Craniofacial asymmetry is expressed as the difference in size between two parts of the face. It is originated by a discrepancy in size and position between the cranial base and the maxilla, between the cranial base and the mandible, or between the maxilla and the mandible. When the craniofacial asymmetry is severe and the patient has completed growth, the indicated treatment is performed in conjunction with orthodontics and orthognathic surgery. The clinical case of a 20-year-old female patient who underwent orthodontic-surgical treatment of a skeletal class III malocclusion due to maxillary retrusion and mandibular prognathism, severe facial asymmetry, right condylar hyperplasia, right side maxillary inclination, anterior open bite and transversal compression of the maxillar is hereby presented. The treatment goals were to provide a stable occlusion, to obtain facial symmetry and improve function by the correction of the transverse, sagittal and vertical dento-skeletal problem. The treatment plan was orthodontic-surgical using 0.022” × 0.025” slot Roth prescription, which consisted in three phases: 1) Pre-surgical orthodontics, 2) surgical phase and 3) Post-surgical orthodontics. The surgical treatment plan consisted of a triple orthognathic surgery: Le Fort I osteotomy (asymmetric maxillary intrusion of 3mm on the right side and 2mm on the left side and a maxillary advancement of 3mm), asymmetric bilateral sagittal osteotomy of the mandible and mentoplasty. In addition to these surgical procedures, a nasal post of septal cartilage was also placed. The obtained results, both facial and occlusal, were satisfactory, achieving the orthodontic goals and fulfilling the patient's expectations.
ConclusionsOrthognathic surgery in conjunction with orthodontics offers a definitive solution for dentofacial corrections in patients who have completed their growth period; giving the patient facial symmetry, occlusal stability and adequate function of the stomatognathic apparatus. The establishment of a common diagnosis and objectives between the maxillofacial surgeon and the orthodontist in an orthodontic-surgical case is crucial to obtain an adequate and favorable result for the patient.
La asimetría craneofacial se expresa como la diferencia en tamaño entre dos partes de la cara, están originadas por la discrepancia en tamaño y posición entre la base de cráneo y el maxilar, entre la base de cráneo y la mandíbula, o entre el maxilar y la mandíbula. Cuando la asimetría craneofacial es severa y el paciente ha terminado completamente su crecimiento, el tratamiento indicado se realiza por medio de la Ortodoncia y la Cirugía Ortognática en conjunto. Se presenta el caso clínico de un paciente femenino de 20 años de edad a quien se le realizó tratamiento ortodóntico-quirúrgico con maloclusión esquelética clase III por retrusión maxilar y prognatismo mandibular, asimetría facial severa, hiperplasia condilar derecha, canteamiento maxilar del lado derecho, mordida abierta esquelética anterior y compresión transversal del maxilar. Los objetivos del tratamiento fueron: proporcionar una oclusión estable, crear una simetría facial y mejorar la función por medio de la corrección del problema transversal, sagital y vertical dentoesquelético. El plan de tratamiento fue ortodóntico-quirúrgico utilizando aparatología fija con prescripción Roth 0.022” × 0.025” y consistió en tres fases: 1) ortodoncia prequirúrgica, 2) fase quirúrgica y 3) ortodoncia postquirúrgica. El plan de tratamiento quirúrgico consistió en una cirugía ortognática triple: osteotomía LeFort I (intrusión maxilar asimétrica de 3mm del lado derecho y 2mm de descenso del lado izquierdo y un avance maxilar de 3mm), osteotomía sagital bilateral asimétrica de las ramas mandibulares y mentoplastia; aunado a estos procedimientos quirúrgicos, también se realizó la colocación de un poste nasal de cartílago septal. Los resultados obtenidos fueron satisfactorios, tanto facial como oclusalmente, logrando los objetivos ortodónticos planteados en un inicio y cumpliendo con las expectativas del paciente.
ConclusionesLa cirugía ortognática en conjunto con la Ortodoncia ofrece una solución definitiva para las correcciones dentofaciales en pacientes que han terminado completamente su periodo de crecimiento; otorgando al paciente una simetría facial, estabilidad oclusal y función adecuada del aparato estomatognático. El establecimiento de un diagnóstico y objetivos comunes entre el cirujano maxilofacial y el ortodoncista ante un caso ortodóntico-quirúrgico es crucial para obtener un resultado adecuado y favorable para el paciente.
Modern society puts too much emphasis on physical appearance. Facial appearance and lack of aesthetics affect the self-esteem of the patient and his or her acceptance by society; this in general, affects their quality of life.1
The term «dentofacial deformity» is defined as a significant deviation from the normal proportions of the maxillo-mandibular complex that negatively affects the relationship of the teeth with their arch and the relationship of each arch with its own antagonist.2
The physical health of patients who present severe malocclusion is disrupted or compromised in different ways; such as: alterations in mastication, speech disorders and decreased permeability of the upper airway. Oral hygiene is compromised also and temporomandibular joint dysfunctions may be present.3
In cases of severe malocclusion with skeletal discrepancy, there are three possible options: early growth modification, orthodontic camouflage by means of a dental compensation or a combination treatment of orthodontics and orthognathic surgery.4
Treatment with corrective orthognathic surgery is indicated in cases of severe facial deformities that cannot be corrected with orthodontic treatment only.5
ObjectiveTo provide a stable occlusion, create facial symmetry and improve function by means of the correction of the transverse, sagittal and vertical dento-skeletal problem.
CASE REPORTThe surgical-orthodontic treatment of a 20-year-old woman who attended the Orthodontics Clinic of the Division of Post-Graduate Studies and Research at UNAM with skeletal discrepancies in all three planes of space: sagittal (class III malocclusion), vertical (maxillary canting) and transverse (facial asymmetry) is hereby presented. Her main reason for consultation was: «I have a deviated bite».
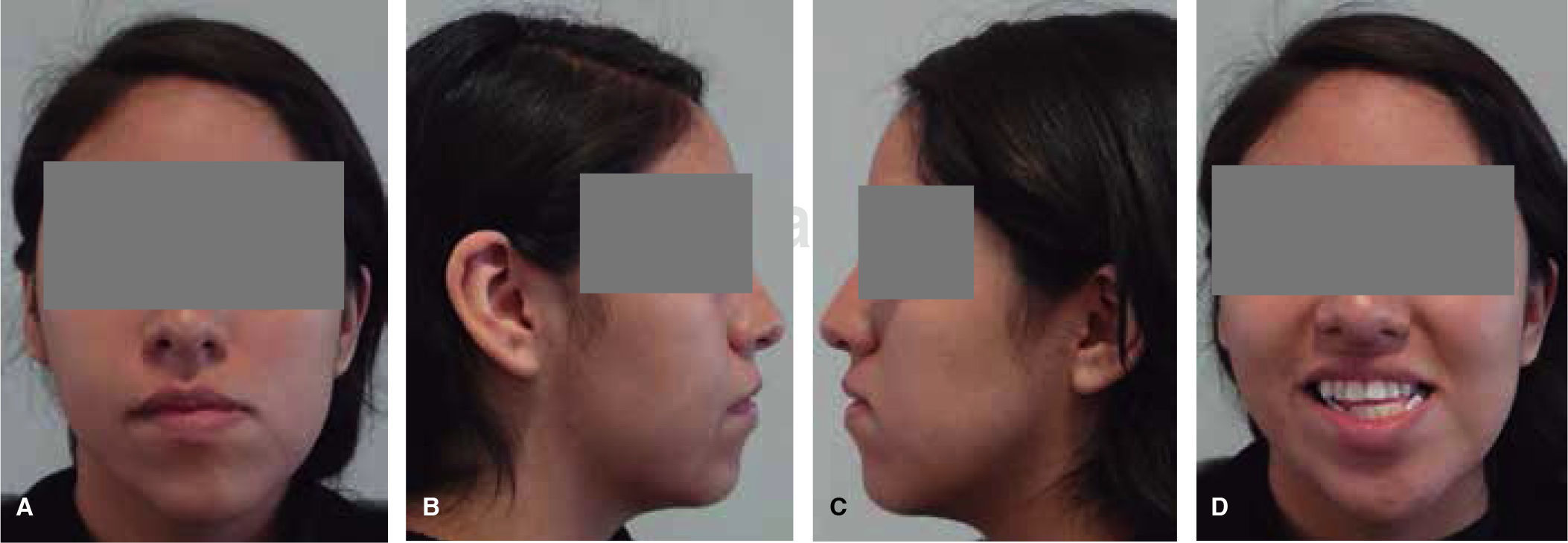
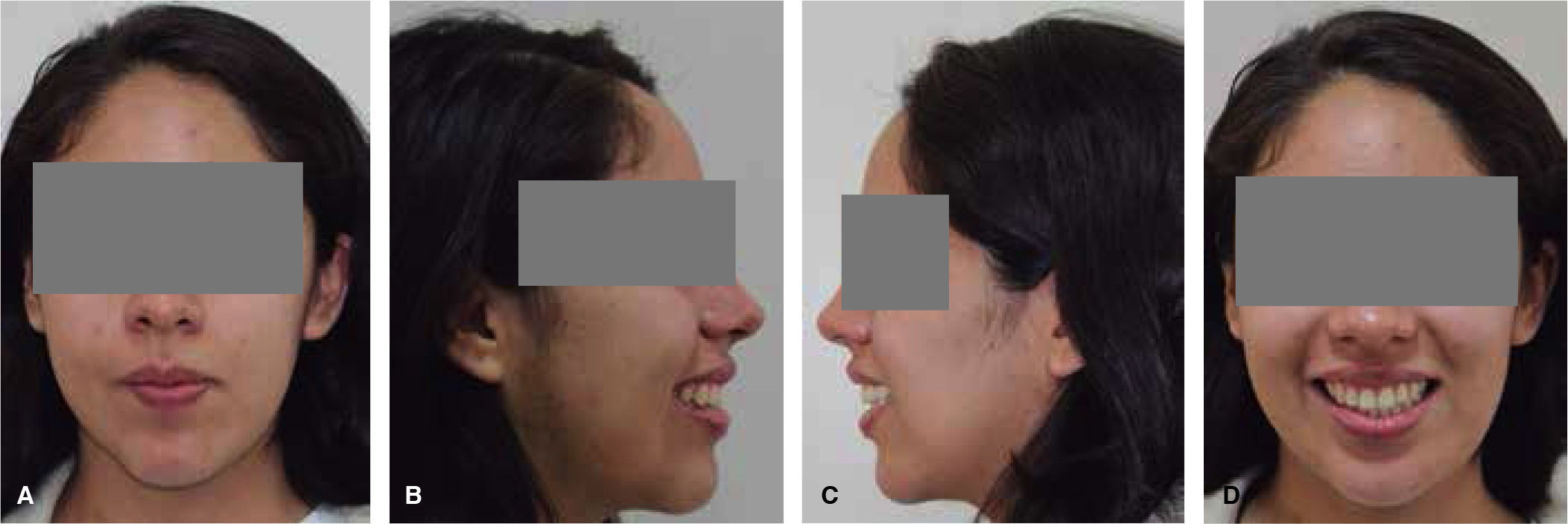
Clinical characteristicsUpon facial examination, the patient showed an oval-shaped face, deficient Para nasal areas, increased lower third of the face, a severe facial asymmetry which included the superciliary, bipupillary, sub nasal and commissural planes as well as a clearly deviated mandible to the left side.
Upon facial profile and oblique photograph examination a depression of the middle third of the face and a straight profile may be observed (Figure 1).
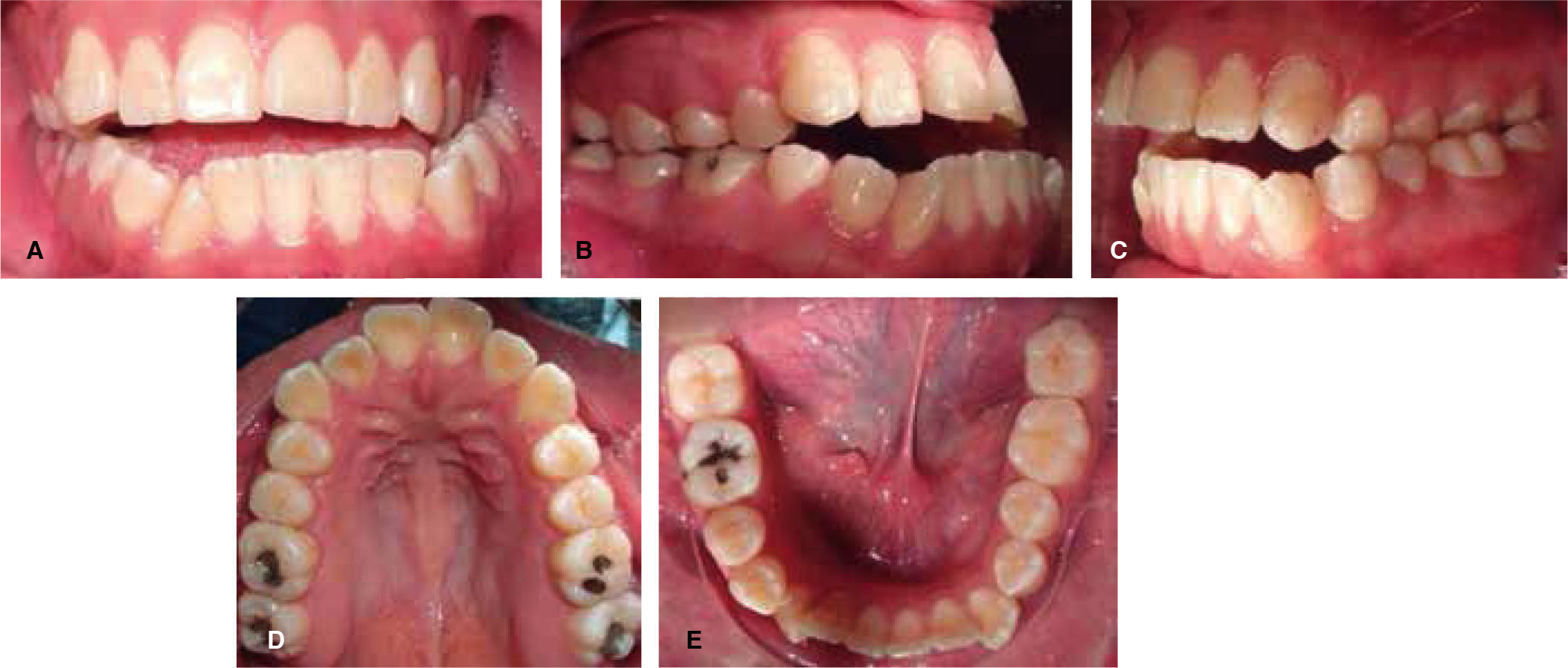
Intraorally the patient presented a molar class III, left canine class II and right class III, anterior open bite and posterior crossbite, 2mm overjet and -2.5mm overbite. She also presented mild crowding in the upper arch and moderate in the lower jaw. Non-coincident upper and lower dental midlines (Figure 2).
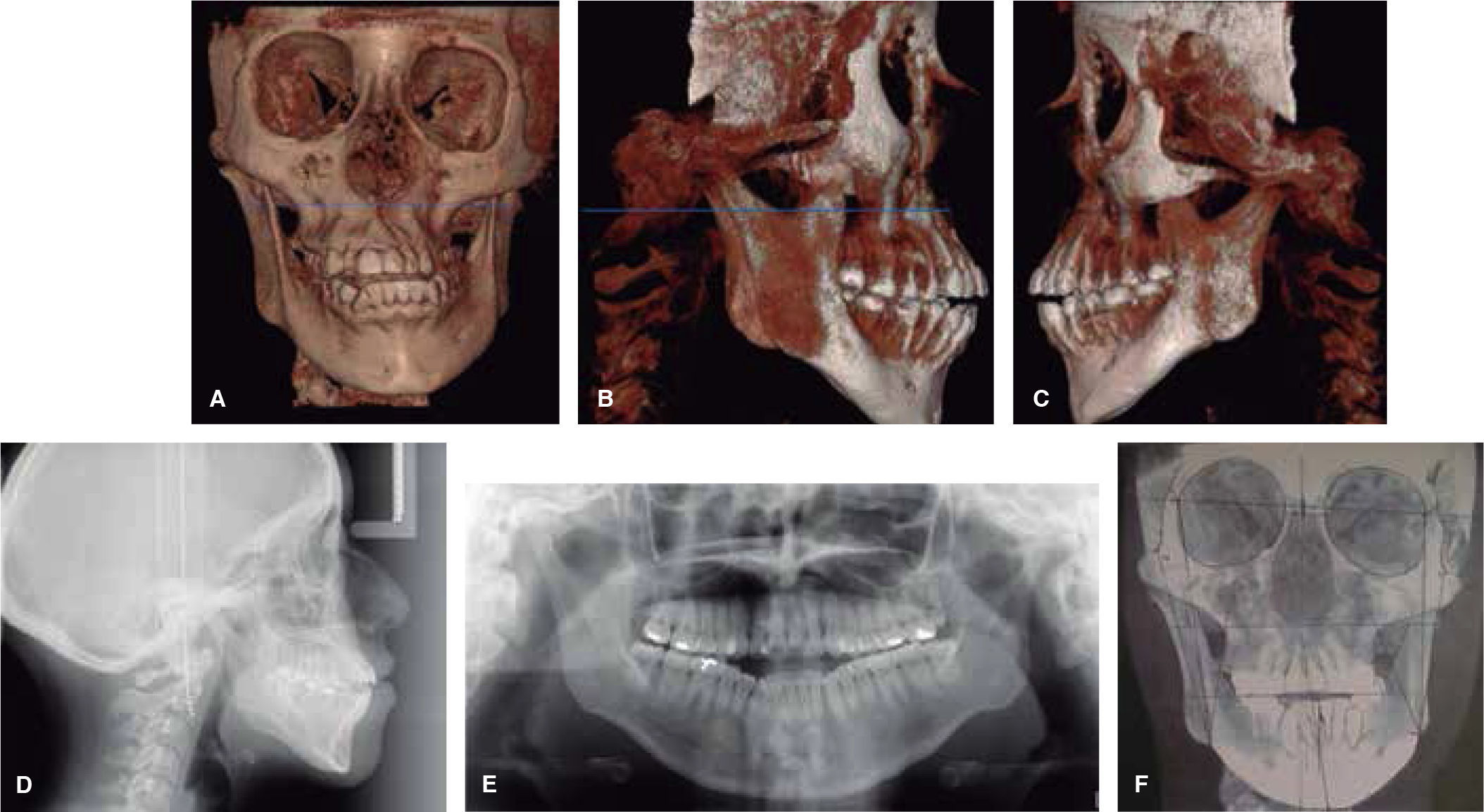
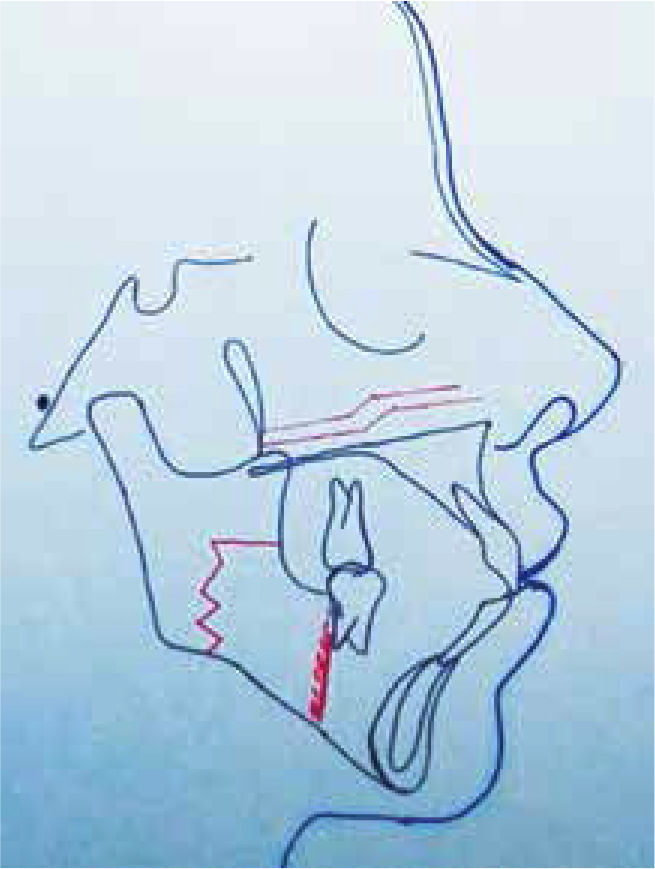
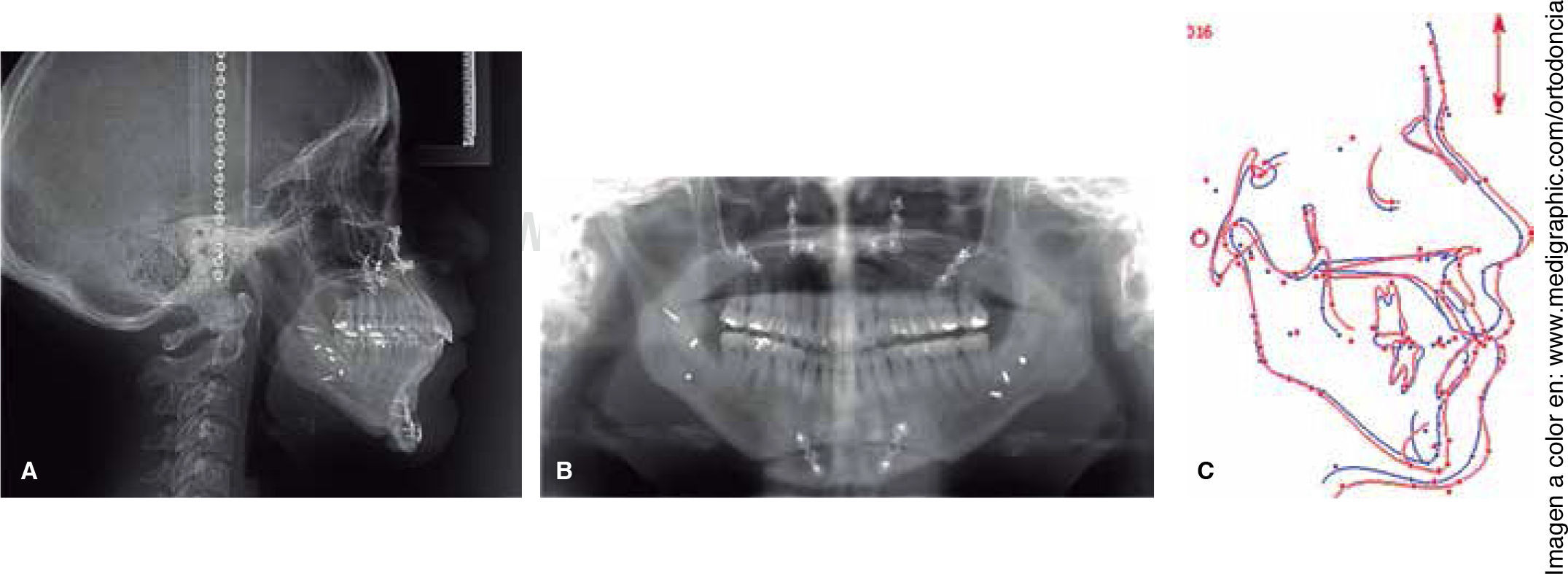
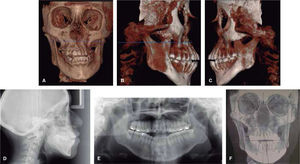
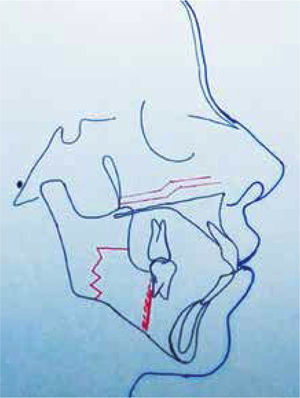
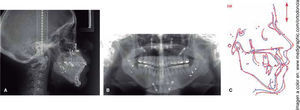
To perform the cephalometric diagnosis, panoramic radiograph, lateral headfilm and a CT cone-beam were obtained (Figure 3). The patient was diagnosed as a skeletal class III due to maxillary retrusion and mandibular prognathism, mandibular deviation due to laterognathia, right condylar hyperplasia maxillary cant to the right side, vertical growth pattern, skeletal open bite, left posterior crossbite, mild transverse compression (3mm) of the maxilla, dental biprotrusion and dental proclination.
Treatment planAn interdisciplinary treatment plan was performed between the Department of Orthodontics and the Department of Oral and Maxillofacial Surgery, which consisted of three phases:
- •
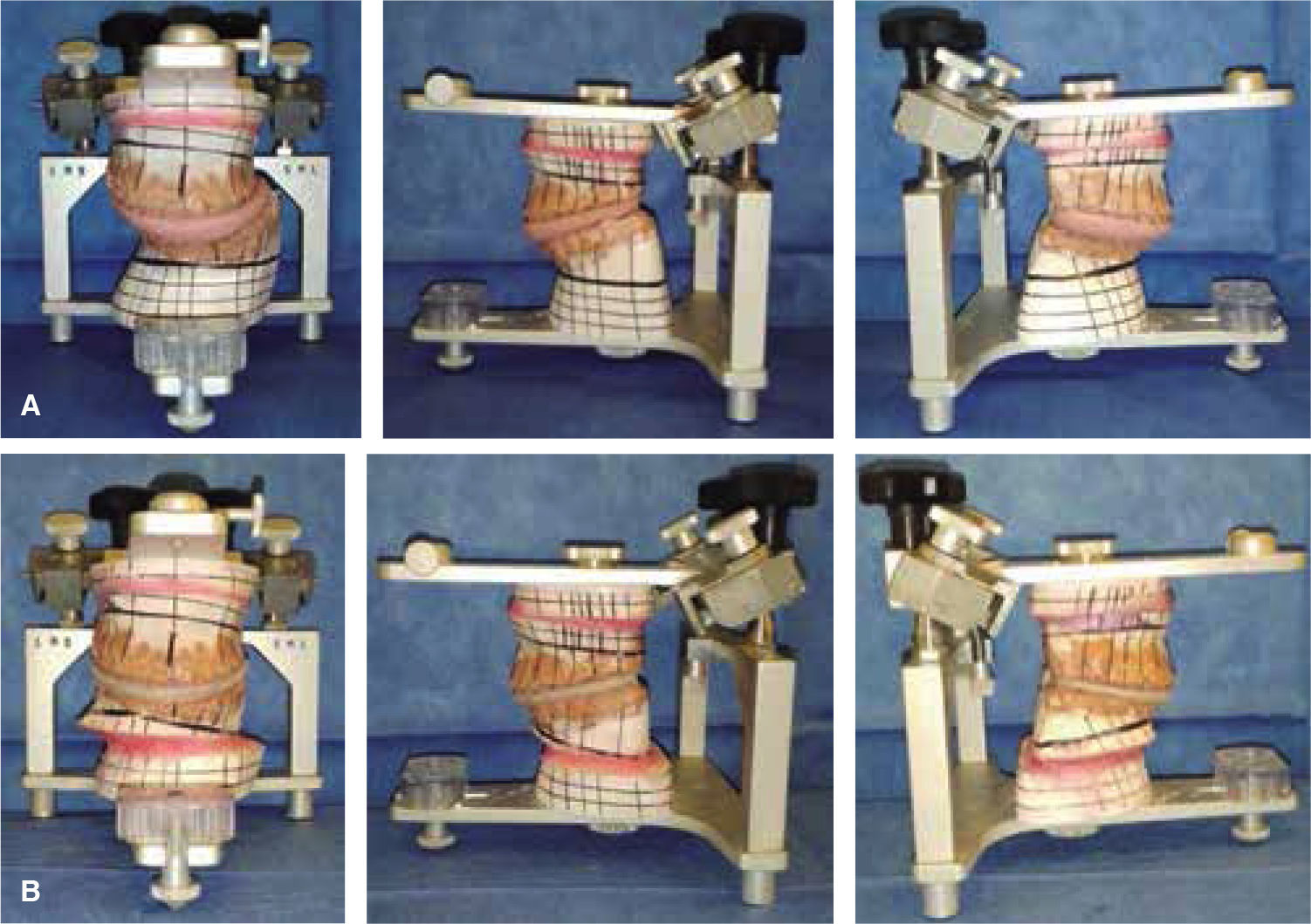
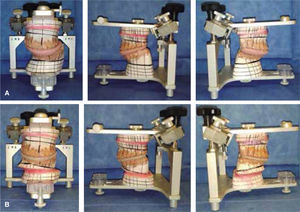
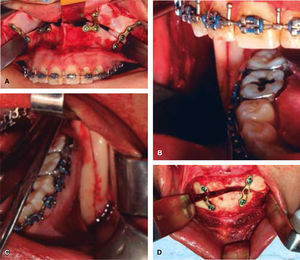
Phase 1: Pre-surgical orthodontics. Fixed appliances, 0.028” × 0.022” slot Roth prescription was placed; the stages of leveling and alignment were performed as well as major mechanics decompensating completely the patient in order to place pre-surgical 0.019” × 0.025” stainless steel archwires. Crimpable hooks were added (Figures 4, 5 and 6) and third molar extractions were also performed. Once the upper and lower arches were consolidated it was proceeded to the surgical stage.
- •
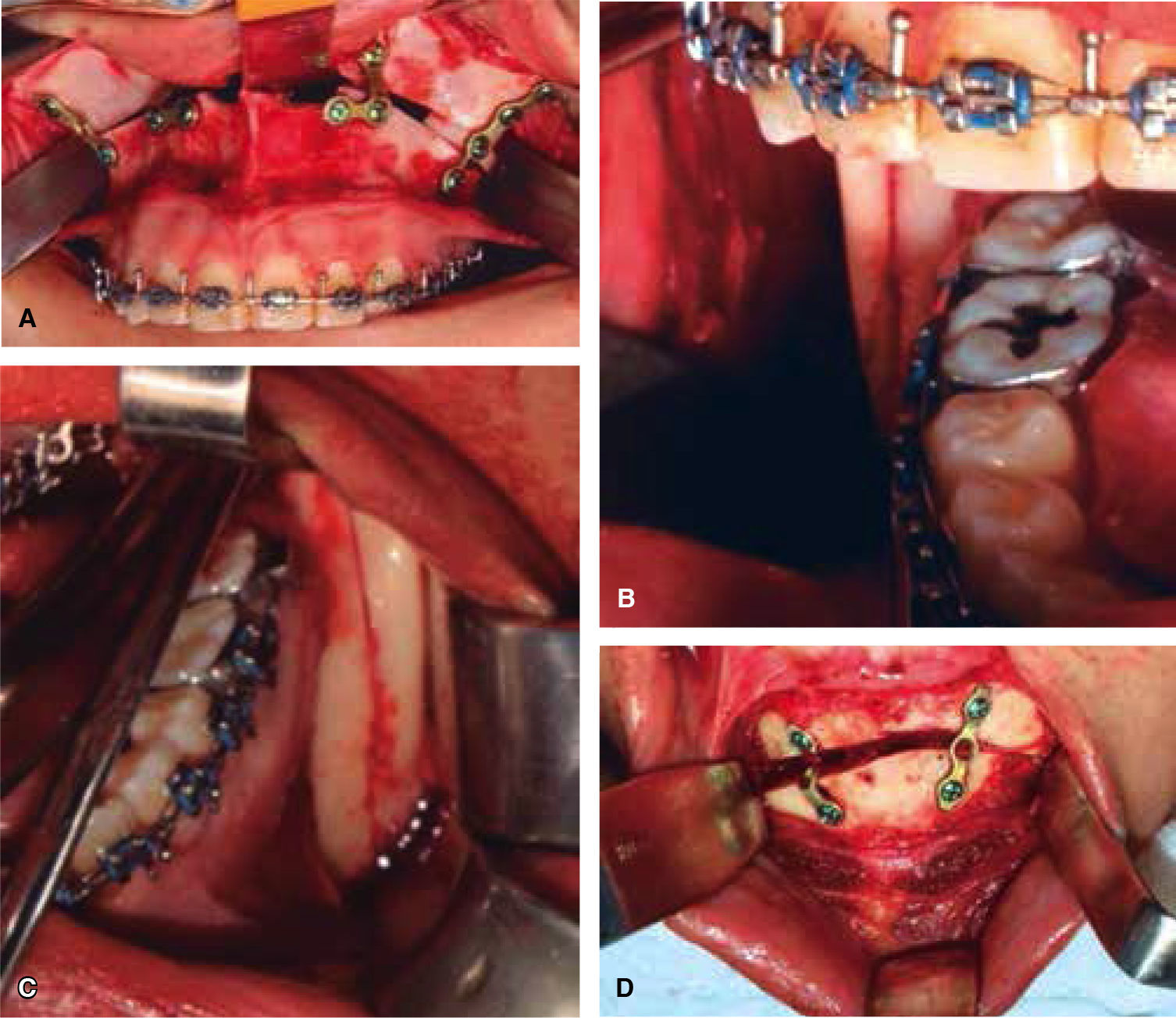
Phase 2. Orthognathic surgery. The surgical treatment consisted in a triple orthognathic surgery: Lefort I osteotomy (asymmetric maxillary intrusion of 3mm on the right side and 2mm downward movement on the left side; maxillary advancement of 3mm), bilateral sagittal osteotomy of the mandibular ramus (correction of laterognathia) and mentoplasty (chin asymmetry correction). In addition to these procedures, a nasal post of septal cartilage was placed (Figures 7 and 8).
Rigid fixation was used with mini mini-plates and mini-screws in the maxilla, mandible and chin.
At the end of surgery, intermaxillary fixation over the crimpable hooks of the surgical archwires was placed for two weeks, with the help of an elastomeric chain.
- •
Phase 3. Post-surgical orthodontics. The orthodontic treatment was active 3 months and a half after the orthognathic surgery to achieve a satisfactory level of bone, muscle, and occlusal stability.
Two weeks after the surgery, the patient was scheduled for a control appointment. Intermaxillary elastics were placed to prevent the patient's tendency to deviate the mandible.
Bracket repositioning was performed with the aid of a panoramic X-ray and the following archwire sequence was used: 0.016” × 0.022” NiTi, upper and lower; 0.017” × 0,025” NiTi, upper and lower; 0.019” × 0.025” NiTi upper and lower and finally, upper and lower 0.019” × 0.025” stainless steel arch wires were placed to consolidate the arches.
Space closure of the remaining spaces was performed and short intermaxillary elastics were used. The goal of this phase was to maintain the molar and canine class I, a good occlusal sagittal and transverse relationship of the upper and lower arches and coincident dental midlines.
After appliance removal, final retainers were placed; in the lower arch fixed retention with a 0.0175” twisted wire was placed from left first premolar to the right first premolar and on the upper arch, a circumferential retainer was indicated. In addition, a myofunctional retainer for nighttime use was fabricated as a reminder for the asymmetric musculature of the patient.
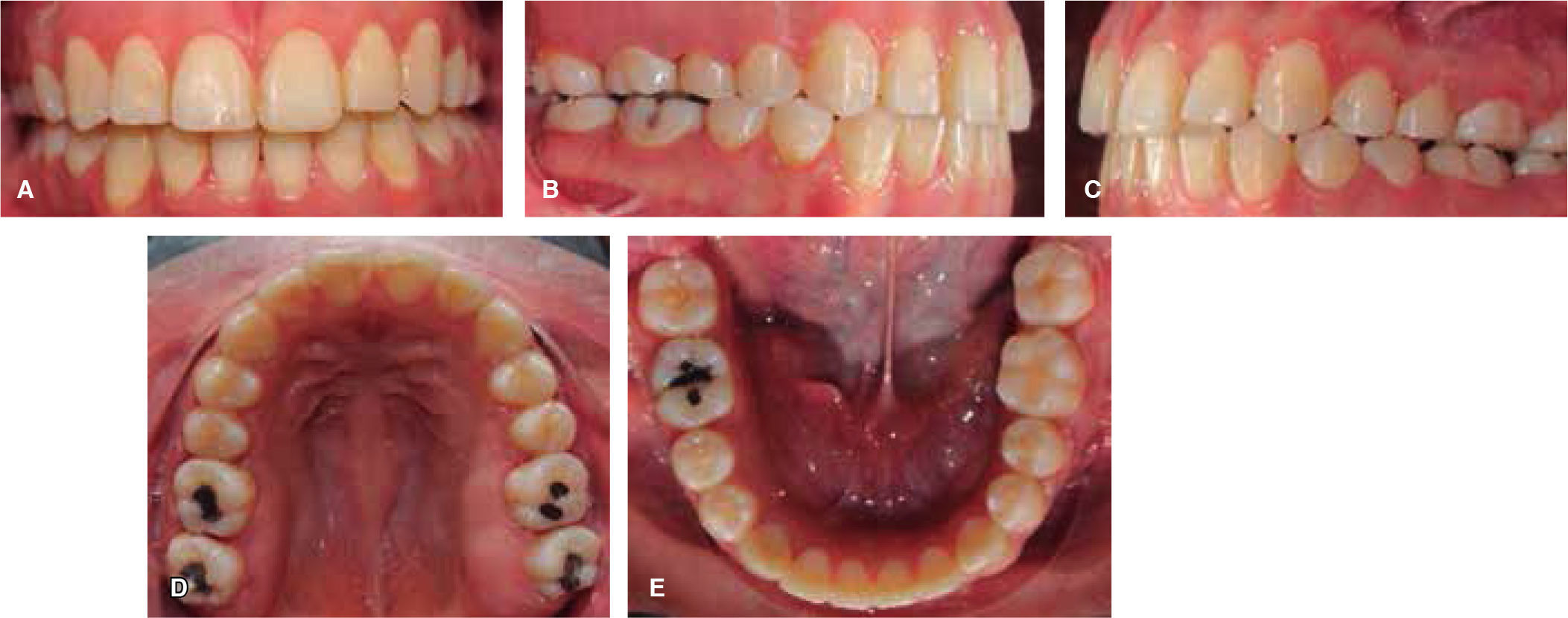
RESULTSThe initially set dental objectives were achieved: molar and canine class I on both sides, matching midlines, coordination of upper and lower arches, normal overjet and overbite and the dental crowding was corrected (Figure 9).
The patient gained a consonant smile due to the correction of the maxillary cant.
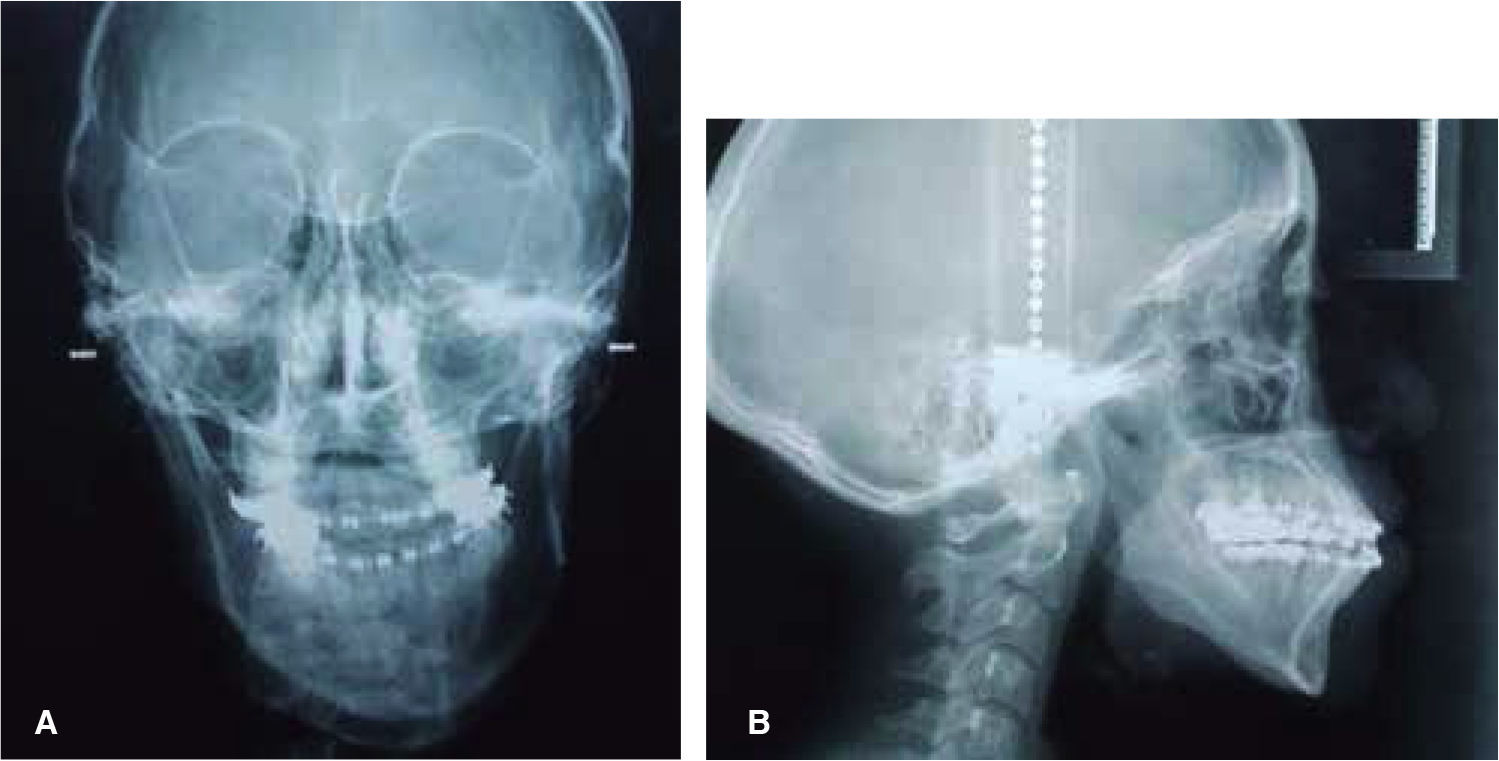
Facially, the asymmetry was corrected, the tip of the nose was raised, the zygomatic-malar area was advanced and a normal maxillo-mandibular relationship in the three planes of space: sagittal, transverse and vertical was obtained (Figures 10 and 11).
Surgery of the maxilla and retroposition of the mandible should be planned accordingly to the desired changes in the patient's profile and soft tissues. It is also important to consider that when bimaxillary osteotomy is performed there is great potential to increase or decrease the vertical facial height hence this surgery should be planned in accordance to the aesthetic requirements of the patient since the soft tissues are directly affected either by relaxing or stretching.6 In the case hereby presented; the vertical facial height was maintained resulting in a very favorable outcome for the patient's aesthetics.
S.H Baek, et al., demonstrated that asymmetric mandibular setback procedures with manual technique for condyle repositioning are favorable and do not significantly affect the position of the articular disc. In this case, an asymmetric mandibular osteotomy was performed without any TMJ problems after a 1-year post-surgical follow-up.8
In the present case, the patient had a mandibular asymmetry toward the left; Severt et al.,9 reported that in 85% of the patients with mandibular asymmetries in their study the deviation was towards the left side.
The post-surgical orthodontic phase lasted 3 months in this case, in which final detailing of the case was performed. The duration of the postsurgical orthodontic phase will depend on the degree of preparation achieved before the surgery.7 Jākobsone et al., in his study concluded that relapse of Class III surgical patients was present within the first 6 months after the surgery and that if there was a skeletal relapse, a dentoalveolar compensation was possible.10
CONCLUSIONSThe establishment of common goals between the maxillofacial surgeon and the orthodontist before a surgical-orthodontic case is crucial to achieve favorable results for the patient.
Additional use of a bi-maxillary night retainer must be indicated to prevent relapse since the patient's muscles need to adapt to the new functional demands.
It is of the utmost importance to have open communication with the patient, explaining clearly the diagnosis, treatment plan, surgery and the expected results; in this way the patient will be psychologically prepared to accept the pre- and postsurgical facial changes, which are generally very radical (Figure 12).
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia