Adenomatoid odontogenic tumor is a hamartomous benign neoplasia of odontogenic origin. It appears mostly in young patients and females, the maxillary region being the most affected. It is a slow-growing, asymptomatic lesion. It is related to non-erupted teeth, mainly canines. Lesions of this type can be clinically classified as a follicular, extra follicular and peripheral lesions. Treatment for these lesions is enucleation and curettage of affected area. No recurrence has been observed.
El tumor odontogénico adenomatoide es una neoplasia de tipo benigno hamartomatosa de origen odontogénico, se presenta en pacientes jóvenes, siendo el género femenino y la región maxilar los más afectados, de crecimiento lento, asintomáticos, se relacionan a órganos dentarios no erupcionados principalmente el canino, clínicamente se clasifica como: folicular, extrafolicular y periférico, el tratamiento para esta lesión es la enucleación y curetaje de la zona afectada sin observarse recidiva.
Adenomatoid odontogenic tumors are considered, rather than a neoplasia, a benign, hamartomatous epithelial lesion of odontogenic origin. Steensland first described it in 1905; he considered it as a variation of ameloblastoma.1 Stafne, in 1948 described it as an «ameloblastic adenomatoid tumor or adenoameloblastoma»,2 since it presented structures which simulated canals or glands, he therefore described it as an ameloblastoma variant. In 1915 Harbitz referred to it as cystic adantamatoma. In 1969 Philipsen and Birn proposed the current name: adenomatoid odontogenic tumor (AOT). This name was accepted by the World Health Organization (WHO) in 1971. Nevertheless, in 2005 WHO defined the histological type of the adenomatoid odontogenic tumor and defined it as a tumor composed of odontogenic epithelium with a variety of histological patterns within a stroma of mature connective tissue.3
EPIDEMIOLOGYAdenomatoid odontogenic tumors represent 3 to 7% of all odontogenic tumors. Only about 750 cases have been reported in scientific literature. Even though there is evidence that tumor cells originate from the epithelium of the tooth's enamel, it has been suggested that this lesion originates from dental lamina remnants. Adenomatoid odontogenic tumors are limited to young patients, two thirds of all cases are diagnosed in 10-19 year old patients. This lesion frequently has its onset at the anterior section of upper and lower jaws and is related to non-erupted canines. Female patients are twice over affected when compared to male patients.4
Adenomatoid odontogenic tumors present three clinical variants; follicular, extra-follicular and peripheral. The follicular type is characterized by being intra-osseous and associated to a non-erupted tooth. Due to its radiographic characteristics, it is oftentimes confused with dentigerous cysts, since there is presence of a well-defined radio-lucid area surrounding root and crown of a non-erupted tooth. The extra-follicular type is characterized by being intra-osseous, and unrelated to a non-erupted tooth. The peripheral type is extra-osseous, and appears as an increase in gingival soft tissue volume.5 Most tumors of this type present various inductive changes in connective tissue, such as small calcification areas as well as areas with eosinophilic content.6 According to Philipsen, the AOT extra-follicular type can be found in four different locations: intra-osseous and unrelated to retained teeth, intra-radicular, periapical and in the middle third of the root. Follicular and extra-follicular variants occur in 97% of all AOT cases, and 73% of this total are of the follicular type.7–9
CLINICAL CHARACTERISTICSAdenomatoid odontogenic tumors appear as an asymptomatic, slow-growth volume increase in edentulous areas related to a non erupted tooth (canine), in the gingival region of upper or lower jaws of patients aged 8-19 years.10–13
RADIOGRAPHIC FINDINGSRadiographically, these lesions are similar to other lesions of odontogenic origin. Nevertheless, these characteristics depend on tumor type. In the follicular type, they appear as a well defined and circumscribed area which is associated to the crown or root of an impacted tooth. In the extra-follicular type, the observed lesion is located between or over the roots of an erupted tooth. In the peripheral type, thinning or resorption of the cortical cortex can be observed, as well as in some cases, tooth displacement without causing root resorption.14 Nevertheless, in periapical lesions, radio-opacities have been observed within the lesion up to a 78%, this represents an advantage when compared to orthopantomography.15
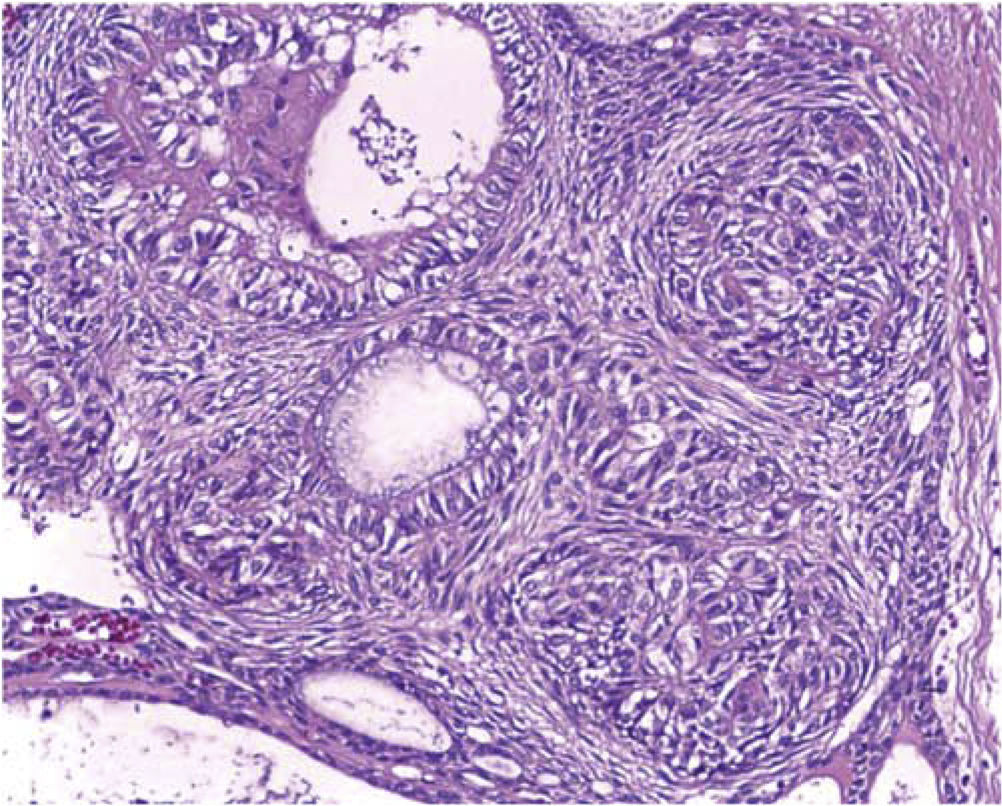
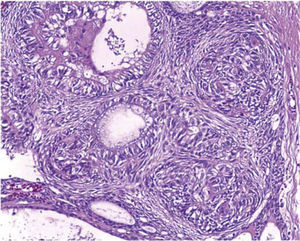
MICROSCOPIC CHARACTERISTICSAOT is composed by solid nodules of epithelial, fusiform or cuboidal cells which form a cluster, as well as characteristics of duct-like spaces and epithelial bands with cancellous or cribiform configuration. The lesion contains an accumulation of inter-cellular eosinophilic material as well as varied amounts of calcified material. Immuno-histochemical studies conducted in AOT lesions showed that they were positive to Pan AE1/AE3, 34β12, CK5, CK14, CK19. CK14 expression and AOT structural aspects tend to support the probable origin of enamel-reduced epithelium. This could explain its frequent association with the crown of an impacted tooth, bearing similarities to a dentigerous cyst.16
TREATMENTAOT cases, due to their non-invasive characteristics and slow growth as well as the presence of a capsule, respond satisfactorily to a conservative treatment consisting on enucleation and curettage. No recurrence has been observed.9,12,17,18
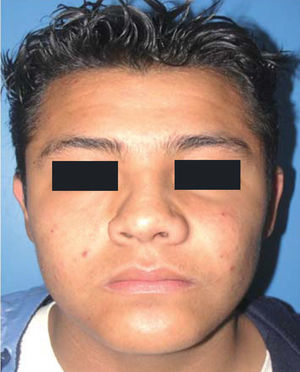
CASE REPORTA 13 year old male patient attended the Maxillofacial Surgery Service of the «Lic. Adolfo Lopez Mateos» Regional Hospital (ISSSTE) (Institute for the Social Security of Government Employees in Mexico). The reason for the visit was increase of volume at the left genian region. The lesion was slowgrowing, asymptomatic, indurated, non-movable, of approximately five month evolution (Figure 1).
Clinically, the following could be observed: full dentition with presence of primary left upper canine, no history of facial or dental trauma or infectious processes associated to the involved area (Figure 2).
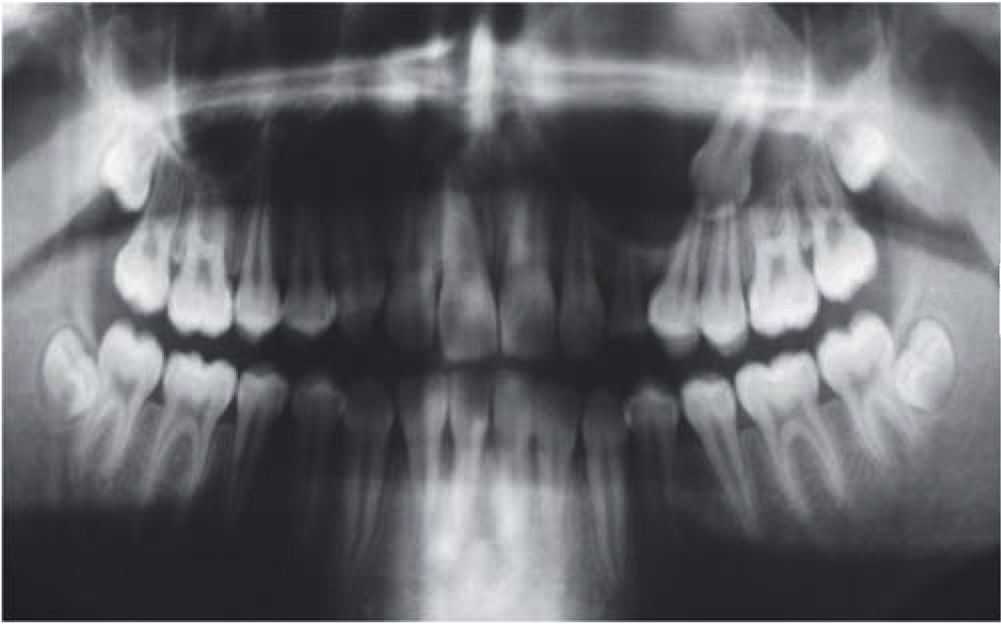
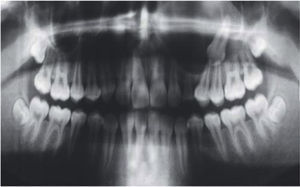
An orthopantomography was taken; it revealed an even-bordered, well-circumscribed radio-lucid lesion in the area of the left maxillary sinus, with the presence of an impacted tooth corresponding to the permanent left upper canine, with absence of data related to dental movement or evidence of toot resorption (Figure 3).
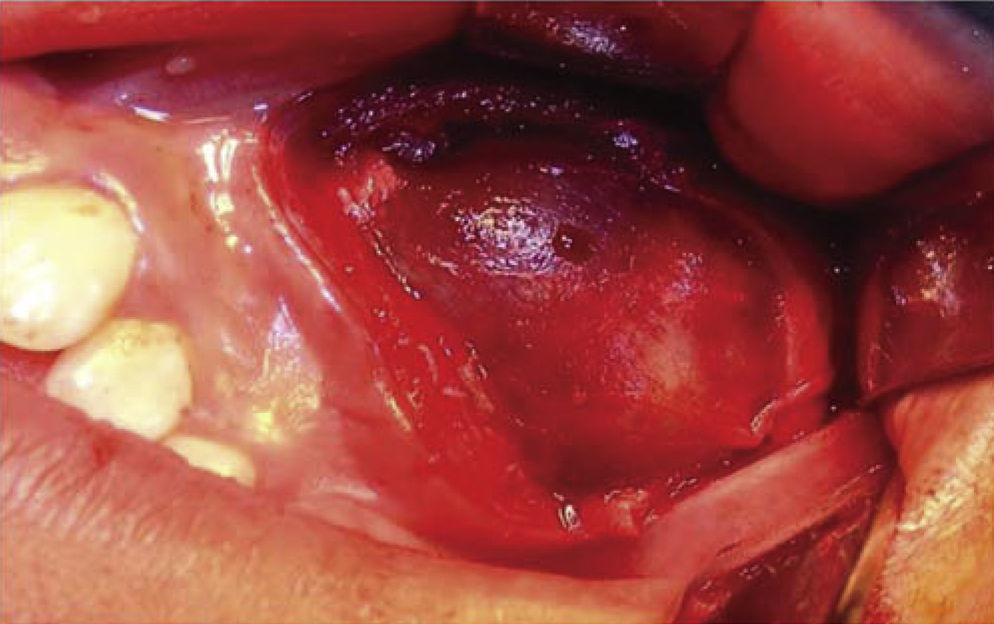
SURGICAL PROCEDUREThe patient was subjected to balanced inhalational general anesthesia, with buccal-tracheal intubation. Previously asepsis and antisepsis of facial region had been executed with povidone-iodine, Pharyngeal blockage and sterile drapes were placed. Xylocaine with 2% epinephrine was administered at the level of the left infra-orbital nerve. With scalpel blade number 15, a semi-lunar incision was made in apical location with respect to teeth 22, 63, 24, 25. Periosteum was removed and a muco-perisoteal flap was raised which revealed an non-perforated wall of the maxillary sinus anterior wall. Thinning of the vestibular cortical zone was observed, therefore, ostectomies were performed in order to expose the tumor (Figure 4). Upon palpation, the tumor was firm, immovable and well circumscribed, it took up the whole maxillary sinus. With blunt dissection, full enucleation was completed. The upper left canine was found within the tumor. After this, the maxillary sinus was subjected to curettage and was cleansed with 0.9% physiological solution. Wound border matching was undertaken with 3-0 polyglycolic acid suture. In that situation, it was decided to preserve the primary canine so it would take the permanent canine's position. The pharyngeal blockage was then removed, and the procedure was completed with no further complications (Figure 5).
Histopathological report was as follows: odontogenic lineage lesion composed of a thick wall of lax, well vascularized fibrous tissue, with recent and previous hemorrhage zone, fully lined with cuboidal-like epithelium, forming duct-like structures filled with amorphous basophilic material and surrounded by a layer of cuboidal and fusiform cells. Within these cells hyaline eosinophilic material focus was observed as well as dystrophic mineralization foci. All the aforementioned characteristics were compatible with follicular-type adenomatoid odontogenic tumor (Figure 6).
Radiographic control was followed during one year and three months. During this time, no recurrence of lesion was observed. Left upper teeth clinically presented vitality and no displacement as well as lack of nerve involvement in the operated area. Permanence of primary dentition canine was equally observed (Figure 7).
DISCUSSIONPhilipsen in 20027 undertook to report the variant of the follicular adenomatoid odontogenic tumor, this has facilitated diagnosis establishment, since it is now related to lesion location. Nevertheless, radiographic interpretation is of the utmost importance, since this study can be considered the basis from where images can be observed, which could otherwise be confused with similar images of dentigerous cysts, calcifying odontogenic cyst, calcifying odontogenic tumor, globulo-maxillary cyst, ameloblastoma, or keratinizing odontogenic tumor. Some reports suggest the fact that in periapical X-rays it is possible to visualize radio-opaque areas within the tumor. This can be an important means to establish a differential diagnosis of this lesion. Nevertheless, all the following factors provide important assistance to establish differential diagnosis: comprehensive clinical assessment of patient as well as frequency, relationship to non-erupted teeth, mainly upper canine, slow asymptomatic growth, with no history of contusion or infection in the affected area, as well as its size, which generally does not exceed 3mm.2,7–9,12–14
Peripheral crown radio-lucid images found in upper or lower jaws are more common than they appear. AOT exhibits a radio-lucid image which is limited to the non-erupted tooth enamel-dentin junction, at the anterior segment of the upper jaw. Notwithstanding the fact that rare cases of this disease have been reported in the lower jaw, canines are the teeth most affected by this condition.14
CONCLUSIONSThe case here presented matched characteristics of all AOT reports published up to this date. Within these characteristics we can mention: age range (first and second decades of life), anatomical zone (anterior segment of the upper jaw), tooth impaction (permanent canine), slow growth, lack of root resorption and asymptomatic teeth. Scarce recurrence after enucleation and curettage was observed. Due to all the aforementioned reasons, suitable diagnosis could be emitted to later perform successful treatment.