A 24-year-old patient attended the Orthodontics Clinic of the Division of Postgraduate Studies and Research, Faculty of Dentistry, UNAM, with a previous orthodontic treatment and absence of lower 1st premolars. The chief complaint was an unattractive facial appearance due to a forward position of the mandible and anterior open bite. Upon facial examination, in the frontal view, a leptoprosopic face, collapsed paranasal areas and incompetent lips were observed. In the vertical facial proportions, the lower third was increased. The lateral and oblique view showed a greater projection of the chin, a concave profile and an increased mentocervical length. Intraorally, the molar relationship was class III; a 2mm anterior open bite and complete anterior cross bite of 1mm were also observed. The patient presented a mild discrepancy of the dental midline as well. Orthodontic treatment was carried out in three phases: presurgical, surgical and postsurgical. In the presurgical phase dental decompensation was performed and the patient was prepared for surgery. In the surgical phase a segmental maxillary surgery from lateral incisor to lateral incisor was performed in order to produce a movement of sagittal rotation thus projecting the nasogenian area and improving incisor inclination. A mandibular setback via bilateral sagittal osteotomy was also performed. In the postsurgical phase ideal occlusal relationships were achieved in terms of canine class, molar class, overjet, overbite, centered dental midlines as well as a more harmonious profile.
Paciente de 24 años de edad, se presenta en la División de Estudios de Postgrado e Investigación de la Facultad de Odontología de la UNAM, con tratamiento ortodóncico previo y ausencia de primeros premolares inferiores. El motivo principal de consulta es la apariencia facial poco atractiva debido a la posición hacia adelante de la mandíbula y la mordida abierta anterior. A la revisión clínica extraoral, en la vista frontal se observa una cara leptoprosopa, áreas paranasales colapsadas y labios incompetentes. En las proporciones faciales verticales, reveló el tercio inferior aumentado. La vista lateral y oblicua mostró mayor proyección del mentón, perfil cóncavo y una longitud mentocervical aumentada. Intraoralmente, la relación molar clase III, mordida abierta anterior de 2mm y mordida cruzada anterior completa de 1mm. Ligera discrepancia en la línea media dental. El tratamiento ortodóncico se lleva a cabo en tres fases: prequirúrgica, quirúrgica y postquirúrgica. En la fase prequirúrgica se descompensó dentalmente al paciente y se preparó para la cirugía. En la fase quirúrgica se realizó una segmentaria de maxilar de lateral a lateral para realizar un movimiento de rotación sagital proyectando la zona nasogeniana y mejorando la inclinación de los incisivos anteriores en combinación con retroceso mandibular mediante osteotomía sagital bilateral. En la fase postquirúrgica se lograron relaciones oclusales ideales, en términos de clase canina, clase molar, resalte, sobremordida, y la coincidencia de las líneas medias dentales así como un perfil más armónico.
Correction of severe dentoskeletal malocclusions has always had a triple objective for achieving: functional efficiency, structural balance and aesthetics.1,2 Physical health of patients with severe malocclusions may be altered or compromised in several ways such as masticatory dysfunction, speech disorders, resistance of the upper airway, compromised oral hygiene and temporomandibular joint dysfunction.3 However, the aesthetic aspect of a severe malocclusion is related with its psychosocial impact and the positive effects of having an attractive face. With regard to self- confidence and self-respect, they could be considered more important than the associated physical problems.4 There are factors that affect the welfare of an individual with severe malocclusion: the experience of physical pain/discomfort (function), psychology (i.e., in connection with the appearance of the person and the self-esteem), and social function (as interactions with others).4
In cases of malocclusions with severe dentoskeletal discrepancies, there are usually three possible therapeutic options: early growth modification, dental compensation or a surgical-orthodontic treatment.1 In recent years, a growing number of patients choose to undergo orthognathic surgery in order to correct a severe malocclusion that has not been solved with conventional orthodontic treatment.5 Patients with skeletal class III malocclusion may present mandibular prognathism, maxillary retrusion or a combination of both. Mandibular prognathism or skeletal class III malocclusion with a prognathic mandible has been considered as one of the most serious maxillofacial deformities.6
CASE REPORTA patient of 24 years of age attended the Division of Postgraduate Studies and Research at the Faculty of Dentistry of UNAM with a history of a prior orthodontic treatment and absence of lower first premolars. The main reason for consultation is an unattractive facial appearance due to the forward position of the mandible and an anterior open bite (Figures 1 to 4).
Clinical characteristics. Upon extraoral clinical examination, in the front view, the patient showed a leptoprosopic face; collapsed paranasal areas and incompetent lips. The analysis of vertical facial proportions revealed an increased lower third (Figure 2).The lateral and oblique view showed a greater chin projection, a concave profile, an acute nasolabial angle and an augmented mento-cervical length with a well- defined mandibular lower edge. Intraorally, absence of first lower premolars, class III molar relationship, a 2mm open bite and a complete 1mm crossbite were observed (Figure 3).
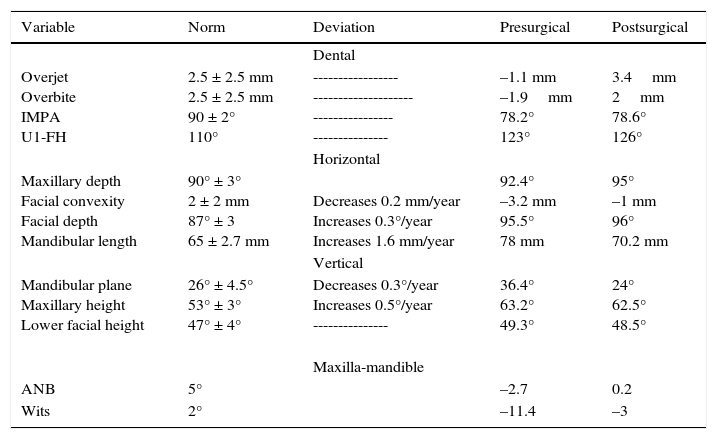
Pretreatment radiographic records included alateral headfilm and an ortopantomography (Figures 5 and 6). The cephalometric analysis (Table I) revealed a skeletal class III due to mandibular prognathism, an increased vertical height, upper incisor retroclination and lower dental proclination produced by physiological compensation.
Cephalometric values.
| Variable | Norm | Deviation | Presurgical | Postsurgical |
|---|---|---|---|---|
| Dental | ||||
| Overjet Overbite IMPA U1-FH | 2.5 ± 2.5 mm 2.5 ± 2.5 mm 90 ± 2° 110° | ----------------- -------------------- ---------------- --------------- | –1.1 mm –1.9mm 78.2° 123° | 3.4mm 2mm 78.6° 126° |
| Horizontal | ||||
| Maxillary depth Facial convexity Facial depth Mandibular length | 90° ± 3° 2 ± 2 mm 87° ± 3 65 ± 2.7 mm | Decreases 0.2 mm/year Increases 0.3°/year Increases 1.6 mm/year | 92.4° –3.2 mm 95.5° 78 mm | 95° –1 mm 96° 70.2 mm |
| Vertical | ||||
| Mandibular plane Maxillary height Lower facial height | 26° ± 4.5° 53° ± 3° 47° ± 4° | Decreases 0.3°/year Increases 0.5°/year --------------- | 36.4° 63.2° 49.3° | 24° 62.5° 48.5° |
| Maxilla-mandible | ||||
| ANB | 5° | –2.7 | 0.2 | |
| Wits | 2° | –11.4 | –3 |
Treatment plan. An interconsultation with the Department of Oral and Maxillofacial Surgery of the Division of Postgraduate Studies and Research of the Faculty of Odontology of the UNAM was conducted. A segmental maxillary surgery from lateral incisor to lateral incisor was suggested to perform a sagittal rotation movement thus projecting the nasogenian area and improving upper incisor inclination in combination with a mandibular setback through a bilateral sagittal osteotomy, presurgical and postsurgical orthodontics. The surgical treatment was planned with the aim of achieving facial aesthetics and optimal functional occlusion. A second surgery was planned for nasogenian grafting, if necessary, after post-treatment evaluation.
Presurgical orthodontics phase. After restoring the decayed teeth and performing a professional dental cleaning, treatment was begun with 0.022” × 0.028” Roth system.
The presurgical facial features show the performed decompensation for surgery (Figures 7 and 8).The upper and lower arches were aligned until a 0.019” x 0.025” stainless steel archwire could be placed (Figures 9 and 10). Upper third molars were extracted. At the end of this stage presurgical radiographic records were obtained (Figures 11 and 12). In order to assess and predict the outcome of the planned surgical approach, a surgical prediction with cephalometric tracings was performed.
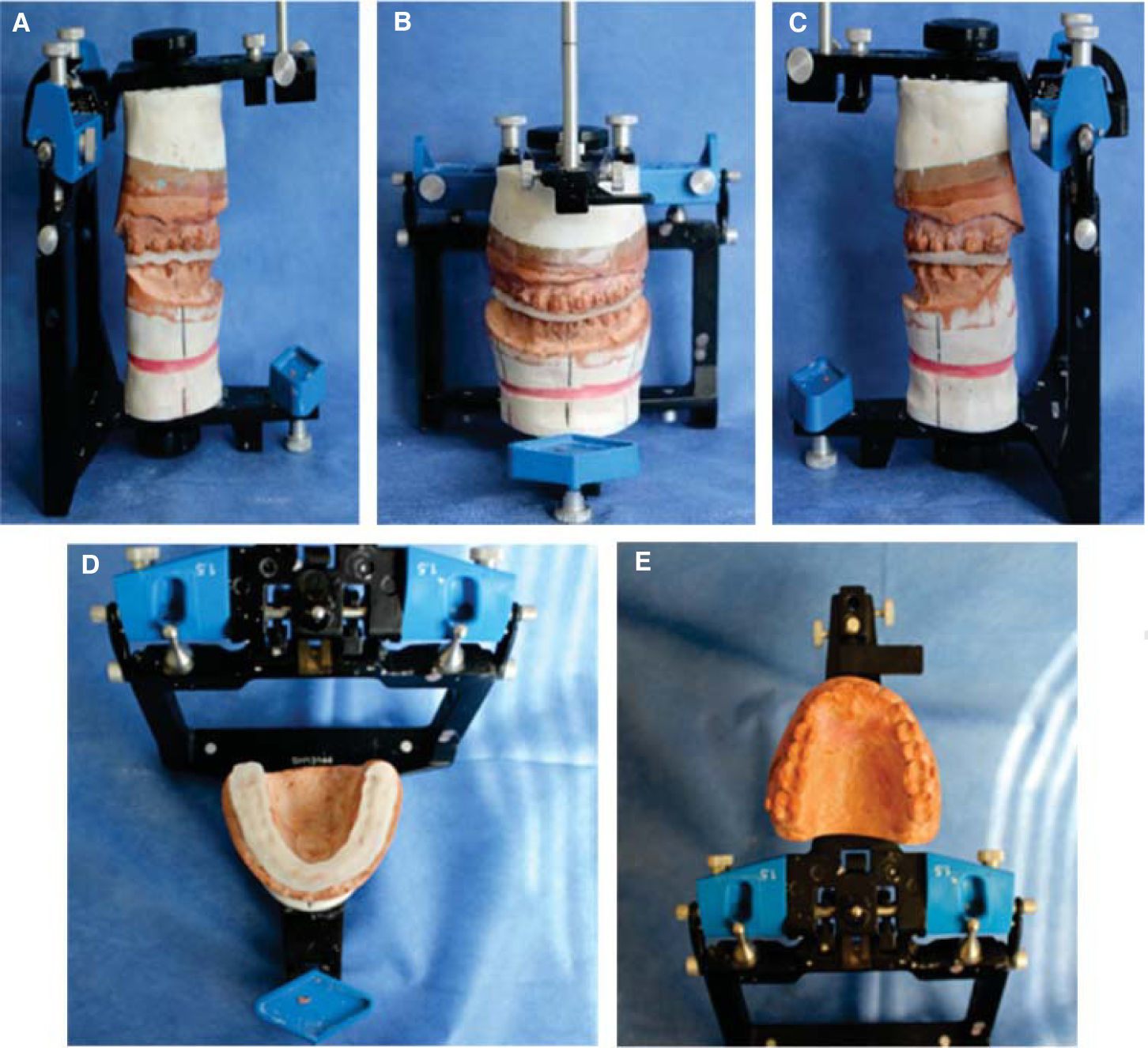
All measurements, calculations and analysis were performed with the Nemoceph program (Figure 13). Based on these calculations the convenient amount of osteotomy was decided. The cuts sections in the maxilla and mandible were adjusted to the desired occlusal relation.7 The mandibular setback was programmed at 5mm indicating good posterior intercuspation with an aesthetically pleasing profile. The following steps in the planning sequence were model surgery and manufacture of the occlusal splints that would be used in surgery. The models were mounted on a semi-adjustable articulator.
Surgery of models was performed. The individual dental models were repositioned, simulating the movements of the mandible as represented by the digital prediction. An acrylic intermediate occlusal splint was manufactured. Afterwards, the upper model was re-positioned in the semiadjustable articulator (Figure 14A). Then the mandibular model was repositioned to oppose the upper model, simulating the final position of the occlusion during surgery. Based on this position the final occlusal splint was made (Figures 14B-E).
Surgical procedure. Surgery was performed with the support of the Maxillofacial Surgery Department of the Division of Postgraduate Studies and Research at the Faculty of Odontology of the UNAM. Initially, the maxillary anterior segmentation from lateral incisor to lateral incisor was performed.8 The anterior segment of the maxilla was repositioned rotating it sagittally thus projecting the nasogenian area and improving incisor inclination (Figure 15A and B). In the mandible a bilateral sagittal osteotomy was conducted using surgical saws toper form a retraction of 5mm (Figure 15C).9,10 Rigid fixation was placed in the maxilla through the use of four-hole miniplates and a screw on both sides (Figure 15B). An intermediate splint was used to secure the mandible in the correct position (Figure 15D). Genioplasty would be carried out as a secondary procedure, if necessary, after post-surgical assessment of the scarring. During surgery mini-implants were placed to be used both for intermaxillary fixation (due to the fact that during segmental osteotomy the archwires were cut) as well as for the use of intermaxillary elastics for 30 days during the immediate postoperative phase to achieve maximum stability.
Postsurgical orthodontics phase. Active orthodontic treatment was resumed four weeks after surgery. The objective was to achieve ideal occlusal relationships, in terms of canine class, molar relationship, overjet, overbite, and matching dental midlines. During postsurgical orthodontics 0.019” x 0.025” SS archwires were maintained. All residual spaces were closed and intercuspation was refined with 0.019” x 0.025” braided archwires and short intermaxillary elastics.
Twelve months after the surgical procedure appliances were removed (Figures 16 to 19); in the retention phase, a lower fixed retainer and an upper circumferential retainer were placed. Final radiographic records were obtained (Figures 20 and 21) and treatment changes were assessed through superimposition (Figure 22). Before and after treatment cephalometric values are compared in table I. Total treatment time was 3 years 10 months.
Stablishing objectives on the outcome of the orthodontic-surgical treatment is a crucial part of the treatment planning process. Therefore a multidisciplinary team approach when recommending surgery for a patient requires good clinical judgment and experience. After initial assessment the presurgical phase of orthodontic treatment was initiated with the goal of achieving arch coordination and placing each tooth in its correct position always considering the initial objectives. In this case we performed a cephalometric prediction at the end of the pre-surgical phase.11
In patients who have a good maxillary position and in whom it is not necessary to perform a complete maxillary advancement, maxillary segmental osteotomy has a better potential for correcting dental inclinations as well as the collapse in the nasogenian area without using grafts in cases with slight depression. These movements have been shown to have excellent postsurgical stability while improving dental position and facial harmony. During the mandibular osteotomy a retraction was performed which significantly improved mandibular position.12 During the post-surgical phase there were notable changes in the soft tissues contour of the nose and lip.13
In this case, postsurgical orthodontics was conducted for 12 months since it mainly involves detailing of the occlusion and retention. Duration of the final phase of orthodontics depends on the degree of preparation achieved during the preoperative treatment.12,14 However, it is important to highlight that a good retention helps maintain the final occlusion achieved surgically and long-term occlusal stability.
CONCLUSIONSClass III patients who suffer from skeletal malocclusion, facial aesthetics and problems of selfesteem lead us to take as an alternative a combination treatment for the correction of maxillofacial deformities. Orthodontics supplemented with orthognathic surgery offers a good option to correct this kind of anomalies. Both the orthodontist and the surgeon must have the required expertise and work together in all treatment stages, both presurgical and postsurgical. The orthodontist must be conscious of dental and jaw movement limits as well as those of the postsurgical treatment plan in order to finish with good results and achieve a satisfactory outcomeat a dental, facial and psychological level.
Graduate of the Orthodontics Department.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia