Maxillofacial Prosthesis studies comprehend two main branches: oral and facial. In the mouth, some defects caused by unilateral or bilateral maxillectomies performed as part of head and neck cancer treatment, leave structural, functional and psychological sequels. This gives rise to the need of a comprehensive prosthetic rehabilitation. To this end, palate prostheses are used, which offer patients’ reinsertion into society as well as better quality of life. In the present clinical case, the shutter was placed in a situation of complete absence of the maxilla, achieving thus function re-establishment and acceptable aesthetics.
La prótesis maxilofacial estudia dos importantes ramas; la bucal y la facial. En relación a la bucal, algunos defectos originados por maxilectomías unilaterales o bilaterales ya sean parciales o totales en el tratamiento del cáncer de cabeza y cuello; dejan secuelas estructurales, funcionales y psicológicas; estableciendo así la necesidad de una rehabilitación protésica integral; para lo cual son utilizadas las prótesis obturadoras de paladar, que ofrecen así al paciente su reintegración a la sociedad con una mejor calidad de vida. En el presente caso clínico, el obturador es colocado en ausencia completa de maxilar, obteniendo como resultados el restablecimiento de las funciones y estética aceptables.
In Mexico, cancer represents a public health problem. This is due to the severe clinical manifestations of the disease, its high mortality rate as well as the variety of associated environmental and individual factors such as ionizing radiation (UV Rays), occupational radiations (X rays), irritants (soldering fumes, ozone, acids, maladjusted prostheses) pneumoconiotic particles (asbestos1,2 and silicosis) allergens (natural or synthetic) carcinogens (benign or malign caused by arsenical insecticides, sawdust, asbestos, vinyl chloride, aromatic amines, etc) lifestyle (tobacco use, alcoholism, human papilloma virus, poor hygiene),3,4 genetic factors: (mutations of gene p53, of chromosome 9p21, mutation of gene RB)5,6 or related to hereditary cancer syndromes (Plummer Vinson)4,7 which increase the degree of the aforementioned risk.8,9 They are related to the following factors: increase of older people in the world, decrease of death cases due to communicable diseases, as well as mortality caused by cardio-vascular disease in some countries as well as increase in cancer modalities9 which affect patient susceptibility, even more so in cases when they present some degree of malnutrition (30-50%). In these cases, tumor recurrence might be a factor to consider.8,10,11
In Mexico, head and neck cancer represents 17.6% of the total malignant neoplasia cases reported by the Histopathological Record of Neoplasia in Mexico (HRNM) in 2002, where 12% corresponded to Upper Aero-digestive Tract (UADT). Out of this, oral cancer represented 37% with a 62.4% mortality rate.9,12
85 to 90% of UADT cancer cases are due to tobacco exposition. Risk is proportional to exposition intensity. According to INEGI it is an increasing circumstance. It has been reported that 12-17 year old youngsters have increased consumption patterns.9,12
Alcohol consumption is another important associated factor. It produces synergism. Whilst a heavy smoker or drinker increases risk in direct proportion to consumption, those who smoke and drink increase risk 35 times over.9
Squamous cell carcinoma is the most frequent oral neoplasia in Mexico. It is found at a risk factor of 1.4% in males and 0.9 in females in the head and neck area. In 0.02% of all cases it is found in the palate in males, and 0.009% in females, in a 1.7:1.2 relationship respectively, in 2007.12 At the «20 de Noviembre» National Medical Center, a study was conducted in 2009, in it, a 2:1 male-female relationship was reported. After treatment 46.9% recurrence was observed, 32.2% metastasis and 22.45% mortality.13
General frequency of ganglion metastases ranges between 10 and 40%, few distanced metastases were reported. In the hard palate and retromolar trigone, tumors are normally detected at an early stage since they elicit bleeding and pain in the palate.14
According to the tumors’ histological type, etiological factors and location, epidemiological characteristics symptomatology, progression, therapeutics and prognosis will be modified.4 Squamous cell carcinoma is a malignant neoplasia originating from squamous cells; it represents 92% of all oral cavity neoplasia, it is followed by basal cell carcinoma and melanoma.13,15,16 It is placed in 12th place of all malignant neoplasia in the whole world. It mainly affects patients in their seventh decade of life, with average age of 68 years.13 This head and neck carcinoma is most frequent in older men, nevertheless, an increase in young people and women has been reported, as well as in pregnant women.17 It can have its onset as a leukoplakia (2-4% invasive) or erythroplasia (80% invasive) in high-risk zones such as floor of the mouth, ventro-lateral side of the tongue soft palate and palatal velum.18 Different locations of the tumor will elicit different behavior patterns and prognoses, which in turn will require different treatment plans.14,19
Reaction to different types of treatment modify prosthetic rehabilitation times during procedure and after it. These treatments can be adjuvant or concomitant (chemotherapy, radiotherapy, surgery), they are alternative treatments and increase organ preservation, improving thus treatment success.8
Chemotherapy consists on anti-neoplastic drug administration to induce tumor cell destruction though the hindering of cell division. Most used drugs for head and neck treatment are: bleomycin, cisplatin, methotrexate, 5 fluorouracil, vinblastine, cyclophosphamide, carboplatin, gefinitib, erbitux, and cetuximab.20–22 Certain anti-neoplastic drugs can cause long-term lesions in the hematopoietic system.23 It can be curative (total tumor control), adjuvant (after surgery, decreasing the risk of metastasis), previous (partial tumor reduction to complement surgery or radiotherapy) and palliative (improving patient's quality of life).14,20 Knowledge of HPV (human papilloma virus) is becoming an important consideration to observe when assessing treatment for patients with head and neck cancer. Patients who are HPV-positive respond better to treatment, Current research is targeting to stratify patients according to their HPV status in clinical trials.21
Ionizing-radiation radiotherapy either destroys cancer cells or decreases their growth. This is a common treatment for head and neck cancer cases, it is used for approximately 50% of all cancer treatments in this area; it can be used by itself, or combined with chemotherapy and/or surgery.14,20 It can cause oral complications such as mucositis, bacterial or fungal infections, salivary gland dysfunction, fibrosis, dental caries, dysfunction of sense of taste or osteo-radionecroses.14,19,22
Surgical treatment of head and neck involves a series of functional repercussions of the anatomical structures affected by the tumor. This can appear in neck and scapular region mobility, alterations in healing and lymphatic drainage, as well as deglutition, which would then warrant extirpation surgery of tumor resection and/or lymphatic surgery of tumor-affected areas.19
Therefore, sequels originated from surgical treatment in the bucco-antral area are caused by maxillectomies (limited, partial, medial subtotal, total radical or extended).24 These sequels can be structural (bucal-antral communication)3,24 functional (breathing, mastication, deglutition, phonation) and psychological.3
Aramany undertook to classify maxillary defects based upon the defect area and remaining teeth25 Classifications I, II and IV (lateral defects with anterior margins close to the midline) are the most frequent.26 It is therefore of the utmost importance to consider that full, wide defects of the soft and hard palate are not considered within this classification (when in the soft palate, they are rather considered hereditary defects).26 Kan-ichi Seto did mention it in 2003 (HS classification), and referred to it as H6SODxT3 (full defect without soft palate involvement, impossible to determine oral opening degree and with no tooth presence).3 It takes into account the fact that not only the upper jaw is involved; hard palate and para-nasal sinuses are equally involved, and due to the loss of support experienced by the upper jaw, there is development of enophthalmos and diplopia.27
Maxillofacial rehabilitation of head and neck cancer patients demands knowledge of the disease, type of resection, margins and post-treatment.7,28–30 The field of reconstructive surgery has seen great advances with techniques of epithelial, muscle and bone grafts, which target prosthesis support.7,28,30 Prosthetic rehabilitation encompasses the palatal shutter (obturator)which offers modifications to full prosthodontics.3,4,28 This techniques takes into consideration defect volume, remaining hard and soft tissues, quality of the mucosa as well as stability and retention of the appliance. All the aforementioned factors will determine the appliance's design. Other factors to be equally considered are: patient's experience with dentures, neuromuscular control and previous therapeutic history (radiotherapy, chemotherapy, surgery).24,27
The palatal shutter is a prosthesis used to close a congenital or acquired opening, preserving the integrity of oral and nasal compartments. It facilitates speech, deglutition and mastication, either in provisional or final surgical stages.3,31
Severe cases require rigid obturator extension towards soft tissue areas. This complicates rehabilitation, since it no longer requires only the aforementioned characteristics, it also requires obturator seal on mobile, free margins. Thus, boneintegrated implants (including mini-implants and zygomatic implants) have been considered as those implants providing most retention and requiring sometimes bone distraction. Reaction of bone tissue to implant insertion must be taken into account (boneimplant bonding), cleansing and preparation of implant surface, as well as bone type (area to receive implant) and implant type.27,32–34
When following this therapeutic approach, patient risk factors such as age, medical circumstances, psycho-social circumstances, habits, presence of osteoporosis, periodontitis or cancer, must35 be taken into consideration. Patients must be referred to special preventive programs. This will bear influence in treatment success or failure.
Bone distraction is a process triggered by application of planned and controlled tension on a corticotomy or osteotomy. This process allows for bone neo-formation and elongation based on a bony callus. This elongation is transmitted to soft tissues, it induces their gradual and continuous growth. It develops in four phases: osteotomy, latency, distraction and consolidation.32,36 It has been shown to be safe and effective, generating histiogenic distraction (masticatory muscles, subcutaneous tissue and skin).36
Use of mini-implants (MDI) is recommended for patients who lack sufficient bone structure to place implants smaller than 3.75mm. These implants have a 1.8mm diameter. Their use provides advantages such as lesser bleeding and lesser post-operative discomfort, faster healing (due to diminished surgical maneuvers) lesser bone loss when compared to the traditional method. In addition to the aforementioned, these implants are of much lower cost. They were first provisionally used for immediate load, along with conventional implants, so as to be retention means of immediate prostheses, and prevent premature loads on the bone and thus avoid compromising final implants. Previous studies report their success as being between 92% and 97%, according to number and surgical zone.37
Since 1990, zygomatic implants created and developed by Dr Branemark have been used as posterior anchorage for implant-supported dentures in patients with severe maxillary atrophy. These implants are indicated in cases of severe maxillary resorption or in patients afflicted with full upper edentulism. Their use eliminates the need for bone grafts or maxillary sinus lifting. They are introduced into the zygomatic bone, and can be joined by other conventional implants in the upper jaw's anterior area, in which place there is normally remaining bone. After implant placement, a provisional denture can be placed. 4 to 6 months must be left to elapse in order to achieve implant boneintegration and then place a final denture.32,38–40
CLINICAL CASE PRESENTATION69 year old male patient, born and residing in Mexico City. The patient reported he had a commonlaw wife, was catholic and a taxi driver. In 1992, at the Mexico's National Cancer Institute, he was diagnosed with non-differentiated squamous cell carcinoma in the hard palate. Approximate tumor size was 1 x 2 x 1.5. The patient suffered hypertension, gastritis and Type II diabetes. He was under medical treatment (acquired after chemotherapy treatment). The patient equally informed he was a two-pack a day cigarette smoker as well as an alcohol drinker.
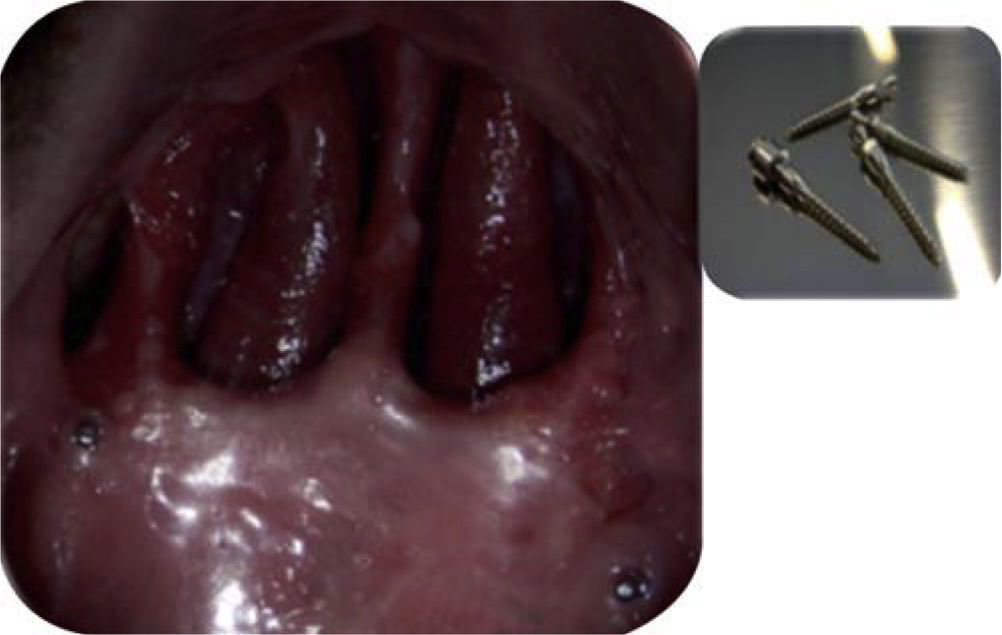
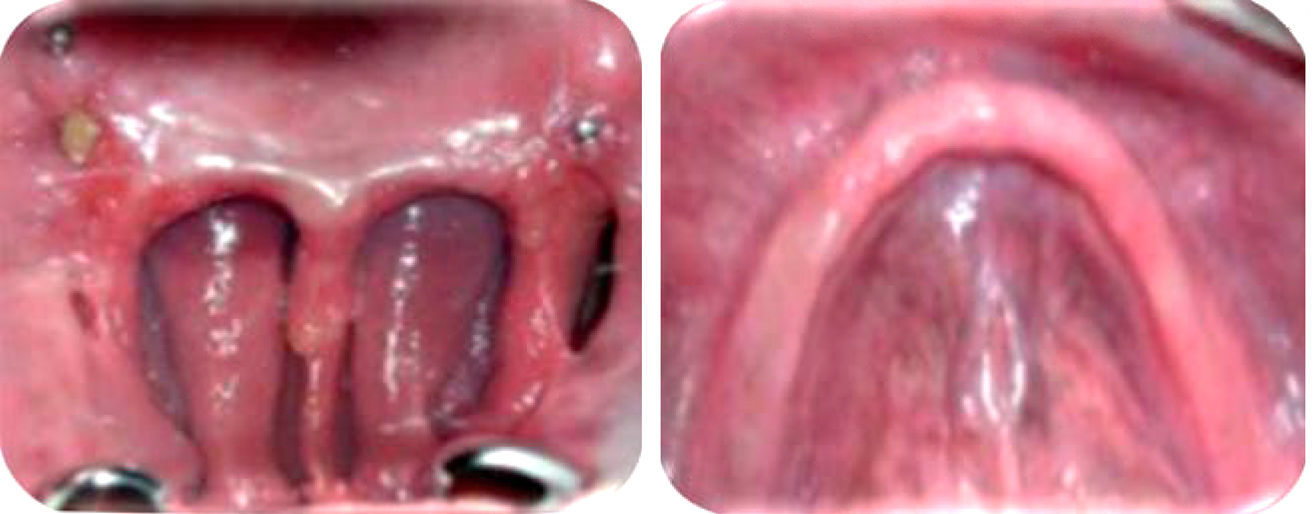
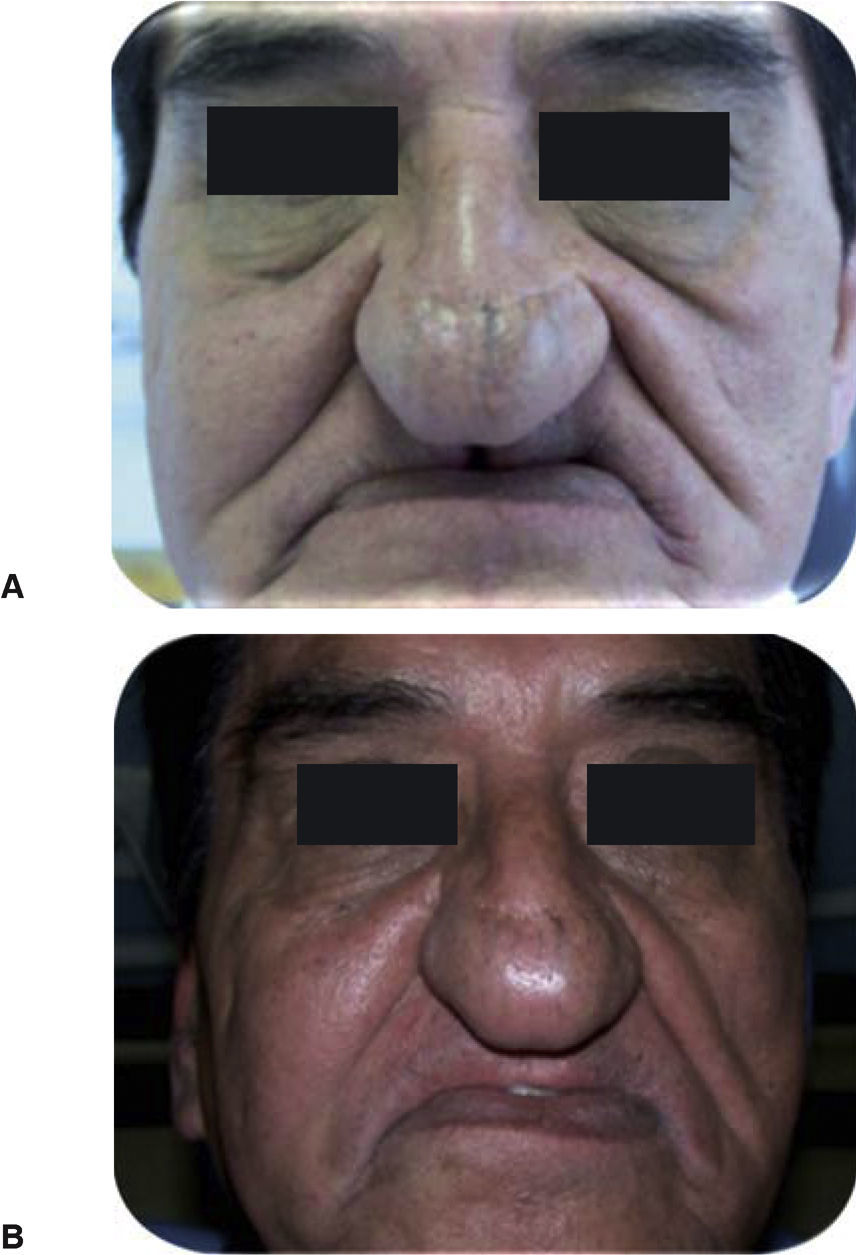
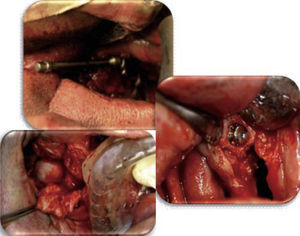
After diagnosis was established, the patient informed he had been subjected for 5 years to chemotherapy with Cis platinum and 5FU. Results were favorable inasmuch as avoiding tumor growth and preventing metastasis. After the aforementioned treatment, the patient suffered tumor recurrence at the same location. This new tumor spanned into the whole upper jaw. Therefore, surgery was deemed necessary. Surgery was total bilateral maxillectomy with radical neck resection. Surgery sequels were facial collapse of the face's middle third. The patient was not subjected to post-operative radiotherapy (Figure 1).
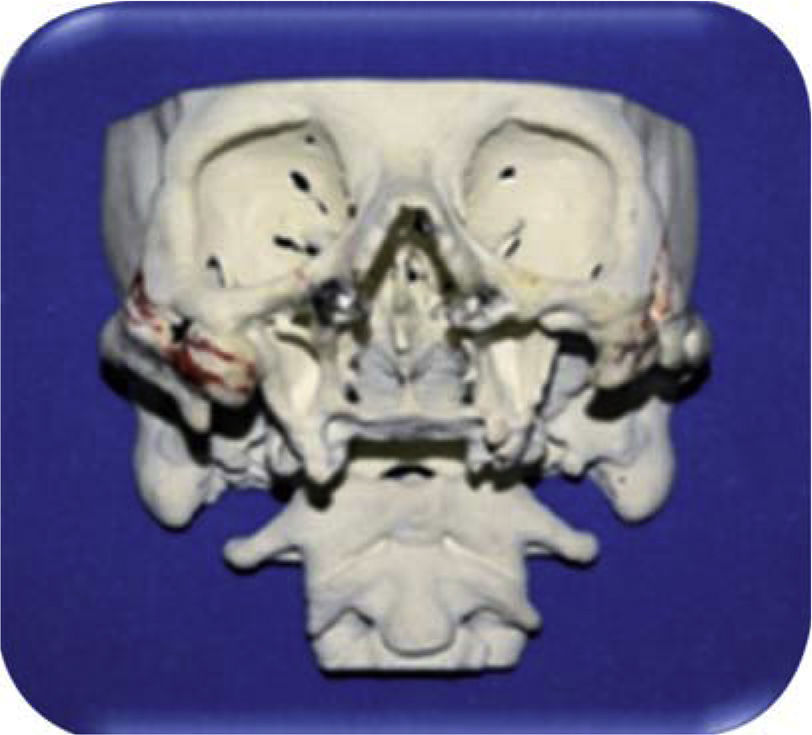
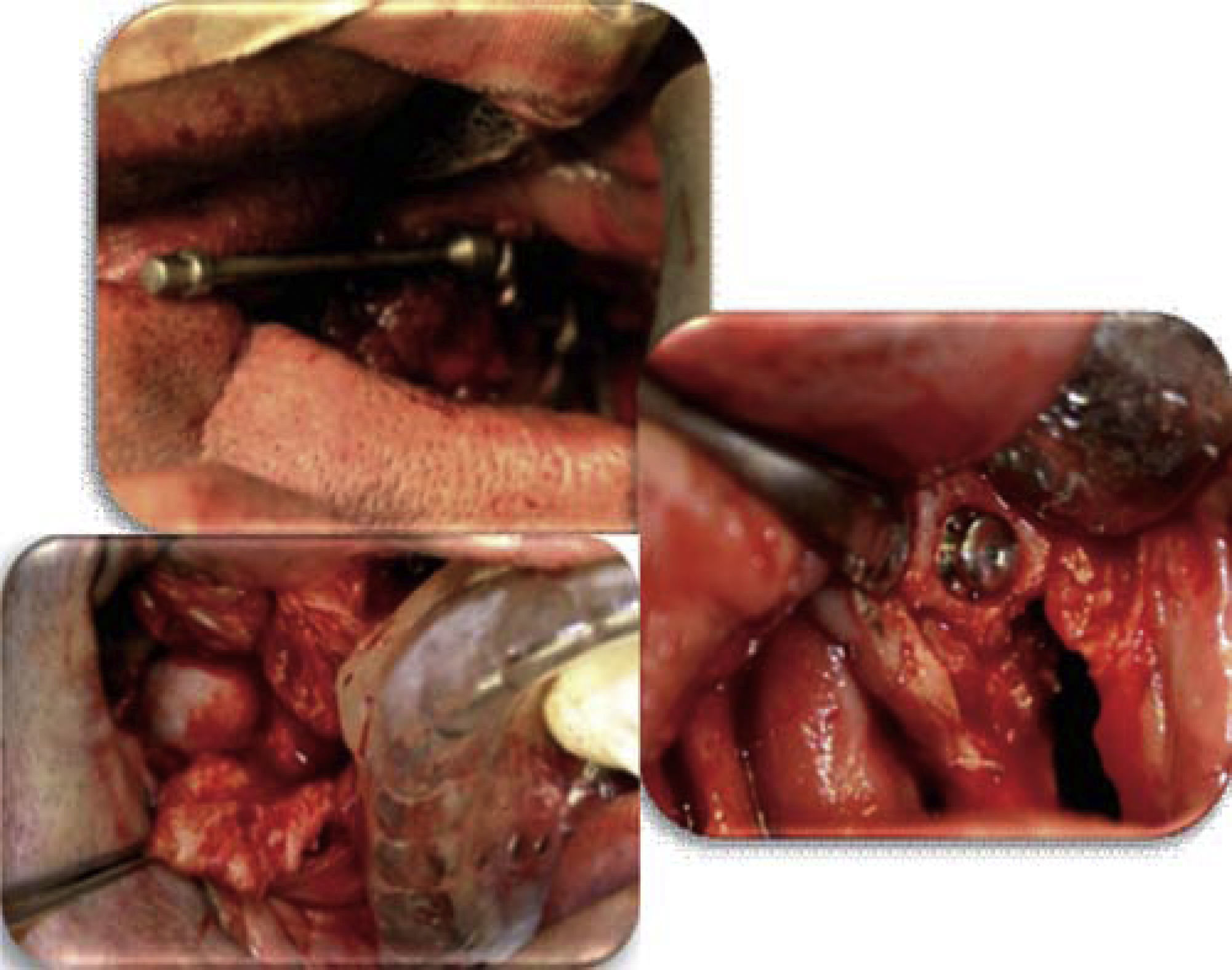
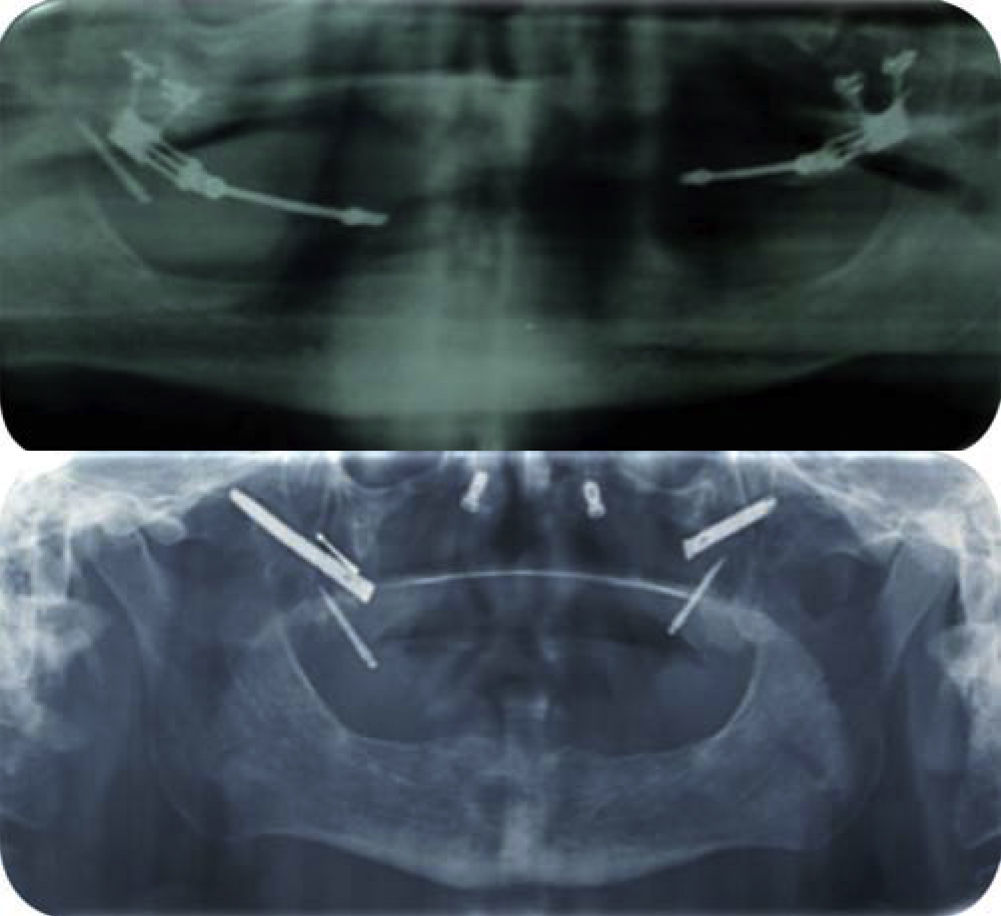
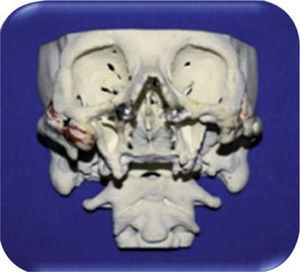
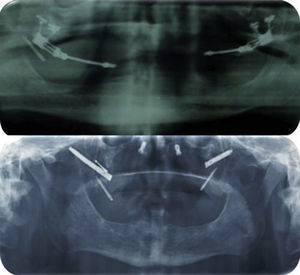
Since rehabilitation was complex, several treatment forms were analyzed (taking into account the fact that the patient had not received radiotherapy). Considered treatment options were: placement of 4 mini-implants (2 in the posterior zone and 2 in the anterior zone). With the help of stereolythography, ideal implant location was planned in order to achieve a surgical guide (Figures 2 and 3).
Manufactured dentures presented insufficient initial stability and retention. With time, the upper denture required greater functionality and esthetics in concordance with changes and requirements of remaining tissue, therefore, present retention was no longer sufficient (Figure 4).
It was decided to place bone distractors, so as to obtain an area of greater support, to later place zygomatic implants. The multi-disciplinary team conducted a previous coordinated analysis of the case targeting the remodeling of that area in order to achieve greater support and stability of the final obturator (Figures 5 and 6).
Unfortunately, due to bone insufficiency, the implanted zone rejected the implants, even though indicated bone-integration time was observed (between 4 and 6 months) as well as healing period, prevention and infection control.
Taking into account bone response to implants it was decided to build modified full dentures. Upon assessing the defect, it was observed there were two posterior mini-implants which afforded some support to the denture, nevertheless, they failed to prevent denture displacement mainly during mastication and phonation procedures. Patient comfort and esthetics were also compromised (Figure 7).
METHODOLOGY- 1.
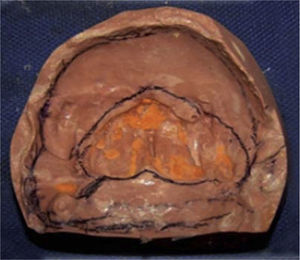
Anatomical impression of the defect was taken. Rapid-setting alginate was used. The material was handled according to manufacturer s instructions. Lower arch impression was equally taken (Figure 8).
- 2.
Positive models of both arches were taken with type III hard plaster (Figure 9).
- 3.
Individual trays were manufactured. Borders were later rectified with type II stick modeling paste material. Defects of border as well as lower arch were recorded.
- 4.
Once the borders were rectified, physiological impression was taken with polysulfide rubber. Impression of upper defect was first taken, followed by impression of the lower arch (Figure 10).
- 5.
Impressions were contoured in order to obtain type IV plaster working models (Figure 11).
- 6.
Working models were trimmed, recording bases were recorded with relationship rollers, so as to later undertake prosthetic, phonetic and esthetics tests.
- 7.
After establishing cranio-mandibular relationships, plastic braces were taken to proceed to model transfer to a semi-adjustable articulator.
- 8.
Once the models were transferred. Teeth were selected according to established principles, so as to place them and later balance them.
- 9.
Dentures were tested in the mouth (Figure 12).
- 10.
Obturator and lower denture were manufactured following the lost wax casting technique. The obturator was hollowed out so as to make it lighter.
- 11.
Dentures were processed with heat-cured acrylic, which was processed according to manufacturer's instructions.
- 12.
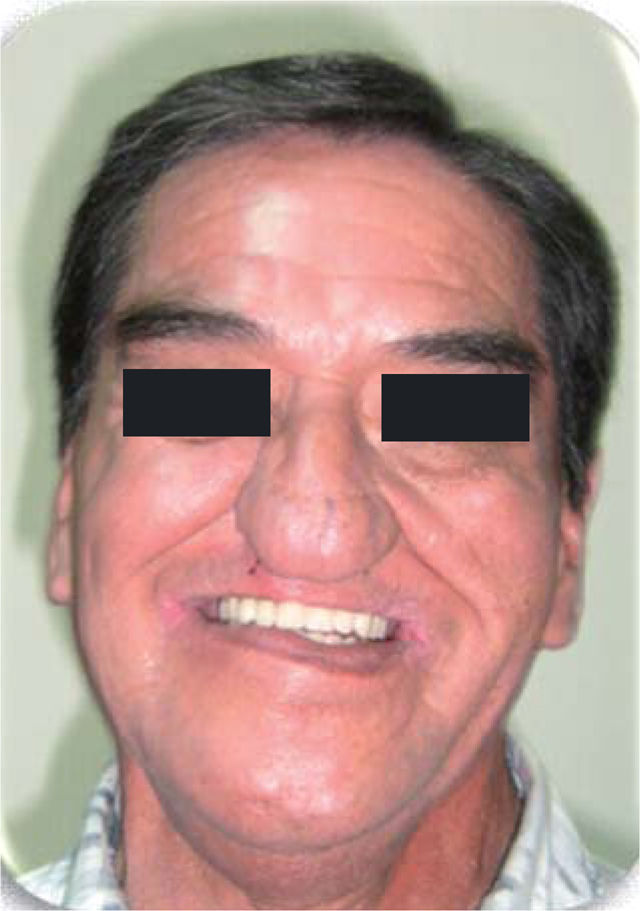
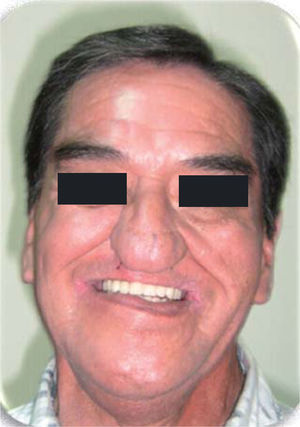
Finally, dentures were retrieved from the muffles in order to be trimmed, polished and placed in the patient (Figures 13 and 15).
- 13.
Patient was instructed on denture use and preservation, as well as to the need of recurrent visits to assess denture adaptation.
The obturator was built in concordance with basic principles of full denture construction. Modifications were executed in order to obtain better results.
DISCUSSIONSquamous cell carcinoma is one of the most frequent malignant neoplasia found in the world. In concordance with numerous authors9,12–14,16–18 we observed that simultaneous smoking and drinking increases the risk of contracting oral cancer.
Therefore, satisfactory prosthetic rehabilitation requires multi-disciplinary efforts in order to achieve suitable functional adaptation24 in view of the complexity of diagnosis, therapies and rehabilitation of head and neck cancer patients.28 In cases when the maxillary defect is not surgically reconstructed, a surgical obturator would be recommended to seal the defect, since it will support the surgical site and restore oral function.27
It is important to note the fact that obturator prostheses have been widely modified, since the essential foundation of a full prosthesis is based on the residual ridge and in this case there was no ridge. Classifications such as that of Aramany do not include total loss of the jaw. Kan-ichi Seto did mention it, but did not explain how to rehabilitate a patient with this type of defect.3,25 Ortegon et al (2008) and Cheng et al(2004) do mention it with different techniques.24,27
Thus, retention of a bilateral full obturator can be supported following several methods such as (1) remaining structures of the upper jaw along with the posterior third of the soft palate, (2) supporting the obturator on a healed lateral band, (3) extending extra-orally the prosthesis towards the nostrils and (4) based on bone-integrated implants.24,32
In the present report, obturator manufacture involved two stages: 1) Manufacture of obturator and lower denture, 2) at the moment of being processed, the obturator is emptied using heat-curing acrylic. In situations when the defect is more complex, the obturator must be manufactured in segments.27
During the manufacture of these obturator prostheses, it must be taken into account that there will be modifications and alterations in clinical and laboratory treatments, such as: 1) During manufacturing of provisional prosthesis, 2) during bulb manufacture in the final prosthesis, 3) upper and lower jaw relationship and 4) insertion of final prosthesis, where wide maxillary defects might compromise denture functionality.27
Therefore, a suitable treatment plan for such a wide defect always will require patient pre-surgical acceptance. The patient will be in the hands of a team formed by surgeons, maxillofacial prosthetic specialists, phoniatricians, nutritionists and psychologists.27
It is equally important to note that success of a prosthetic rehabilitation will depend 50% on the physician and 50% on the patient (before, during and after treatment).
Finally restoration was achieved as far as possible, impacting deglutition, speech, mastication, esthetic appearance as well as patient's psychological welfare; which will in turn impact on patient's comfort, and security which are necessary to reinsert the patient into society affording thus suitable quality of life.24,27
CONCLUSIONSThe patient informed of a 5-year ongoing chemotherapy history, with late mini-implant placement, bone distraction procedure and placement of zygomatic implants based on stereolitographs. Patient's clinical experience was negative, as a result of existing poor bone quality. It was therefore decided to manufacture a full lower prosthesis and a modified palatal shutter.
When bilateral total maxillectomy was undertaken, prognosis was negative. The patient was fully edentulous in the lower section, therefore, a light, retentive and functional shutter had to be devised, to primarily achieve a barrier between oral and nasal cavities. The shutter provided support and stability, and this, along with a full lower denture, preempted the need to use adhesive material.
The patient experienced suitable defect healing, and was of a positive attitude, this was very important in the process.
We noticed the fact that the modified palatal prosthesis afforded the patient another treatment alternative. The present one was manufactured with acrylic material and met with patient's expectations for improved quality of life.
The patient presently exhibits better adaptation to the palatal shutter. He can now eat, drink liquids and speak better. The restoration is more aesthetic and affords the patient with more self-security to interact in society.