Eagle's syndrome can be defined as the elongation of the styloid process and the calcification of the stylohyoid ligament. It is characterized by painful pharyngeal symptoms, odynophagia, dysphagia, headaches, pain irradiation to the ear and cervical pain. The average length of the styloid process is 2.5cm. Eagle's syndrome etiology is not well known. The present study reports the case of a 53 year old male patient who presented cervical pain, pain at the lateral region of the neck, as well as limitations in neck lateral movements. Protocol was initiated for stylohyoid ligament resection via extended sub-mandibular extra-oral approach. The aim of the present article was to raise awareness on the advantages of extraoral approach in these cases, as well as supplementary postsurgical therapy used at the Regional Hospital «Licenciado Adolfo López Mateos», ISSSTE (Mexico).
El síndrome de Eagle es definido como la elongación del proceso estiloides y calcificación del ligamento estilohioideo, se caracteriza por sintomatología dolorosa faríngea, odinofagia, disfagia, cefalea, irradiación de dolor a oreja y dolor cervical. El promedio de longitud del proceso estiloides es de 2.5cm. La etiología del síndrome es poco conocida. Se reporta el caso de un paciente masculino de 53 años de edad con cervicalgia, dolor en región lateral del cuello, limitación de movimientos de lateralidad del cuello. Inicia protocolo para exéresis de ligamento estilohioideo por abordaje extraoral de tipo submandibular extendido. El objetivo del artículo es dar a conocer las ventajas del abordaje extraoral para esta patología, así como la terapia complementaria postquirúrgica empleada en el Hospital Regional «Licenciado Adolfo López Mateos» del ISSSTE.
The classical definition of Eagle's syndrome is the elongation of the styloid process and the calcification of the stylohyoid ligament. The condition is characterized by painful pharyngeal symptoms, odynophagia, dysphagia, headaches, pain irradiation to the ear, as well as cervical pain. In some cases, even vertigo and syncope have been reported.1 In many cases, symptoms are vague and non-specific, therefore, patients seek consultation with surgeons, dentists, neurologists or psychiatrists and thus receive countless treatments that do not provide clinical improvement.2,3
The first case reported in scientific literature described a calcified elongation of the stylohyoid ligament. This description was undertaken in 1652 by Pietro Marchetti, a Padua (Italy) surgeon.4 In 1872, Weinlechner described the first case of surgically treated stylohyoid process elongation. In 1937 Dr. Watt W. Eagle, at Duke's University, began to defi ne the syndrome as the result of a styloid process elongation.
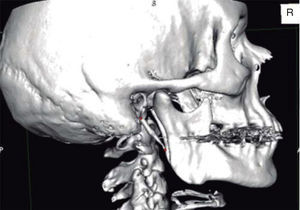
He described it in two syndromes (classical syndrome after tonsillectomy and stylo-carotid syndrome not associated to tonsillectomy). He established the fact that symptoms were caused by a styloid process’ length of more than 25mm.5,6 Incidence has been reported to be between 1.4 and 30%. In order to be able to diagnose this syndrome, it is necessary to conduct palpation of the tonsillar fossa as well as infiltrate it with local anesthetic. X-ray assessment with ortho-pantomography can reveal ligament calcification, which extends as a radio-opaque area up to the posterior region of the mandibular ramus.3,7 Nevertheless, in many cases, panoramic X-rays can distort the styloid process's dimensions and magnify the image due to the different angulations that can be present.8 Computed tomography with 3D reconstruction has been of great diagnostic help, since it allows for precise measurements and thus establish a more accurate diagnosis.
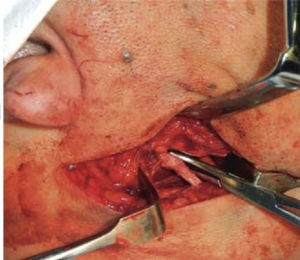
Treatment of choice is styloid process resection surgery, with extra-oral or intra-oral approach. The first extra-oral approach was described by Loeser and Caldwell in 1942. It was described as a proximal incision close to the sternocleidomastoid muscle up to the hyoid bone portion. The parotid fascia is upwardly retracted, and the carotid sheath along with the sternocleidomastoid muscle are placed to the rear, muscle insertions in the styloid process are dissected and the process is removed. Advantages of this type of approach are suitable visibility and handling of adjacent structures as well as sterile operative handling. Nevertheless this is a surgical technique requiring drains, sutures, and above all, it leaves a visible scar in the neck.2,8 Eagle described an intraoral approach: in this procedure, the styloid process is located through digital palpation in the tonsillar area. An incision is performed with blunt dissection, until locating the styloid process, which is then removed. If the palatine tonsil were to be present, a tonsillectomy is conducted at the same surgical event.2,4,9
Nevertheless, time has brought about alternative handling methods, such as steroids and lidocaine application, as well as trans-pharyngeal fracture of the styloid process.3,7,10
As mentioned beforehand, this condition consists of two syndromes: the first «classical» syndrome is observed after tonsillectomies, and is due to the direct irritation of soft tissues and glossopharyngeal nerve around the stylohyoid chain. The second, syndrome of the carotid artery or stylocarotid syndrome is caused by the pressure exerted by the stylohyoid ligament to the carotid artery's external and internal rami, generating painful symptoms at the irrigation zones (mainly peri-orbital and parietal region).11
Embryologically, the styloid process originates from the Reichter's cartilage (second pharyngeal arch), which in itself presents four growth centers: tympanum, styloid, ceratohyal and hypohyal. Tympanohyal portion forms the base of the styloid process until reaching full calcification at 8 years of age. Stylohyal portion forms the body of the styloid process, the calcification degree of this division determines the length of the process. The ceratohyal portion forms the stylohyoid ligament, which in many mammals is calcified (epihyal). The hypohyal portion develops the minor horn of the hyoid bone. The styloid process is projected in a caudal-medial direction into the para-pharyngeal space, separating it into two compartments. The first compartment is called retrostyloid where the internal jugular vein is located, internal carotid vein vagus nerve, glossopharyngeal nerve, accessory and hypoglossal nerve, and the second, the pre-styloid, which contains the maxillary artery, lingual nerve, auricular-temporal nerve and with lower communication to the tonsillar space. There are three muscles and two ligaments which insert into the styloid process (styloid-pharyngeal muscles, stylohyoid, styloglossus and stylohyoid ligament and stylomandibular ligaments). The length average of the styloid process is 2.5cm. Eagle's syndrome etiology is not well known, nevertheless it is considered that there is increased calcification of the ceratohyal portion. Moreover, there could be a calcification at the stylohyal portion, which could be due to embryological potential or as a response to trauma.12 In 1986, Langlais et al described a classification for this condition in the following manner: type I (elongated), type II (pseudo-articulated), type III (segmented). They also described different calcification patterns: (external calcification, partially calcified, nodular, and fully calcified).13,14 Sudden death cases have been reported where autopsy revealed presence of styloid process elongation, where continuous irritation of vagus nerve was presumed as well as of the carotid sinus which could lead to sudden cardiac failure.15,16
The aim of the present article was to raise awareness on the advantages of extra-oral approach to treat this condition, as well as postsurgical adjunctive therapy used at the Regional Hospital «Licenciado Adolfo López Mateos» ISSSTE.
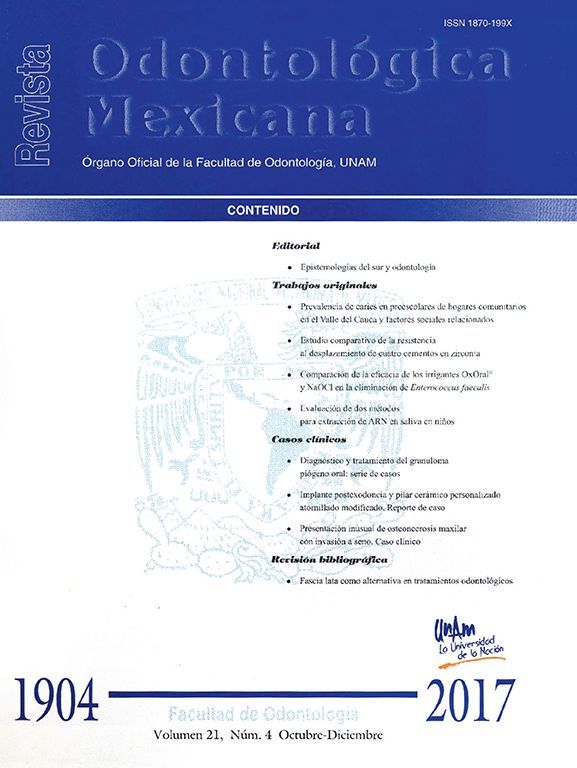
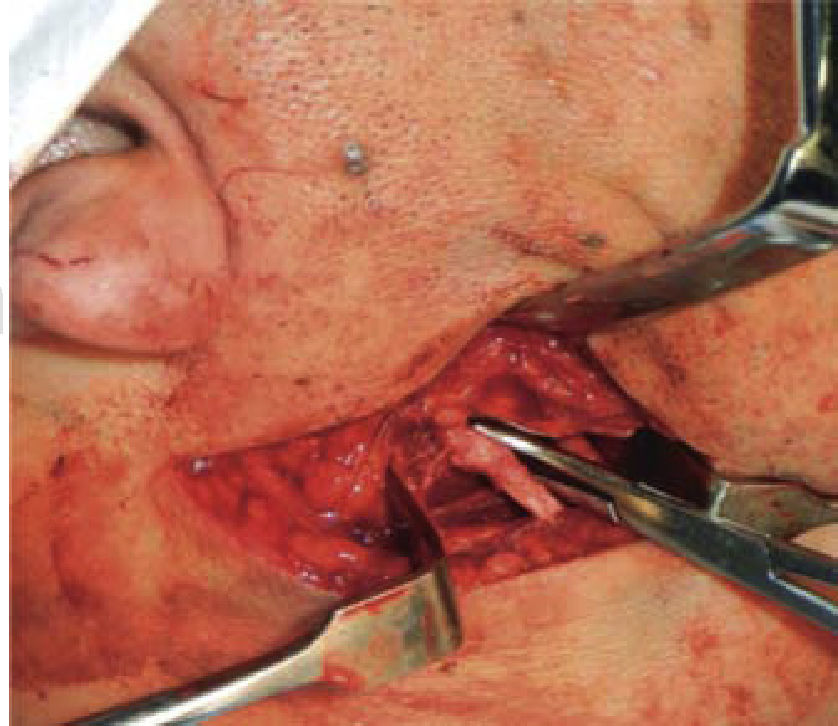
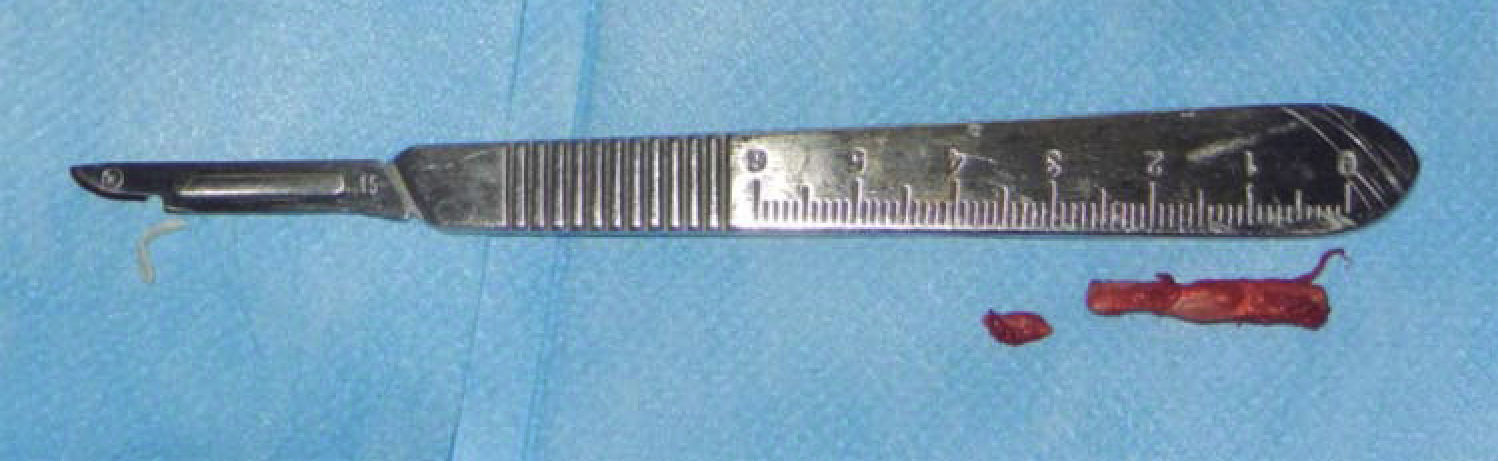
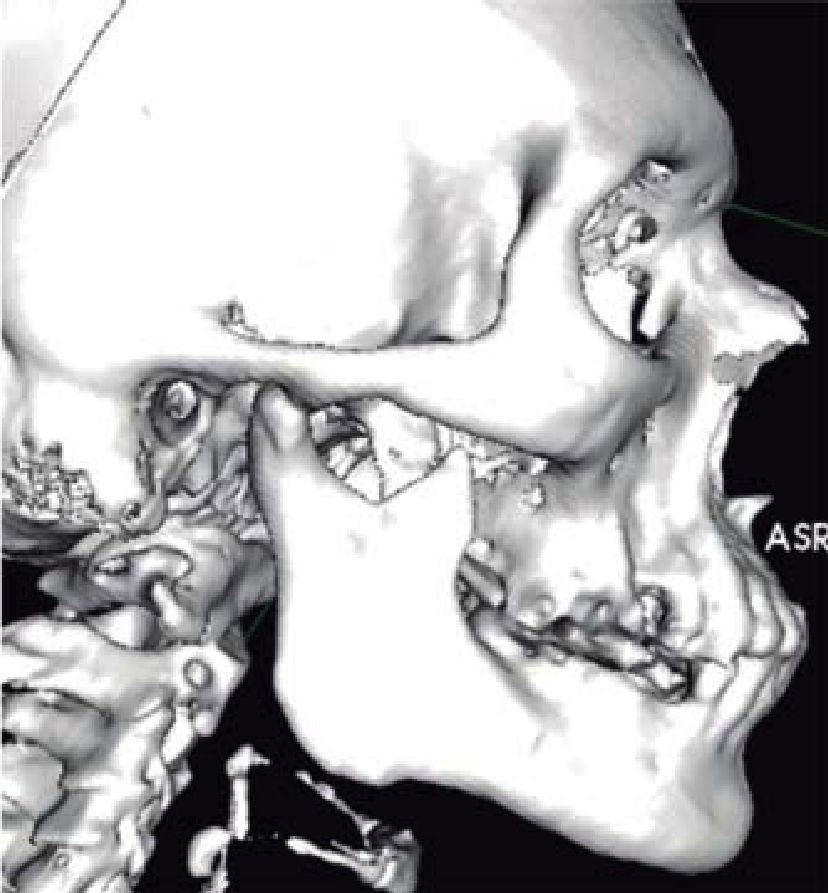
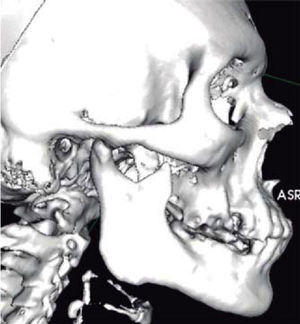
CASE REPORTA 53 year old male patient attended the Regional Hospital «Licenciado Adolfo López Mateos». The patient was referred from his family clinic due to painful symptoms of the cervical region during lateral neck movements which were associated to probable elongation of the styloid ligament. The case was thus diagnosed as possible Eagle syndrome. Clinical exploration revealed a male patient, with matching chronological and apparent age, normal skull, with no palpable exostoses or indentations, hair normally inserted into the skin, undamaged orbital ridges, suitable eyebrow thickness, central and symmetric nasal pyramid, with permeable nostrils and undamaged maxillary ridge. Intraoral clinical exploration revealed incomplete permanent dentition with misplaced teeth, oral mucosa of suitable color and hydration, preserved lingual movements, presence of well circumscribed volume increase, of the same color as the adjacent mucosa, of approximately 0.9cm, unaltered dorsum and floor of the mouth, just like the soft and hard palates and the oral pharynx. Full mandibular ridge, short and cylindrical central neck with presence of nevus at the anterior left triangle. Upon palpation, masticatory muscles revealed painful symptoms at the following muscle trigger points: temporal, masseter, sternocleidomastoid muscles as well as in posterior neck muscles. Limited right laterality and painful symptoms were observed when the patient performed lateral movements. Computerized axial tomography of the patient with 3D reconstruction was requested. CAT revealed a 3.7cm long stylohyoid ligament elongation, observed in sagittal crown axial cuts and corroborated with 3D reconstruction. (Figure 1). Remaining structures did not exhibit relevant data for treated condition. Treatment proposed was resection of calcified stylohyoid ligament under balanced local anesthesia performed in the operating theatre. The patient agreed and signed informed consent form. A 10cm long right submandibular linear incision was undertaken. Resection by planes was conducted until reaching the basal region of the mandibular angle. With the help of palpation, stylohyoid apophyses as well as ligament calcification were located. Inserted muscles were dissected with a curette, and then fractured with Kelly forceps. Ligament and apophyses fragments were placed in 10% formaldehyde to be sent to histopathological analysis. Suture by planes was executed with internal inverted simple sutures, skin was sutured with 6-0 subdermal nylon. Surgical procedure was completed with no further accidents or incidents. A compressive dressing was placed on the right submandibular region. The patient was sent to recovery and was hemodynamically, cardiopulmonarilly and neurologically stable (Figures 2 to 5). The patient was discharged the following day, the dressing was removed, suitable healing of the surgical wound was observed, no blood collection or egress of material was noted. Seven days later, the patient exhibited suitable healing with decrease of painful cervical symptoms as well as limited neck lateral movements. Tomography images were requested in order to assess surgical treatment (Figure 6). Three months later the patient exhibited mild painful symptoms located at the right sternocleidomastoid muscle, with mild limitation of lateral movements, it was decided to apply botulinic toxin, 100 UI at the sternocleidomastoid, trapezius and posterior neck muscles. 15 days later the patient was re-examined: he exhibited clear improvement of the painful muscle syndrome. Histopathological report informed of «trabecular bone and hyaline cartilage with focal calcification, fibro-connective tissue with mild recent hemorrhage». The patient continues attending follow-up visits at 6 and 12 months at our service and has not exhibited any changes.
Eagle's syndrome is a condition often misdiagnosed and misinterpreted due to its clinical characteristics, since the patient might exhibit a great variety of symptoms. It is important to note that clinical data of said condition are not definite data upon which a diagnosis can be emitted. As mentioned by Bagga et al (2012), Beder et al, 2005 and Abdel-Ghany,14 additional X ray studies (CAT with 3 D reconstruction and orthopantomography) provide accurate diagnosis.
There are many ways to surgically treat styloid process resection. Many extra oral approaches have been described, among them, the sub-mandibular, pre-auricular, retro-auricular as well as intra-oral approaches (Williams et al 2011, Buono et al 2005, Bueno 2011). Nevertheless, at the Maxillofacial Surgery Service of the Regional Hospital «Licenciado Adolfo López Mateos» ISSSTE, one of the approaches used to resect styloid processes of patients suffering Eagle's syndrome is the extended submandibular extraoral type of approach. This technique presents the advantages of providing better vision of important anatomical structures in the operating field. Esthetics would be another point to consider since this approach is executed underneath the mandibular ridge, on a facial expression line.
From the clinical point of view, and concurring with authors such as Williams et al 2011, Beder et al 2005, Bagga 2012 and Rechwet 1998, we have found that painful symptoms are always confused with conditions such as headaches, painful myofascial syndromes or joint dysfunctions. Radiographically, and concurring with other authors such as Jewett 2014, Andrade et al 2008, Fini 2000, we deemed computerized tomography the choice study, nevertheless, orthopantomography plays an important role in initial diagnosis.
We have additionally observed that surgical time is shorter when compared to intraoral approach since it is easier to handle proximity vascular structures achieving thus minimal bleeding during procedures. When compared to intra-oral approach, at the postoperative care phase, patients report greater ease of cleansing and thus absence of possible infection.
CONCLUSIONSAfter patient assessment, it was noted that the extended submandibular approach executed at the Maxillofacial Surgery Service of the Regional Hospital «Licenciado Adolfo López Mateos», ISSSTE, was an effective and efficient procedure to undertake stylohyoid ligament excision, achieving thus scarce surgical anatomical risks and suitable postoperative evolution. Botulinic toxin therapy provides more effective decrease of patient's initial painful symptoms. Postsurgical physical rehabilitation is of the utmost importance in order to de-program muscle chains which have become modified by the restriction of the ligament. It is essential to closely follow-up the patient in order to assess his evolution.
Regional Hospital «Licenciado Adolfo López Mateos», Institute for Security and Social Services of State Employees (ISSSTE).