Epidermolysis bullosa is a genetic syndrome that consists in the formation of blisters on the skin and oral epithelium in response to mechanical trauma. Epidermolysis bullosa is classified into three major categories, including epidermolysis bullosa simplex, junctional epidermolysis bullosa, and dystrophic epidermolysis bullosa. The dental treatment of patients with epidermolysis bullosa represents a challenge due to the difficulty of operative techniques and the risk of causing blisters in the oral mucosa and also because of the microstomia that results from the cicatrization of injuries in oral epithelium. The pediatric dentist should treat the patient with an integral approach not only by means of restauration or mutilatory treatments, but including an individual risk analysis and prediction for the long term to guide the patient to an excellent status of oral health.
La epidermólisis bullosa es un síndrome genético dermatológico que se caracteriza por la formación de lesiones ampollosas en la piel y mucosas, la cual puede ser de distintos tipos de acuerdo con el estrato de la epidermis que se encuentre afectado, generando sintomatología diversa. Ésta es una entidad de sumo interés para el área estomatológica, debido a las manifestaciones orales que puede presentar y a la dificultad para su tratamiento. El manejo integral estomatológico de los pacientes con epidermólisis bullosa representa un reto, debido a la dificultad de las técnicas operatorias por el riesgo de lesiones en la mucosa oral, por la microstomía secundaria a la cicatrización de las lesiones ampollosas, por la maloclusión dental frecuente en estos pacientes y por la higiene deficiente que condiciona los procesos cariosos extensos. El estomatólogo pediatra debe realizar un tratamiento integral y transdisciplinario, no sólo restaurador o mutilatorio, con un análisis individual de riesgo y una predicción a futuro para guiar al paciente a un óptimo estado de salud bucal.
Epydermolysis bullosa is a genodermatosis which refers to a group of hereditary diseases that affects the stratified tissues such as skin and mucosa and includes the formation of blisters and vesicles after minimum trauma, exposure to high temperatures or in a spontaneous manner with variable affection of different organs.1 The structural defect relies on anomalies on the proteins that form the dermo-epidermic union. It is associated with defects in type VII collagen which may be absent or diminished causing alterations in the anchoring fibrils,2 keratin 5 and 14 defects affecting the basal membrane cell structures; laminin defects, hemidesmosomal structural protein.3There is no specific treatment available and it has a chronic evolution causing gradual movement limitation with an impact over the patient´s life quality. This calls for a case management by means of different specialists with a multidisciplinary approach as well as with the cooperation of the patient´s family.1,3,4
There are approximately 25 subtypes of EB with variations in their clinical and histological characteristics and in their type of heredity. Depending on the histological degree of severity, four groups can be identified according to these subtypes:
- •
Epidermolytic or simple EB (SEB), the defect is intraepidermic where the union between keratinocytes and the basal membrane.
- •
Junctional epidermolysis bullosa (JEB), the union defect is located on the lamina lucida of the basal membrane.
- •
Dermolytic or distrophyc EB (DEB), the affection is located at the level of the anchoring fibrils from the basal lamina to the dermis.1,5,6
- •
Kindler syndrome, which consists in a mixed type of EB with poikiloderma (pigmentation anomalies in the area of the lesion).3
In the subtype classification, besides the degree of histological damage, type of heredity is also considered whether it is dominant or recessive.3
General characteristicsThere is a wide spectrum of cutaneous characteristics present in patients with EB and they can vary from blisters, long and confluent ulcers, extensive cicatrization, pigmentation anomalies, movement limitation, alopecia, fusion of limb folds and onychodystrophy. There are also disorders in non-cutaneous structures such as conjunctiva, gastric mucosas or the muscular skeletal system. In some cases there is a systemic affection such as anemia which in patients with EB it is multifactorial, associated with diet limitations, poor nutrient absorption due to cicatrization in the gastrointestinal tube as well as chronic iron loss because of bleeding in the gastric mucosa. Aditionally, some subtypes of EB are related with growth delay and low height associated with malnutrition and the formation of scarring tissues. In patients with recessive distrophyc EB (RDEB) cutaneous or mucous lesions may evolve into an epidermoid carcinoma, a frequent cause of mortality with a 7.5% risk at age 20 and 67.8% at age 35.7–9
EB oral featuresBlisters in the oral cavityLocalized blisters in the oral cavity are the most common characteristic in every type of EB. However findings in different subtypes vary in degree of severity from small vesicles that heal easily to extensive, confluent lesions that cause gradual or abnormal healing with oral deformity. According to the National Register of Epidermolysis Bullosa (USA) 35% of the localized forms of EBS and 59% of the general forms of EBS present less than 1cm long blisters and heal with no scarring.1,10,17–19 In dominant JEB and DEB lesions in the oral cavity are longer, more than 1cm but heal adequately without causing severe retraction of the tissue or gradual healing.19The blisters present in REB patients are the ones associated with more severe complications in the oral cavity due to their extension and confluence. During cicatrization they cause long bridles that occlude the buccal vestibule and cause severe ankiloglossia and microstomia.
Microstomia and ankiloglossiaMicrostomia is a decrease in mouth opening due to the formation of cicatricial bridles in the mucosa and in the skin of the labial region and to the occlusion of the buccal vestibule. Microstomia appears in the DREB more frequently. Herlitz microstomia in the DREB type also occurs frequently, however in this type of EB the vestibule obliteration or the ankiloglossia are not present and the miscrostomia is due to the formation of extensive perioral lesions.11–14
As part of the comprehensive treatment of microstomia, primarily prevention must be performed, which consists in keeping the trauma to the oral mucosa and the perioral tissues to the minimum. Oral opening exercises are indicated to stimulate the muscles and limit the scar retraction thus improving mouth opening. These exercises can be performed on a voluntary basis and without attachments, only moving the mandible to maximum opening. Auxiliary attachments such as plastic or rubber cones can also be used. These are introduced in the oral cavity causing a forced opening, only using as support the incisal edges of the anterior dental organs.1,14,15 In cases where the EB patient already presents microstomia, restorative dental treatments will be complicated from the technical point of view, however they must be performed.16
Dental anomaliesEnamel hypoplasia has been frequently associated to EBU. Several studies have reported the existence of structural alterations using scanning electron microscopy. (M) Wright described the discovery of enamel hypoplasia in patients with EBD, although it is not as constant as in EBU. Wright also described taurodontism while reviewing X-rays from patients with EBD.1,17–19
Anomalies in craniofacial growth and developmentPatients with generalized EB present an overall delay in growth without the literature being able to elucidate the precise cause of this. It has been associated with chronic malnutrition caused by alterations in the gastric mucosa as well as by limitations in the diet and inadequate nutrient intake. Another factor that has been considered as predisposing to general growth delay is the formation of scarson a large scale in the skin which distort and restrict growth in friction areas, limbs and joints. Growth delay was more severe in patients with EBD and EBU. Patients with EBS have little affection and typically grow without any important sequelae.17–20
Due to the formation of intraoral cicatrization bridles, patients with EBD frequently present a collapsed maxilla, severe dental crowding and lack of space. Scarring tissue on the cheeks, vestibular obliteration, ankiloglossia, and microstomia cause alteration of muscle function with the subsequent alteration of craniofacial growth, as well as the abnormal development of the dental arches.
CariesDental caries has been described as a clinical feature related to EB, however the presence of carious lesions is multifactorial and is associated with individual risk factors that are not exclusive of the disease as well as factors associated directly to the EB. Patients with EB have predisposing risk of caries due to a reduction of salivary flow and alterations in the IgA present in the gingival sulcus.1,8,21,22,23
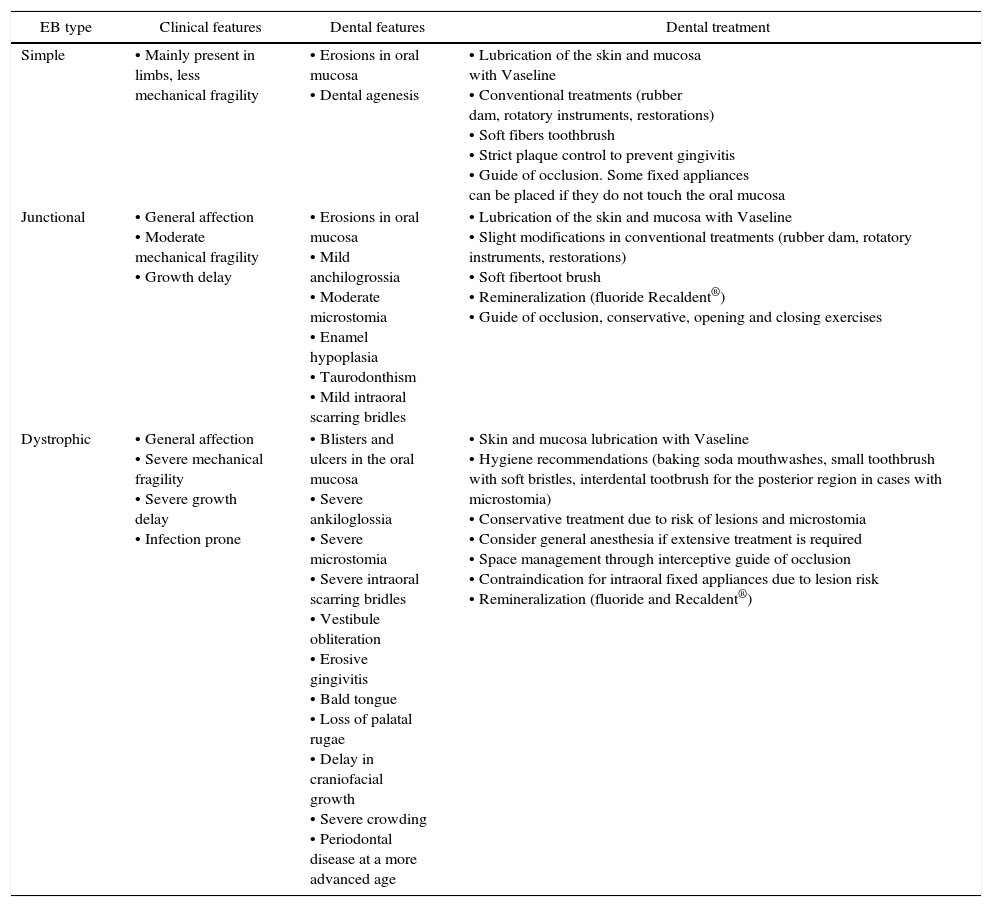
Dental treatment should be based on a thorough diagnosis and an individualized treatment plan with a comprehensive and preventive approach. The individual analysis of caries risk can be performed using validated indexes such as the CAMBRA (caries management by risk assessment).24 There are general measures that the dentist should consider when treating patients with EB, they are mentioned in table I.
Dental treatment in the patient with EB.
| EB type | Clinical features | Dental features | Dental treatment |
|---|---|---|---|
| Simple | • Mainly present in limbs, less mechanical fragility | • Erosions in oral mucosa • Dental agenesis | • Lubrication of the skin and mucosa with Vaseline • Conventional treatments (rubber dam, rotatory instruments, restorations) • Soft fibers toothbrush • Strict plaque control to prevent gingivitis • Guide of occlusion. Some fixed appliances can be placed if they do not touch the oral mucosa |
| Junctional | • General affection • Moderate mechanical fragility • Growth delay | • Erosions in oral mucosa • Mild anchilogrossia • Moderate microstomia • Enamel hypoplasia • Taurodonthism • Mild intraoral scarring bridles | • Lubrication of the skin and mucosa with Vaseline • Slight modifications in conventional treatments (rubber dam, rotatory instruments, restorations) • Soft fibertoot brush • Remineralization (fluoride Recaldent®) • Guide of occlusion, conservative, opening and closing exercises |
| Dystrophic | • General affection • Severe mechanical fragility • Severe growth delay • Infection prone | • Blisters and ulcers in the oral mucosa • Severe ankiloglossia • Severe microstomia • Severe intraoral scarring bridles • Vestibule obliteration • Erosive gingivitis • Bald tongue • Loss of palatal rugae • Delay in craniofacial growth • Severe crowding • Periodontal disease at a more advanced age | • Skin and mucosa lubrication with Vaseline • Hygiene recommendations (baking soda mouthwashes, small toothbrush with soft bristles, interdental tootbrush for the posterior region in cases with microstomia) • Conservative treatment due to risk of lesions and microstomia • Consider general anesthesia if extensive treatment is required • Space management through interceptive guide of occlusion • Contraindication for intraoral fixed appliances due to lesion risk • Remineralization (fluoride and Recaldent®) |
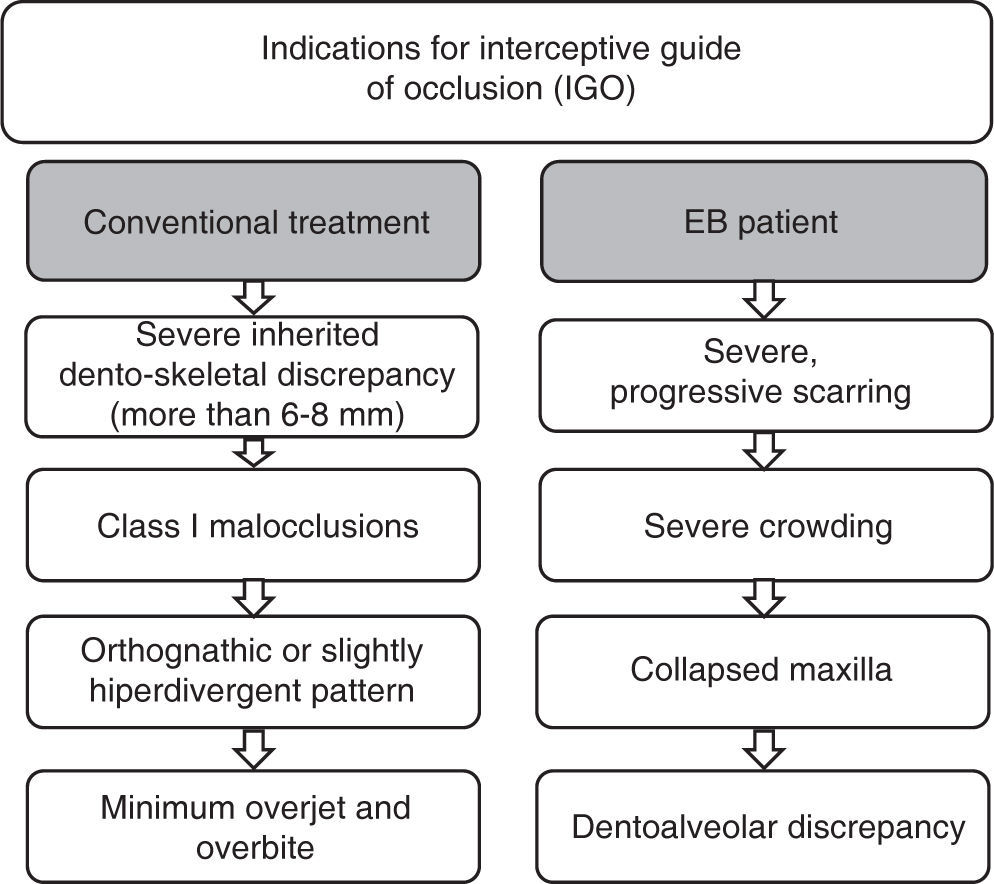
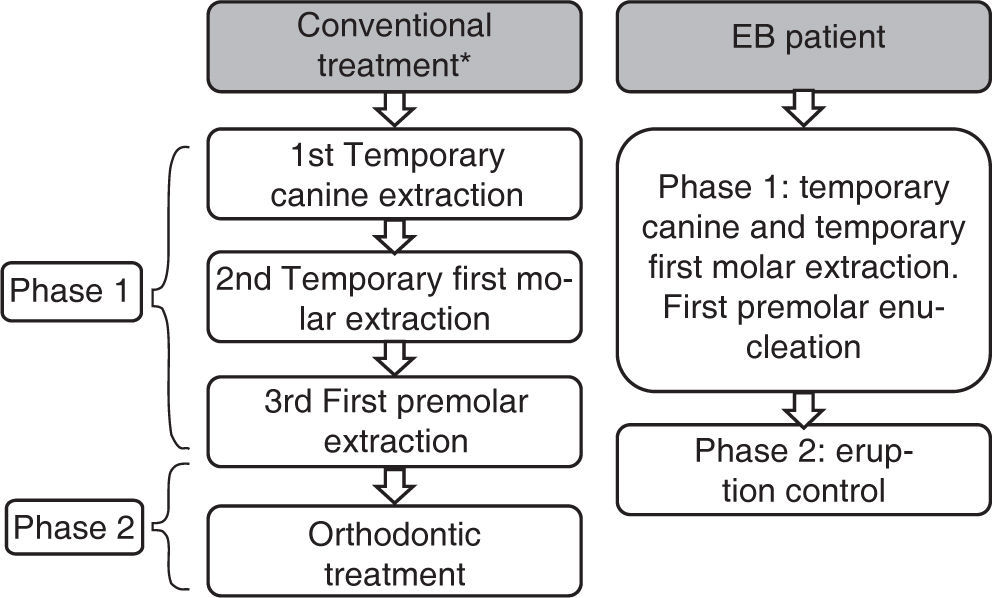
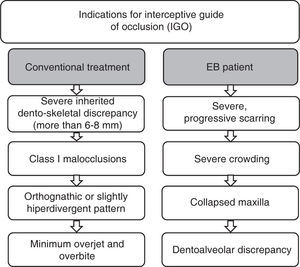
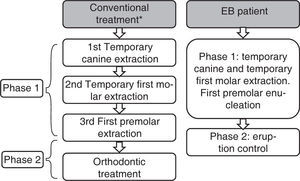
In 1930 Birger Kjellgren coined the term «serial extraction» to define the treatment through extractions when there was lack of space. Rudolf Holz in the same year proposed the term «Guide of dental eruption through removal» which describes more adequately the beginning of the treatment. According to Jack Dale extractions act as a guide for occlusion and are a valid method of treatment, which must be performed under a careful analysis of the case, that provides multiple benefits. The indications for consider the extractions are shown in figure 1.
There is not a precise sequence of extraction, as it varies according to the individual goal of treatment. However there is a frequent sequence that adapts to the majority of the treatments, which consists in the extraction of the temporary canine when the unerupted teeth have less than half of root formation.
Afterwards, the removal of the temporary first molar is performed when the first premolar root is more than a half formed. Finally, we extract the first premolar upon eruption. In a second phase orthodontic treatment should be conducted. In patients with EBD the intervention should be made when the lateral incisors have erupted and with a root formation of at least two-thirds.
In regard to the age of treatment it is associated with dental and bone age so it should be individualized for each case (Figure 2).25
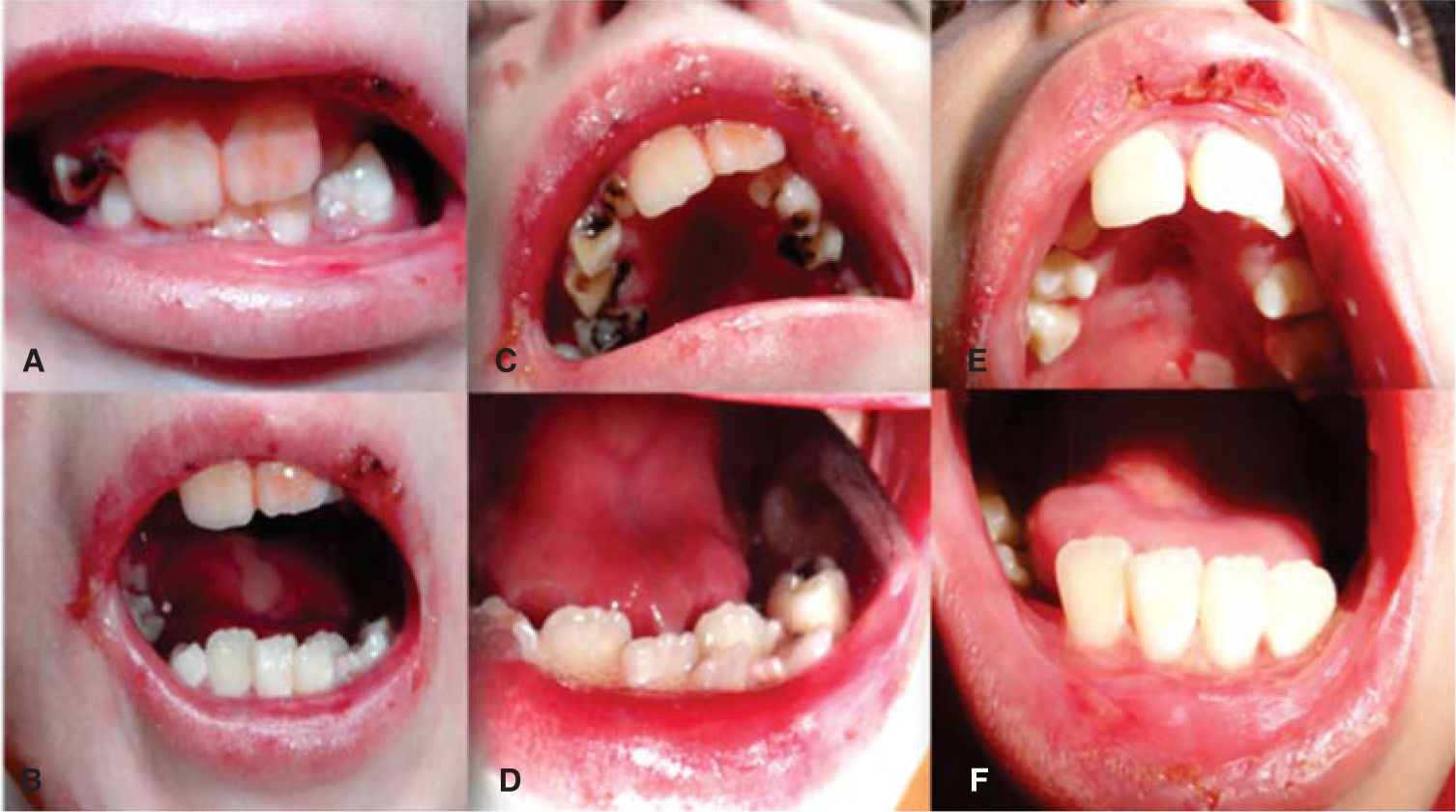
Clinical casesClinical case No. 18-year-old male patient with a diagnosis of dystrophic epidermolysis bullosa, referred from the Dermatology Service for dental assessment. Upon clinical exploration the patient presents multiple lesions in the skin of the face, neck and limbs that correspond to blisters in different stages of healing. The facial analysis reveals a mesofacial type, with decrease of the middle facial third, slightly convex profile, with a posterior position of the lower lip and soft pogonion. There is limitation of mouth opening with aninterincisal distance of 2 centimeters (Figure 3).
At intraoral examination large blistering lesions in the region of the hard palate over the midline, ulcers in the process of healing in the upper and lower labial mucosa, limitation of lingual mobility, with a smooth dorsal surface of the tongue and pale pink color consistent with depapillation by scarring and a blister on the midline are observed. Scarring tissue is observed in skin and on the corners of the mouth with blisters in process of healing (Figure 4).
A, B) Photographs in occlusion and maximum opening, intraoral photograph, C) initial upper arch, D) photograph of initial lower arch that shows severe crowding, E) pos-treatment photograph of the upper arch with proper alignment of the dental arches and eruption of the premolars, F) postreatment photograph of the lower arch with alignment of the incisors.
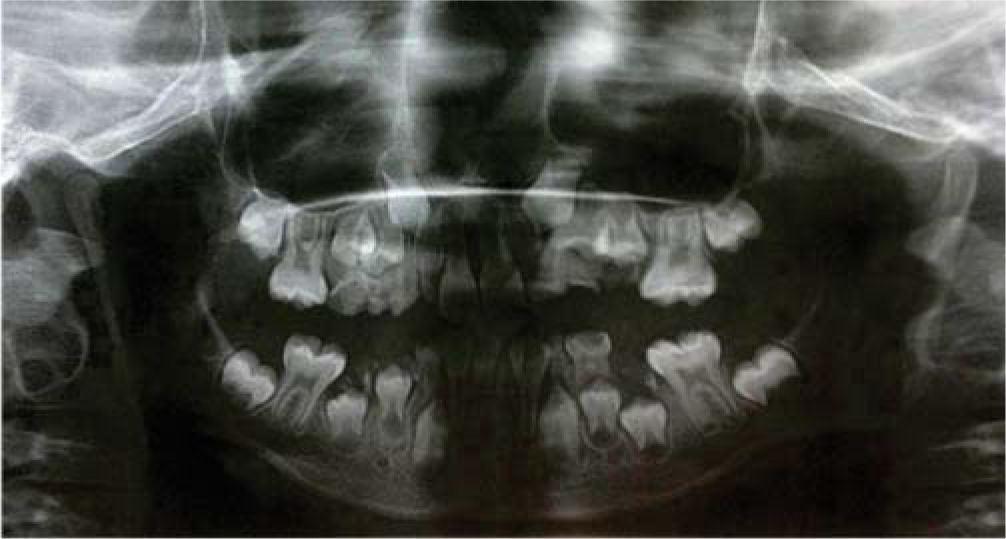
The patient is in the mixed dentition with presence of large carious lesions dental organs: 55, 54, 53, 52, 62, 63, 64, 74, 73 and 83. It may be observed the clinical absence of dental organs 65, 75, 84 and 85. Dental organs number 16, 26, 36 and 46 with caries of both enamel and dentin. Dental organs 11 and 21 are free of carious processes, dental organs 32, 31,41 and 42 exhibit severe crowding and are free of carious processes. A panoramic radiograph was requested and widespread crown destruction of all primary dentition is observed with an adequate path of eruption of the upper canines but with lack of space for their eruption (Figure 5).
An individual risk assessment was made using the CAMBRA index and concluded that the patient had high risk of tooth decay, so a prevention, rehabilitation and follow-up program was established.
Treatment planPreventionAn adequate brushing technique was indicated using a small brush with soft bristles and fluoridated paste with 1,450 ppm. In addition, mouthwashes of water and baking soda three times a day were prescribed. Topical applications of fluoride varnish every 6 months and dietary recommendations were made.
Elimination of infectious disease outbreaksThe patient was programmed for oral rehabilitation under general anesthesia due to the limitation of mouth opening, extension of treatment, risk of oral lesions and poor patient cooperation. Nasotracheal intubation was performed through fiberscope because of the difficult access to the airway. Patients with EB have risk of stenosis from the airway intubation maneuver, therefore the riskbenefit must be assessed meticulously to determine the treatment plan. The patient presented pseudosyndactilyso a consult from the Cosmetic and Reconstructive Plastic Surgery Department was requested. It was decided to carry out the surgery of the affected hand in the same surgical time.
The extractions of the dental organs 55, 54, 53, 52, 62, 63, 64, 65, 75, 74, 73, 83, 84 and 85 were performed and a resin-based restoration was placed in 16, 26, 36 and 46.
Interceptive guide of the occlusionThe enucleation of the first premolars was performed to promote an adequate eruption of the permanent lateral incisors and canines. Due to the patient´s diagnosis, the use of orthopedic appliances as space maintainers was a contraindications just the teeth enucleation was made (Figure 6).
Clinical case # 2Female patient, 7 years of age, with a diagnosis of dystrophic epidermolysis bullosa who comes in for dental assessment. Exploration of patient notes with injury exulcerativas in skin of neck, arms, nose, with difficulties for ambulation. Upon intraoral examination multiple blisters in the oral mucosa, in region of hard palate, cheeks and lateral border of the tongue are observed. There is limitation of mouth opening because of the formation of scarring tissue inside the oral cavity. Interincisal distanceis less than 1 centimeter and ankyloglossia is total. She has mixed dentition with abundant dental plaque and generalized erythema of the masticatory mucosa. Dental organs 52 and 62 exhibited mobility of 2mm and caries of the enamel and dentin (Figure 7).
Treatment planPreventionAt the initial phase oral hygiene technique education was performed using a small manual toothbrush with soft fibers and the use of a clorhexidine gluconate mouthwash as an auxiliary. An improvementij hygiene and conditions of the periodontal tissue was observed.
RehabilitationA non-traumatic rehabilitation technique was used in the primary upper lateral incisors using a glass ionomer-modified resin in the interproximal areas.
Guide of occlusionThe patient presents severe dental crowding, maxillary and mandibular compression and lack of space for the permanent dental organs. Since the patient did not present large dental caries, she did not undergo general anesthesia and therefore interceptive guide of occlusion was not performed. Due to the progressive nature of the disease in subsequent appointments an increase in the compression and in the crowding was observed forecasting difficulty in the eruption of the permanent canines and the possible ectopic eruption of the permanent first molars.
ConclusionsAmong the most relevant long term sequelae in the oral cavity in patients with dystrophic epidermolysis bullosa are microstomia, maxillary compression and subsequent crowding. These anomalies prevent good oral hygiene and an adequate oral food intake that has a direct impact on the patient´s nutritional status, their overall health and quality of life.
Dental treatments must be carefully planned for each individual because in some cases dental procedure´s techniques may be carried out in a conventional manner with rubber dam isolation and cavity preparation. In other cases the disease may present oral conditions that complicate dental treatment due to the microstomia and the obliteration of the buccal vestibule, making the isolation and even the access of rotary instruments inside the buccal cavity difficult. The purpose of the dental intervention is to always improve the patient´s quality of life, eliminate infectious disease outbreaks and prevent alterations of the stomatognatic system in the long term.
In the cases hereby presented, the first patient met the criteria for oral rehabilitation under general anesthesia due to dental caries and the severity of the lesions so the interceptive guide of occlusion was justified. In addition, during the same surgical time an attending physician from a different medical service intervened so that the patient benefited from receiving two needed treatments. In the second case, the patient did not meet the criteria for the procedure to be carried out under general anesthesia since the extension of the carious lesions was minimal. Therefore no dental organs were removed for an interceptive guide of occlusion and a gradual deterioration of the patient´s oral condition was observed with severe crowding and progressive lack of space.
By making a proper diagnosis and prediction of the malocclusion on the long term, interceptive treatments can be performed at an early age when the microstomia that makes dental treatment difficult is not present. Treatment through an interceptive guide of occlusion in patients with dystrophic epidermolysis bullosa provides a better quality of life, facilitates oral hygiene techniques and prevents complications such as interproximal caries and periodontal problems in the future. It is important to conduct an individual analysis, considering the benefits and risks of the intervention and assess in other types of epidermolysis bullosa the implementation of this protocol.
Due to the inherent risk of airway stenosis in patients with EB when performing the orotracheal or nasotracheal intubation, it is recommended to plan the surgical intervention in conjunction with other services in order to minimize the risk, however, the risk-benefit for each individual patient should always be assessed.