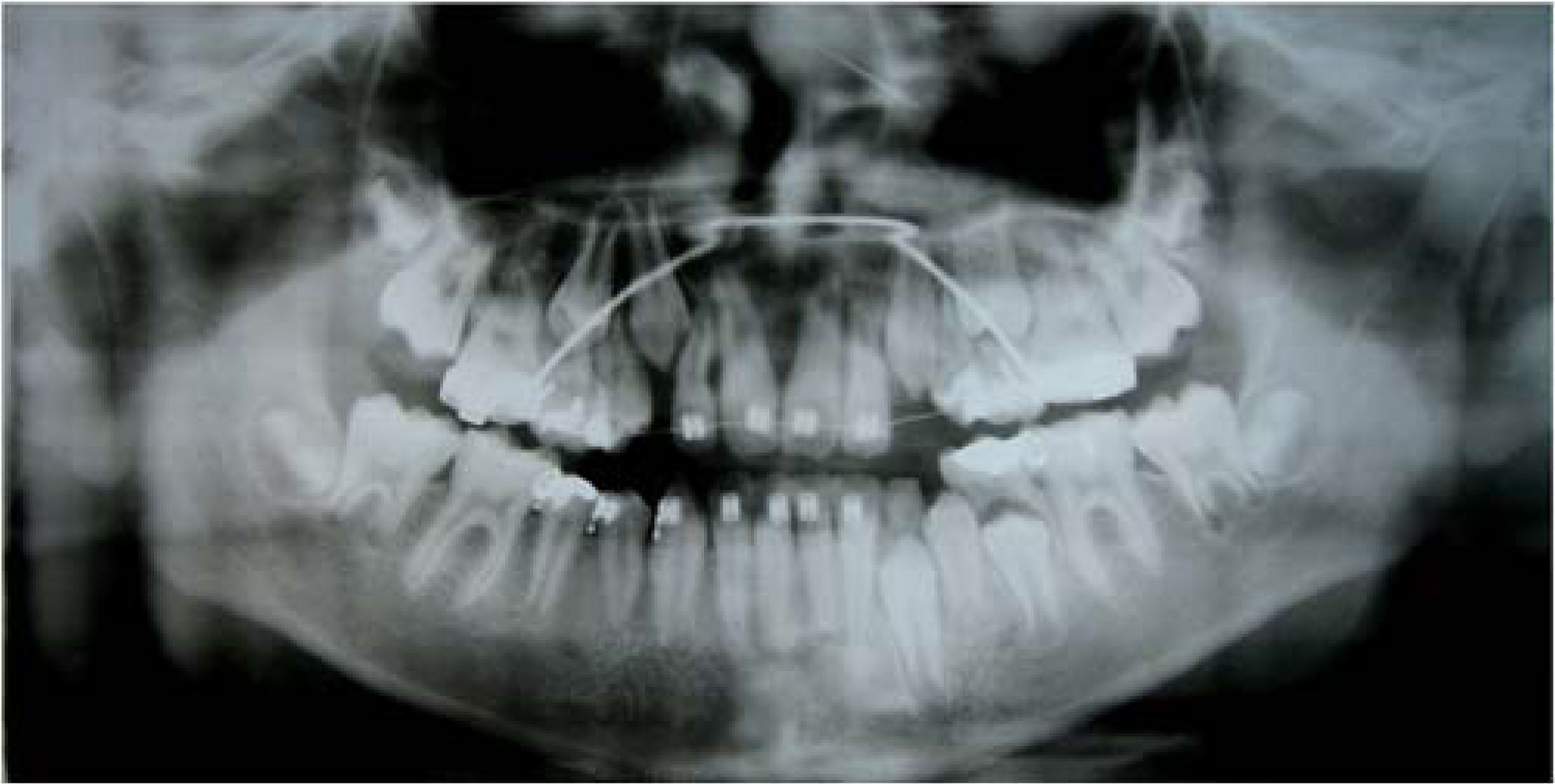
Intraoral analysis. The lower dental midline was deviated to the left. An anterior crossbite was noted and in centric relation the incisor contact did not reach edge to edge. In centric occlusion a -2mm overjet was observed with a Class I molar relationship. The patient was in a mixed dentition and had caries in the dental organs #53, 55, 24, 65, 74 and 75 and an amalgam in #45.
Radiological analysisIn the panoramic and periapical radiographs the skeletal and alveolar structures appeared to be normal with the exception of the apices of the central incisors and the upper right lateral incisor which were not well defined.
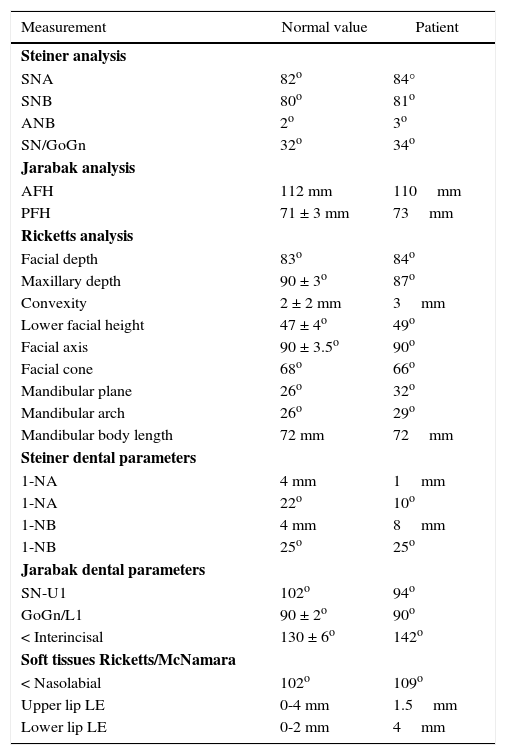
A cephalogram was obtained in centric occlusion and the cephalometric analysis of Steiner, Jarabak and Ricketts were performed (Table I).
Cephalometric data before orthopedic treatment.
| Measurement | Normal value | Patient |
|---|---|---|
| Steiner analysis | ||
| SNA | 82o | 84° |
| SNB | 80o | 81o |
| ANB | 2o | 3o |
| SN/GoGn | 32o | 34o |
| Jarabak analysis | ||
| AFH | 112 mm | 110mm |
| PFH | 71 ± 3 mm | 73mm |
| Ricketts analysis | ||
| Facial depth | 83o | 84o |
| Maxillary depth | 90 ± 3o | 87o |
| Convexity | 2 ± 2 mm | 3mm |
| Lower facial height | 47 ± 4o | 49o |
| Facial axis | 90 ± 3.5o | 90o |
| Facial cone | 68o | 66o |
| Mandibular plane | 26o | 32o |
| Mandibular arch | 26o | 29o |
| Mandibular body length | 72 mm | 72mm |
| Steiner dental parameters | ||
| 1-NA | 4 mm | 1mm |
| 1-NA | 22o | 10o |
| 1-NB | 4 mm | 8mm |
| 1-NB | 25o | 25o |
| Jarabak dental parameters | ||
| SN-U1 | 102o | 94o |
| GoGn/L1 | 90 ± 2o | 90o |
| < Interincisal | 130 ± 6o | 142o |
| Soft tissues Ricketts/McNamara | ||
| < Nasolabial | 102o | 109o |
| Upper lip LE | 0-4 mm | 1.5mm |
| Lower lip LE | 0-2 mm | 4mm |
According to Steiner analysis, the 84° SNA, 81° SNB and 3° ANB angles suggested a biprotrusive skeletal class I; the 34° mandibular plane angle showed a slight mandibular vertical growth. In relation to Jarabak analysis, the anterior facial height (AFH) was normal (110mm) and a 73mm posterior facial height also showed a posterior mandibular vertical growth. With regard to Ricketts analysis, the Facial Depth was 84° and the Maxillary Depth, 87°, both within normal values. The Convexity was 3mm which suggested a biprotrusive skeletal Class I, the Facial Height was 49°, Facial Cone, 66°; Mandibular Plane Angle, 32°, Mandibular Arch, 29° and the Facial Axis 90°, all suggesting a slightly vertical mandibular growth. In all three analysis the maxillary incisors were retrusive and retroclined whereas the mandibular incisors were in a normal position in relation to their basal bone: Steiner analysis: 10° 1NA angle, 1mm 1NA distance, 25° 1NB angle, 8mm 1NB distance. Jarabak Analysis: 94° SN/U1angle, 90° Go/Gn/L1angle, 142° interincisal angle.
The upper lip was retruded in relation with the aesthetic line and the lower lip was in a protrusive position. The nasolabial angle was increased as a result of the poor lip support of the upper central incisors (Figures 1 to 5).
Biprotrusive skeletal class I, vertical growth of the maxilla.
DentalClass I molar relationship, retroclined upper incisors, normally inclined lower incisors, mixed dentition, anterior crossbite, upper and lower squared archform, -2mm overjet and 3.5mm overbite.
FacialLeptoprosopic, facial asymmetry, deep nasolabial and subnasal folds, depression of the upper portion of the lower third, convex profile poor anterior chin projection, retruded upper lip and protrusive lower lip.
TREATMENT GOALSThe significant problems were the premaxilla collapse, the negative overjet and the absence of an acceptable profile.
Thus the goals of treatment were the following:
- •
Correction of the anterior crossbite.
- •
Acceptable profile.
- •
To increase the perimeter of the maxillary arch.
- •
To decrease the nasolabial angle.
- •
To eliminate the maxillary depression that caused the deep nasolabial and subnasal folds.
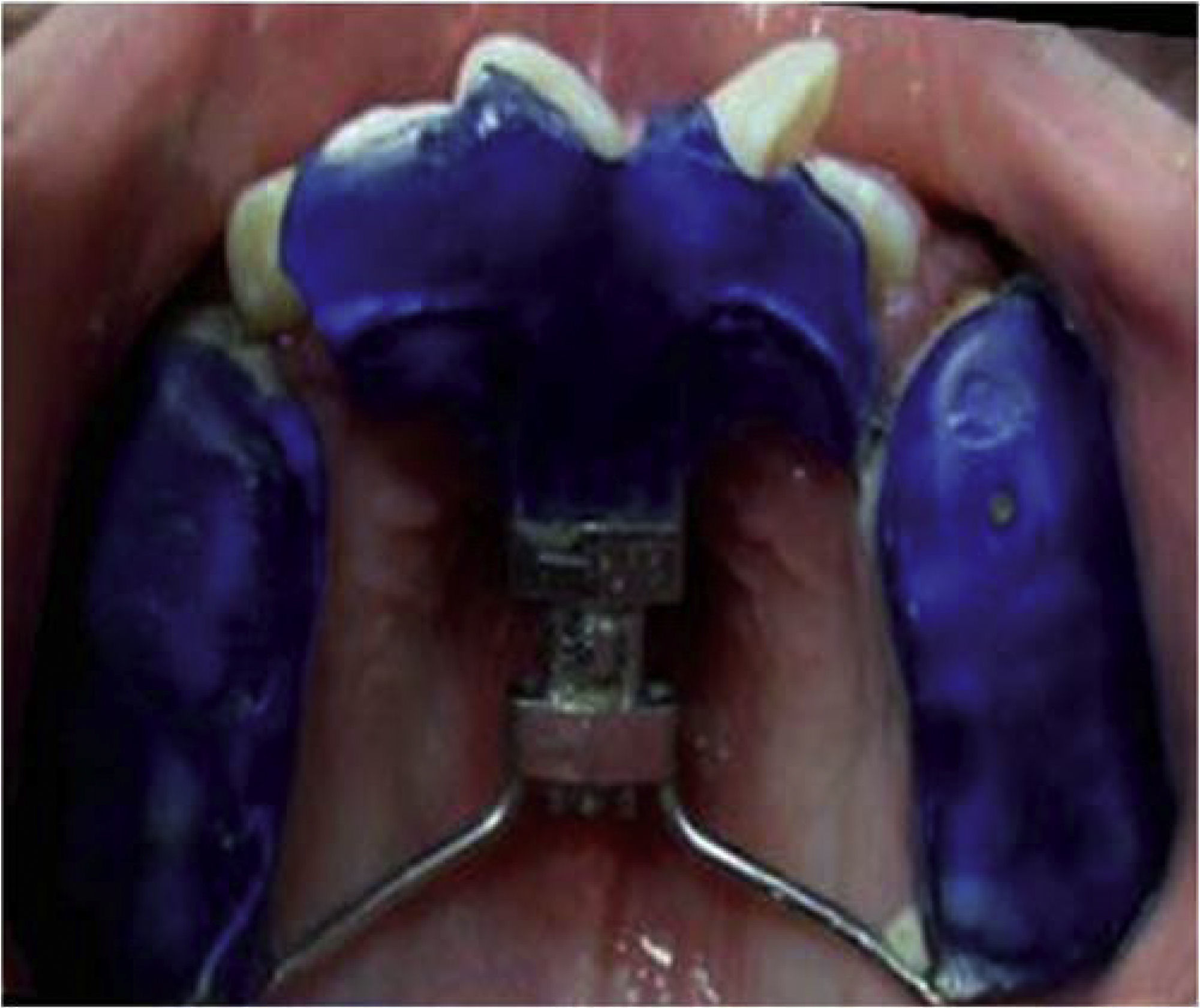
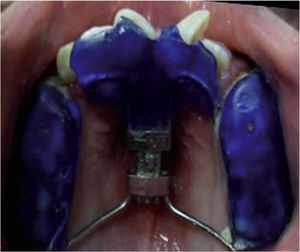
A bite block-type device was built with an expansion screw placed in a sagittal position and it was combined with a face mask with vertical rod in order to prevent the distalization of the posterior segment (Figures 6 and 7).6
TREATMENT PROGRESSThe thermo-curable acrylic device with the expansion screw was placed in a sagittal position involving the posterior teeth with an extension of the anterior screw supported in the premaxilla and the cingulum of the anterior teeth. It was designed to exercise an anterior movement of 3.8mm. The reatment plan was explained to the patient and his guardian and obtained the approval of both.
Construction of the thermo-curable acrylic device with a expansion screwModels were obtained with alginate, the hyrax-type expansion screw was placed parallel to the palatal suture and the anterior extension of the screw was located in the premaxilla and cingulum of the upper anterior teeth. The crowns of the posterior maxillary teeth were covered with high-gloss-polished thermocured acrylic.
ACTIVATION PROTOCOLThe patient was monitored for four months and instructions were given to him to activate the device 0.25mm every third day for 46 days in order to obtain 3.83mm and use the vertical rod facemask 14hours a day to avoid distalization of the posterior segment of the maxilla (¼” elastics on each side, 16 ounces, 453.5g).
The retention period was three months after which the device was removed.
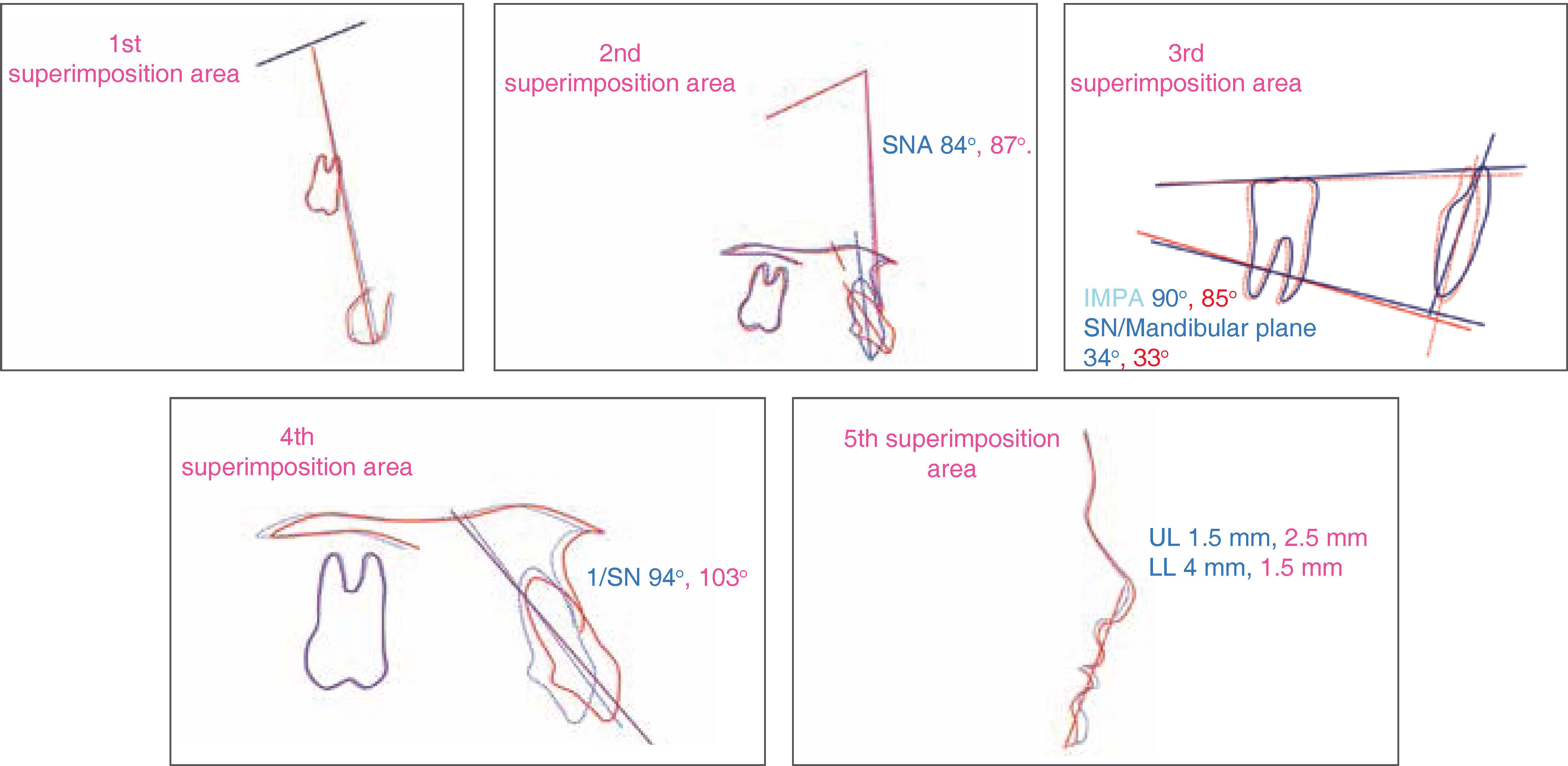
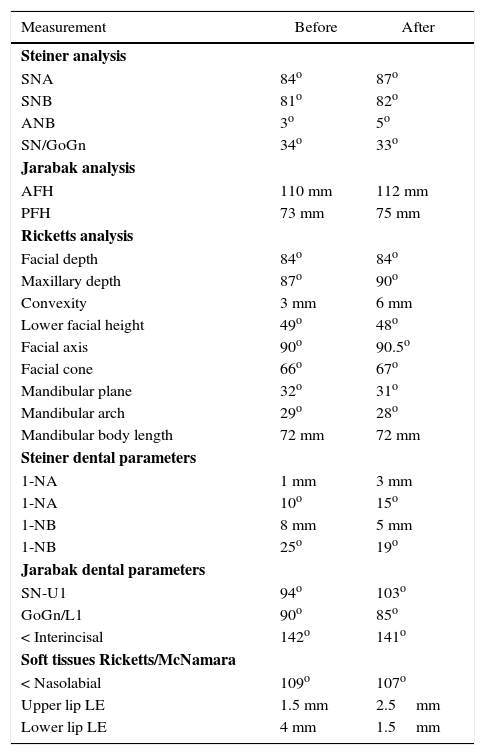
TREATMENT RESULTSThe patient's anterior cross bite was corrected and the lateral headfilms and cephalometric tracings of Steiner, and Ricketts Jarabak were obtained at the end of the orthopedic phase.
Skeletal parametersIn the Steiner analysis it was observed that the SNA angle was 84° pre-treatment and 87° post-treatment, a 3° increase by modifying point A. The SNB angle was 81° before treatment and 82° post-treatment, a 1° increase that suggests a slight counter-clockwise (CCW) mandibular rotation. The ANB angle was 3° pre-treatment and 5° post-treatment: an increase of 2°. The SN/GoGn angle was 34° before treatment and 33° after treatment thus decreasing 1°. According to Jarabak analysis the initial value for the anterior facial height (AFH) was 110mm and the final value, 112mm thus increasing 2mm. The posterior facial height (AFP) was 73mm before treatment and 75mm at the end, increasing its value 2mm.
With regard to Ricketts analysis, the facial depth was 84° pre-treatment and 84.5° post-treatment with an increase of 0.5° which confirms the mandibular rotation. The initial maxillary depth was 87° and the final value was 90° (a 3° increase); the initial convexity value was 3mm and the final, 6mm (a 3mm increase); the lower facial height was 49° pretreatment and 48° post-treatment, decreasing 1° which affected the lower third soft tissues; the initial facial axis value was 90° and the final, 90.5°: an increase of 0.5°. The facial cone was 66° before treatment and 67° after, with an increase of 1°; the mandibular plane was 32° pre-treatment and 31° post-treatment later with a decrease of 1°, the mandibular arch value was 29° before treatment and 28° at the end, decreasing 1°. The mandibular body length was 72mm pre-treatment and 72mm at the end of treatment, remaining without a difference.
Dental parametersAccording to Steiner analysis, the 1aNA angle was 10° pre-treatment and 15° post-treatment, a 5° proclination; the initial 1aNa distance was 1mm and final, 3mm showing a 2mm protrusion. The 1NB angle was 25° before treatment and 19° after treatment which suggests a 6° retroclination; the 1NB distance was 8mm before treatment and 5mm after treatment, with a 3mm decrease in the incisor angulation.
In Jarabak analysis the SN/U1angle was 94° pretreatment and 103° post-treatment thus increasing the proinclination by 9°; the GoGn/ L1angle was 90° before treatment and 85° after treatment, a 5° decrease and regarding the interincisal angle, it was 142° before treatment and 141° at the end of treatment, a decrease of 1°.
Facial parametersWith regard to the soft tissues, in relation to the aesthetic line (LE) the upper lip was 1.5mm pre-treatment and 2.5mm post-treatment, a 1mm increase. Lip protrusion corrected the depression in the area: the lower lip was 4mm before treatment and 1.5mm after treatment decreasing by 2.5mm thus favoring the profile. The nasolabial angle was 109° pre-treatment and 107° post-treatment with a decrease of 2°. The lower third (Sn-Me) maintained a 1:2 ratio, the subnasale-upper stomion value was 23mm before treatment and 24mm after treatment and the lower stomion-menton value was 47mm pre-treatment and 48mm post-treatment, a 1mm increase.
The overjet was -2mm before treatment and 2mm at the end; increasing by 4mm and the vertical overbite value was 2mm.
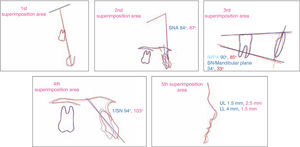
The cephalometric superimposition illustrates the patient's changes (Figures 8 to 13andTable II).
Cephalometric data before and after orthopedic treatment.
| Measurement | Before | After |
|---|---|---|
| Steiner analysis | ||
| SNA | 84o | 87o |
| SNB | 81o | 82o |
| ANB | 3o | 5o |
| SN/GoGn | 34o | 33o |
| Jarabak analysis | ||
| AFH | 110 mm | 112 mm |
| PFH | 73 mm | 75 mm |
| Ricketts analysis | ||
| Facial depth | 84o | 84o |
| Maxillary depth | 87o | 90o |
| Convexity | 3 mm | 6 mm |
| Lower facial height | 49o | 48o |
| Facial axis | 90o | 90.5o |
| Facial cone | 66o | 67o |
| Mandibular plane | 32o | 31o |
| Mandibular arch | 29o | 28o |
| Mandibular body length | 72 mm | 72 mm |
| Steiner dental parameters | ||
| 1-NA | 1 mm | 3 mm |
| 1-NA | 10o | 15o |
| 1-NB | 8 mm | 5 mm |
| 1-NB | 25o | 19o |
| Jarabak dental parameters | ||
| SN-U1 | 94o | 103o |
| GoGn/L1 | 90o | 85o |
| < Interincisal | 142o | 141o |
| Soft tissues Ricketts/McNamara | ||
| < Nasolabial | 109o | 107o |
| Upper lip LE | 1.5 mm | 2.5mm |
| Lower lip LE | 4 mm | 1.5mm |
At present, the use of dentofacial orthopaedics, orthodontics and orthognathic surgery provides treatment alternatives in the different stages of growth and development, but what is most important is the treatment of the malocclusion in its early stages.
In studies related to the anterior crossbite correction by means of fixed mandibular devices S. Sari et al4 used a resin inclined plane placed on the incisal edges of the mandibular incisors for anterior crossbite correction in 35 children aged 7 to 11 years; they observed that satisfactory results were obtained without using a face mask.
The bite-block type device was designed in 2004 by A. Osman Bengi5,6 to obtain a successful maxillary distraction using an osteotomy which included the pyriform apertures bilaterally and the anterior nasal spine (ANS) was advanced with the anterior segment. A 15° intrusion movement was planned to modify the upper lip and tip of the nose thus improving the nasal profile. The A. Osman Bengi device has not been reported for orthopedic treatments, in our case report, the facemask was used as a means of anchorage to avoid distalization of the posterior teeth thus obtaining a better premaxilla shape, a CCW rotation of the mandible and a lingual inclination of the lower incisors.
CONCLUSIONSCephalometric analyses are auxiliaries that have to be considered along with the patient's facies and not so pointedly during diagnostic and post-treatment evaluations.
Orthopedic appliances in growing patients are useful and easy to use; orthopedic anterior crossbite correction will be successful in the case that factors such as the growth stage, remnant and direction (controlled by the clinician) and patient cooperation are favorable.
Significant changes were achieved with the Bite Block-type device combined with a facial mask to correct the anterior crossbite and control the lower vertical height. These results will simplify future orthodontic treatment and avoid possible extractions.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia