Human papilloma viruses constitute a heterogeneous viral group; their genome is made up of a helicoidal double-stranded DNA molecule with a protein capsid. There are over 230 HPV types (118 of them well characterized; more than 40 are anal-genital types, out of which 15 are oncogenic). In humans they represent one of the viral groups which more frequently infect epithelium of skin and mucosae, conjunctive tissue, oral cavity, larynx, and bronchial tree among others. Oral mucosa squamous papilloma, caused by genotypes 33 and 32, is the most frequently found papillary lesion and represents 2.5% of all lesions of the oral cavity, larynx, bronchial tree, esophagus, bladder anus and genital tract. The aim of the present study was to conduct a literature review on oral papillomatosis as well as to review a clinical case.
Los virus del papiloma humano (VPH) constituyen un grupo viral heterogéneo, cuyo genoma está constituido por ADN de doble cadena helicoidal con una cápside proteica. Existen más de 230 tipos de VPH (118 de ellos bien tipificados), más de 40 tipos anogenitales, de los cuales 15 son oncogénicos y, en humanos, constituyen unos de los grupos virales que con mayor frecuencia infecta el epitelio de piel y mucosas: conjuntivas, cavidad bucal, laringe y árbol bronquial entre otros. El papiloma escamoso de la mucosa oral, ocasionado por los genotipos 33 y 32, es la lesión papilar más frecuente y constituye el 2.5% de todas las lesiones de la cavidad oral, laringe, árbol bronquial, esófago, vejiga, ano y tracto genital. El objetivo del presente estudio es realizar una revisión de la literatura sobre la papilomatosis oral y reportar un caso.
Human papilloma viruses (HPV) conform a heterogeneous viral group; their genome is constituted by a helicoidal double stranded DNA molecule with a protein capsid. They are formed by epitheliotropic entities which infect the epithelium's basal state and, as a result, preserve its DNA transcription and replication at basal levels, producing hyperplastic papillomatous and verrucous lesions in the skin and mucosae.1
There are over 230 HPV types (118 of them well characterized) and over 40 anal-genital types, out of which 15 are oncogenic. In humans, they represent one of the viral groups more frequently infecting epithelium of skin and conjunctive mucosae, oral cavity (genotypes 33 and 32) larynx, bronchial tree, esophagus, bladder, anus and genital tract.2,3
In the case of tongue HPV, there are two main groups of clinical presentation:
a) Benign lesions and b) pre-malignant or malignant lesions. Among benign oral lesions we can find oral papilloma, oral verruca vulgaris (common wart), oral acumina condyloma and focal epithelial hyperplasia (Hecks disease).4–6 Malignant and pre-malignant lesions are mainly represented by leukoplakia and squamous cell carcinoma.7
Squamous papilloma of the oral mucosa is the most frequently found papillary lesion, it represents 2.5% or all lesions found in the mouth.6 HPV clinical lesions are most frequently observed in the upper lip, the lower lip, lingual frenulum, dorsum of the tongue and corners of the lips.8
The most commonly observed morphology of these lesions assumes a cauliflower-like shape, nevertheless, other shapes can be observed such as common warts, hyperkeratosis or even non-keratinized surfaces, which exhibit superficial color changes (normally a violet hue).9 According to bibliographic references, this disease is mostly transmitted through a oral-genital sexual practice.10
The aim of the present study was to conduct a literature review on oral papillomatosis review as well as reporting a clinical case.
HISTOLOGY OF THE TONGUECells located in the tongue exhibit a polystratified structural arrangement. They are settled on a (superficial) stratum corneum, a granular layer, spinous layer and basal layer (deepest layer). The nucleus of these cells changes in size according to their maturity and specialization.11
PAPILLOMA VIRUS GENOMEViral particles are composed of a protein capsid which is composed of 95% protein L1 and 5% protein L2. These proteins link to form icosahedral capsomers. Double-stranded circular DNA of approximately 8000 base pairs can be found inside the capsid. It is formed by eight genes and a non-codified regulatory region; this region contains linking sites for host's hormonal and protein factors, needed by the virus to complete its replication cycle.12
HPV virus is similarly conformed by two types of genes: genes codified during the early infection stages, better known as E genes (E for early) and genes codified during late stages of replication known: E1, E2, E4, E5, E6, E7 (although E4 is considered a late gene) as well as two late genes, L1 and L2. Early genes codify proteins involved in viral replication and regulation, as well as in their carcinogenic capacity. On the other hand, late genes codify structural proteins which form a viral capsid.12,13
HPV CYCLE OF LIFEHPV enters the host through a small abrasion in the tongue's integral epithelium.13 It then initiates its productive cycle infecting poorly differentiated cells of the epithelium's basal layers, where transcription of genes begins.12
When infected cells differentiate and migrate from the basal layer into the epithelium's spinous layer (immunological permissibility), viral replication is stimulated producing thus virion accumulation within the nucleus and the assembly of the capsid in the cytoplasm. There are at least two cycles for viral replication: a) lytic infection and b) lysogenic infection.
In cases of lytic infection, the virus arrives into the para-basal cells with replication ability, it penetrates the cytoplasm and later the nucleus. Once within the nucleus, it replicates in the episomal area, without integrating into the cellular genome, producing thus approximately 20 viral copies. These complete viral particles cause cell death and remain thus free and in proximity to epithelial surfaces.
In cases of lysogenic infection cell genome is directly affected. This is the case of the high risk HPV (16 and 18). After reaching cell nucleus, the virus integrates into the host's cell genome, mainly segments E6 and E7. In this case, virus replication assumes a latency stage until the host cell replicates its own DNA as well as DNA of integrated viruses. Viral DNA segments are transcriptionally active after cell division; this guarantees their propagation13 Unlike lytic infection cases, this type of infection is observed in cells experiencing malignant growth.
Gene expression of different HPV types is strictly and specifically regulated through transcription factors such a AP-1, keratinocyte specific factor, NF-1CTF, CEFI, CEFII and TEFI as well as some hormonal origin factors.
In both types of infection, E1 and E2 proteins initiate their expression in an ascending direction (supraregulation), activating thus DNA transcription as well as basal cells’ controlled expression.12
E6 and E7 HPV genes are directly related to cell malignant transformation through oncoproteins E6 and E7. These proteins are able to form compounds with cellular gene products which regulate cellular cycle, among which p53 and Rb can be found. Oncoprotein E6 creates a compound with p53 protein, whereas E7 creates a compound with Rb protein.
Rb protein regulates the passage from G1 to S Oncoprotein E7 sequesters Rb preventing it from regulating cell proliferation proteins, this forces the cellular cycle to remain in synthesis phase.13 These two events: viral gene integration to cell genome and blocking of normal function of tumor suppressor genes p53 and Rb are associated to cellular transformation of cells infected with high oncogenic potential viruses (16 and 18). Progressive changes experienced by keratocytes modify the microenvironment and alter the epithelium's balance though cellular proliferation stimuli guided by secretion of alpha and beta epidermal growth factors.
Proteins E2, E3, E4, E5, E6 and E7 induce loss of gene protein control (episomal DNA at the nucleus center) while E6 and E7 replicate viral DNA. L1 and L2 assemble the virus and place themselves in mature squamous cells to later slough off (over 1,000 copies per cell).
In benign lesions, such as tongue papilloma, proliferation of episomal DNA particles promotes abnormal epithelium growth, increasing thus gene errors of the cells (gastogenesis).
E6 and E7 promote virus proliferation and immortalization. When the virus possesses oncogenic potential it causes malignization, when it doesn’t, a benign lesion is developed which can self-limit in a two year period. This mechanism is mainly induced by loss of DNA telomeres, which inhibits apoptosis, increases number of infected cells and decreases p53 and Rb acetylation and phosphorylation. Moreover, angiogenic factors expression is promoted. Such is the case of the vascular growth factor which disorganizes cell cytoskeleton and extracellular matrix affecting regulation factors which take part of the health of these structures.12
HPV infection causes important changes in cell morphology. For instance, peri-nuclear vacuoles formation is observed, enlarged, irregular and hyperchromatic nuclei as well as bi-nucleation. Cell which have suffered these changes are called koylocytes and are considered the «fingerprint» of the virus.
Condyloma is the most common morphologic manifestation of HPV infection (condyloma acuminatum).14
CASE PRESENTATIONThe patient was a 21 year old single female. She did not work outside her house, was born and residing in the Estado de Mexico (State of Mexico). Her blood type was O, Rh positive. As part of her family history she reported her father as carrying multiple sclerosis and a sister afflicted with rheumatoid arthritis. The patient denied any drug addiction. She was afflicted with multiple juvenile breast fibroadenoma in the left breast, which were surgically treated. She initiated menarche at 15, with menstrual rhythm 28 × 3. Sexual activity began at 17. She reported one sexually active partner, denied practice of oral-genital sex. She experienced pregnancy and was delivered of a 3.1kg live child.
One year before she had been subjected to cytology and colposcopy studies in the lower genital tract, in addition to breast check-up. Results proved negative for cancer and HPV. Family planning method used by the patient was intrauterine device.
The patient sought consultation for the first time in April 2014, complaining of ventral glossodynia with a three month evolution. After this, she experienced a feeling of foreign body and bulging in the soft tissue, with progressive centrifuge growth until formation of a lentil-shaped tumor which bled when contacting the hard palate and during mastication. She attended a doctor's office where she received non-specified systemic treatment which did not elicit satisfactory results.
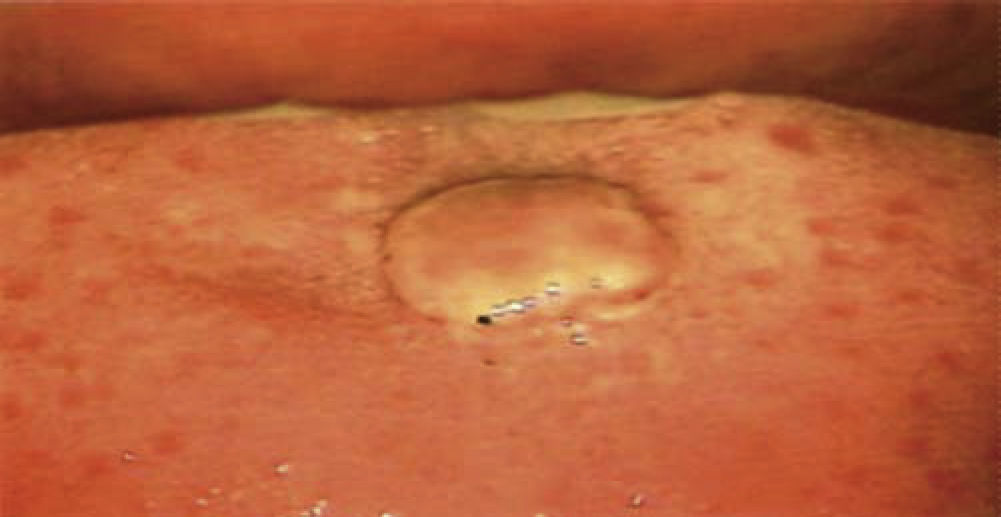
The mouth was inspected through a colposcopy procedure with 0.66x magnification (Hinselmann colposcope, 2014 Mexico). Said procedure revealed a lesion of approximately 1cm diameter, of a pinkish hue, circular shape, with jagged edges, without pedicle and of an avascular nature (Figure 1). Once the study was completed, the patient was informed about diagnosis and desirable treatment.
TREATMENTUnder local anesthesia and 2% xylocaine with epinephrine (1mL) the base of the lesion was infiltrated with a 30G caliber needle. Lesion surface was clipped and dissected undertaking a wedge sharp dissection. After haemostasis was achieved, borders were faced (Dermalon 000) in one plane with inverted sutures. Specimen obtained was fixated in 5ml 10% formalin to then be sent to the Pathology Department.
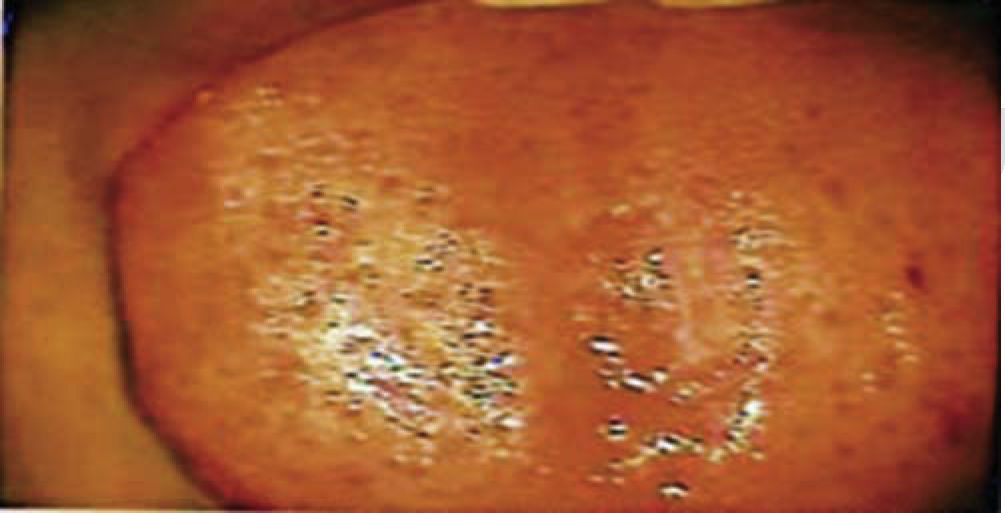
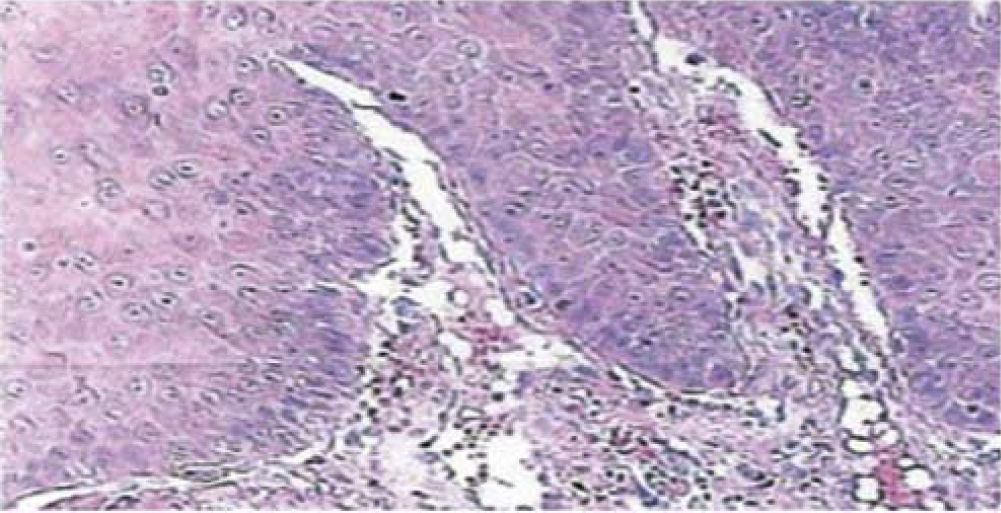
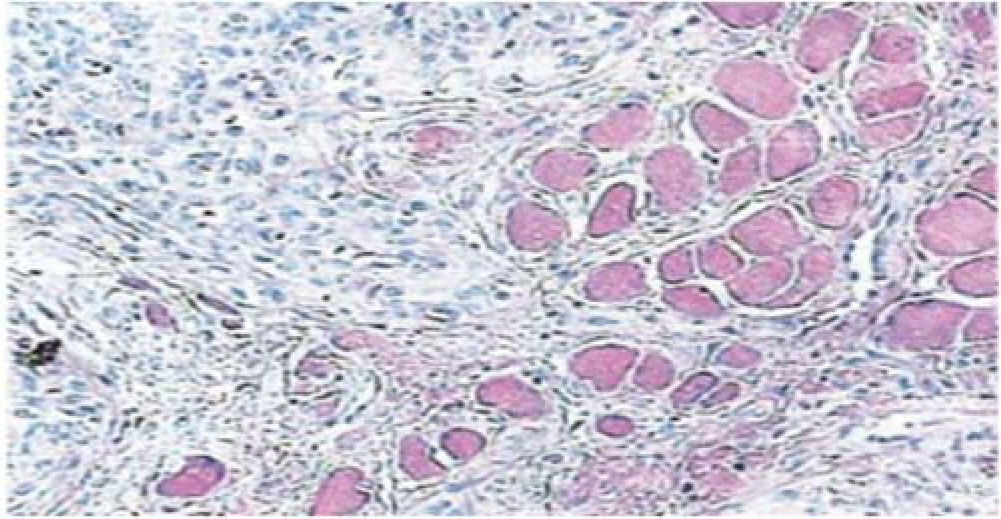
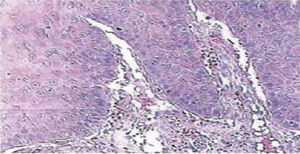
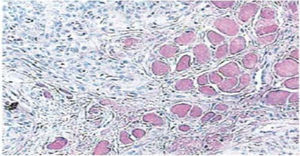
Fifteen days later the sutures were removed and healthy surgical area was thus obtained (Figure 2). Histopathology report revealed presence of tissue with 0.6 × 0.5cm measurements. The specimen was of irregular shape, dark brown hue and soft consistency. Microscope analysis revealed poly-stratified, corneal epithelium, acanthosis and hyperkeratosis. Sample's interior revealed intra-epithelial cornification foci of different sizes. In general, epithelial cells were of a smaller size than those of normal stratum spinosum (Figures 3 and 4). Final diagnosis indicated a squamous papilloma of the tongue. Viral gene-typing conducted with polymerase chain reaction (PCR) in real time reported presence of a 58 genotype (high risk virus).
HPV is a DNA virus; it belongs to the papovaviridae family, of the papillomavirus gender. Over 230 genotypes have been described. Incubation period varies from three weeks to eight months, with a three month average. Out of the 230 papillomavirus genotypes, 16 are most frequently associated to oral lesions (1, 2, 3, 4, 6, 7, 10, 11, 13, 16, 31, 32, 33, 35 and 57).
There are two main groups of HPV clinical presentation: a) benign lesions and b) premalignant or malignant lesions. Benign oral lesions include oral papilloma, verruca vulgaris (common wart), oral acuminatum condiloma and focal epithelial hyperplasia (Heck's disease). Premalignant and malignant lesions are mainly represented by leukoplakia and squamous cell carcinoma associated to genotypes 16 and 18. HPV transmission is conducted through oral-genital sexual practices.
There are several techniques to diagnose HPV, among them we can count conventional cytology, liquid base cytology, histology, colposcopy and molecular biology techniques such as in situ hybridation and polymerase chain reaction (PCR).15,16 In the clinical case here presented it was decided to undertake virus gene-typing with PCR, this procedure revealed presence of a 58 genotype. This datum has not been documented in the classification reported in literature.
Treatment is tailored for each individual case. Destructive techniques can be used, such as cryotherapy or electro-surgery, use of immunemodulators (imiquimod at 5%), or use of an antimetabolite to interfere with RNA (ribo-nucleic acid) and DNA, or through thymidylate synthetase inhibition (5-fluororacil).17,18 In the present case it was decided to use surgery with cold scalpel based on the site of lesion apparition, to avail ourselves to the possibility of not leaving sequels.
CONCLUSIONIn oral mucosa exposed to micro-trauma, microorganisms as well as chemical and physical factors can synergistically act with HPV to propitiate development of benign lesions or carcinoma.
HPV plays an important role in the development of squamous cell carcinoma in anal and genital tracts as well as in verruciform epidermodysplasia, and in the larynx.
In benign lesions, genotypes 33 and 32 are the most frequent. Nevertheless, in our study, report of molecular biology procedure indicated presence of genotype 58.
In worldwide literature 58 gene-typing has not been reported in this type of lesions which clinically appear to exhibit benign behavior.
In order to successfully approach this condition, interdisciplinary diagnosis and treatment among dentists, oncologists and gynecologists suitably trained in the study of these lesions under colposcopic perspective is of the utmost importance.
Treatment executed through surgical intervention with cold scalpel, aiming at leaving lesion-free borders is an adequate solution to eradicate this type of lesions and cause no sequels, especially in tumors which appear to be clinically benign, but which according to their gene-type, will undergo malignant behavior in the medium and long term.
We consider the present case report interesting since there were few reports related to this condition in Mexican scientific bibliography.
Master in Sciences, Specialist in Gynecology and Obstetrics, recertified by the Mexican Board of Gynecology and Obstetrics, Professor of Genital Tract and Anal-Perineal Complex Pathology (UNAM) (CONADICO), Medical Director of the Satelite Hospital and Surgical Center.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
Student, Nursing School, Mexico's Technological University (UNITEC).
Specialist in Gynecology and Obstetrics, re-certifi ed by the Mexican Board of Gynecology and Obstetrics, Professor of Genital Tract and Anal-Perineal Complex Pathology Degree (UNAM), (CONADICO), Medical Director of the Satelita Surgical Center Hospital.