Assessment of periapical and pulp disease prevalence as a risk factor for secondary uveitis in patients attending ISSSTE (Social Security Institute for Government Workers) in 2013 in the city of Merida, Yucatan, Mexico.
IntroductionPeriapical and pulp diseases can elicit inflammatory reactions which might affect vision.
Material and methodsThe present study was of a descriptive, cross-sectioned and observational nature. Patients’ Informed consent was secured. System identification card included demographic data, intraoral clinical examination results of 12 patients with an a priori diagnosis of secondary uveitis confirmed by a dentist, with presence of pulp or periapical disease along with history of pain (duration, frequency, type and quality), pulp examinations (palpation, percussion, thermal and vitality tests). Panoramic and periapical X-rays were taken, descriptive statistics were conducted as well as chi-square (χ2) test of goodness of fit for two categories with Yates correction.
ResultsOut of the 34 patients diagnosed with different types of uveitis, 35.29% was established as secondary uveitis. Of the aforementioned patients, 33.33% were in the 48-57 years age range. The examination encompassed 19 teeth of the 12 patients; out of these, 26.32% exhibited pulp disease and 73.68 periapical disease.
ConclusionDiseases involving dental periapex and pulp may cause inflammatory reaction in the eyes.
Evaluar la prevalencia de enfermedades pulpares y periapicales como factores de riesgo de la uveítis secundaria de pacientes del ISSSTE, Mérida, Yucatán, 2013.
IntroducciónLas enfermedades pulpares y periapicales pueden producir una reacción inflamatoria que afecta el órgano de la visión.
Material y métodosEstudio descriptivo, transversal y observacional. Se efectuó: consentimiento informado, cédula de investigación con: datos demográficos, resultados del examen clínico intraoral de 12 pacientes con diagnóstico a priori de uveítis secundaria confirmado por un oftalmólogo, con presencia de enfermedad pulpar o periapical acompañada con la historia de dolor (duración, frecuencia, tipo y calidad), exámenes pulpares (palpación, percusión, térmicos y de vitalidad). Se tomaron radiografías periapicales y panorámicas. Se realizó estadística descriptiva y se utilizó la prueba ji cuadrado (χ2) de bondad de ajuste para dos categorías con la corrección de Yates.
ResultadosDe 34 pacientes diagnosticados con diferentes tipos de uveítis, el 35.29% fue establecido como uveítis secundaria. El 33.33% de los pacientes con ésta estuvieron entre los 48-57 años de edad. Se estudiaron 19 órganos dentarios de los 12 pacientes, el 26.32% presentaron enfermedad pulpar, y 73.68% periapical.
ConclusiónLas enfermedades que involucran a la pulpa dental y periápice, pueden producir reacción inflamatoria en el ojo.
It is important for dentists to be knowledgeable with and be able to interpret the manner in which bacteria present in the mouth can act upon the genesis of systemic nosologies, where any lesion of the dental pulp can develop its inflammatory reaction. In cases when they are not timely treated, they might probably cause pulp necrosis. Anaerobic micro-organisms and gram-negative bacteriae are considered to be main etiological agents in the pathogenesis of periapical and pulp disease. Radiographic examination of these lesions reveals a radio-lucid area surrounding the apex. It is therefore necessary to understand the type of response generated in tissues in the presence of aggressors, as well as methods used to eradicate and control infections of the system of conducts and of periapical tissues, avoiding thus destruction of tooth-supporting bone.1–3
The means through which this infection can reach dental pulp is more often through the crown (caries, fissures, fractures, dental development defects) or through the dental root (caries of the neck, periodontal pockets, bacteremia). When studying odontogenic infections, it can be said that 70-95% of all odontogenic infections contain mixed flora (aerobic-anaerobic) produced by 5 to 8 different species, among which the following are prevalent: aerobic gram-positive cocci (Streptococcus 95%, Staphylococcus 5%), anaerobic gram negative cocci (Peptococcus, Peptostreptococcus spp and Peptostreptococcus micros) as well as anaerobic gram-negative bacilli (Bacteroides forsythus, Prevotella intermedia, Porphyromonas gingivalis and Fusobacterium spp).4 Periapical lesions are infections associated to anaerobic-type micro-organisms such as Porphyromonas endodontalis and Prevotella species among others.3,5,6
According to the classification established by the American Association of Endodontics (AAE)7 in 2007, correct diagnoses of periapical and pulp diseases are based on histological evidence complemented with radiographic and clinical findings. Pulp diseases are classified into: normal pulp, reversible pulpitis, symptomatic and asymptomatic irreversible pulpitis and pulp necrosis; it must be noted whether the tooth has been previously treated or initiated. On the other hand, toxic elements which are a product of pulp decomposition originated by microorganisms, toxins and enzymes act as irritants on the periapical tissues and give rise to many forms of reactions. Some of these reactions will take place in a short time and will be accompanied by signs and symptoms, others will slowly and progressively develop, and in general terms will be asymptomatic. Periapical classification has been established in the following manner: Healthy Apical Tissues, Symptomatic Apical Periodontitis, Asymptomatic Apical Periodontitis, Acute Apical Abscess, Chronic Apical Abscess and Condensing Osteitis.7,8
Along with the aforementioned situation, it can be said that uveitis is an inflammation of tissues surrounding the iris, ciliary body and choroids, although other intra-ocular structures such as retina and optical nerve can also be affected. The uvea is a single layer which begins at the iris, and continues into the posterior pole with the choroids. The term uveitis is applied to any inflammatory process of the uveal tract (iris, ciliary body, choroids) which, in certain cases, affects other neighboring structures. Any causing agent affecting the uvea will trigger inflammation's physiopathological mechanisms. These conditions can be exogenous in nature such as post-traumatic and post-surgical, or they can be endogenous (of greater importance) among which we can count the following: those exhibiting an infectious cause, those related to systemic diseases and idiopathic uveitis. Several methods are presently employed to describe variations of intra-ocular inflammation that can affect not only the uvea but adjacent structures as well. Pathogeny might include immune system infections and/or alterations, and might be primarily ocular (primary uveitis) or associated to systemic or infectious diseases (secondary uveitis)1,9–11 Microorganism dissemination towards the orbital area is due in the adult, to infections at the incisor, canine or premolar areas, and in children to any tooth in the upper jaw. They can extend to soft tissues, mainly the upper lip area, and, due to the fact that the canine muscle can be found at each side of this structure, there is a communication of the infection with the eyelid region and the inner canthus of the eye, among the fibers of the upper lip elevator muscle and between this and the nasal wing elevator.4
An uveitis classification method has been developed according to inflammation site, this improves circumstances of uveitis diagnosis and treatment. In this classification, the following can be found: anterior uveitis or iritis, intermediate uveitis or parsplanitis, posterior uveitis (Figure 1) and panuveitis or diffuse uveitis. Within this classification, anterior uveitis is the most common, accounting for 50-60% of all cases. Among reported symptoms we can count the following: photophobia, blurry vision and pain and reddening of the eye. This condition is diagnosed through radiographic, laboratory and clinical examinations as well as ophthalmic and dental examinations.11 Ophthalmic examination include direct ophthalmoscopy, slit-lamp examination, fluorescence staining as a contrast medium to conduct retina fluorangiography (FAG) and Shimmer test.12 On the other hand, a non invasive technique to assess fundus has been integrated into the opthamological examinations: this technique is called optic coherence tomography; its characteristic is the ability to quantitatively measure macular volume and central point thickness (CPT).13
In anterior uveitis cases, establishing whether it is infectious or non infectious is fundamental in order to devise suitable treatment. Over 50% of patients with anterior uveitis receive a diagnosis of idiopathic disease, and are treated with topical and orallyadministered immune-suppressor agents which could worsen the underlying infectious uveitis. This is due to the sensitization of uveal tissue caused by microorganisms which can be guest microorganism; this has caused a search for distanced infectious foci whose elimination will determine the non-remission of the uveitis, breaking thus relapse cycles.11,14 Nevertheless, in some cases and to alleviate uveitis discomfort, dexamethasone/neomycin drops are prescribed, although this is not advisable since it could mask the true provenance of secondary uveitis.
Although most cases of uveitis are considered immune system mediated diseases, infectious disease is the second most important group within uveal disease etiology. When there is an infectious cause, it can remain latent or chronic, and can mimic cases of uveitis associated to auto-immune diseases.15,16
The clinical picture of infectious secondary uveitis can appear in one or both eyes; it has sudden onset and can rapidly worsen. A characteristic of said uveitis is habitual eye pain, sensitivity to light (photophobia) or reddened eyes. In cases of intermediate or posterior uveitis the most common symptom is blurry or impaired vision, which can be accompanied by perception of dark points or apparent flying flies.14
Since uveitis is little known in the dental field, it can be primarily ocular, and can be associated to the inflammation of other eye structures or adjacent to the orbital cavity, due to existing proximity among tissues. Nevertheless, in general, its frequency depends on the disease to which it is associated. In the dental field, uveitis appears secondarily through the dissemination of a focal infection present in the oral cavity, either through innervation of the facial cranial complex by the trigeminal nerve as well as other cranial pairs, as well as hematogenously, or it can also be due to an antigen-antibody reaction. Frequently, patients who show no infection focus are diagnosed with uveitis due to the presence of dental abscesses which might be in direct contact with bone tissue, which in turn is subjected to pressure changes and irritation as a result of the masticatory process, causing thus ingress of bacteria into the blood stream and the lymphatic system.14,15,17,18
Oral lesions that might create primary infectious foci in the population are acquired due to poor hygiene habits, deficient eating habits or some unknown or multi-factorial etiologies. Among these the following can be included: caries, periodontal disease, dento-alveolar lesions, alterations of the pulp chamber and alterations of the tooth structure caused by physiological wear (attrition), pathological wear (abrasion) and to chemical-type lesions such as tooth erosion, residual alveolar infection, periapical cyst, periapical granuloma, pulp disease ad pericoronitis.17,19
The aim of the present study was to establish prevalence of pulp or periapical diseases as a risk factor for secondary uveitis in patients attending outpatient clinic at the Familial Medical Unit of the Institute for Social Security of Government Workers (ISSSTE) at the Lindavista Clinic, Mérida, Yucatan.
MATERIAL AND METHODSA total of 34 patients were studied, 12 male and 22 female, ages ranging 18-77 years, mean age 47.5 years. Patients exhibited different types of uveitis that had been previously diagnosed by ophthalmologists of the Familial Medical Unit of the ISSSTE Lindavista, Merida Yucatan, Mexico. Out of the 34 patients under study, 15, who presented infectious secondary uveitis, (diagnosed by ophthalmological specialists) were subjected to an oral study according to Mexican Official Norm NOM-013-SSA2-2006,20 established for infection control. During the search for infectious processes in the mouth, the following procedure was adhered to: a voluntary, informed letter of consent was signed in order to preserve the ethical aspects requested by the Helsinki Declaration of the World Medical Association for medical patients.21 Patients were treated with dignity, responsibility, confidentiality, equity, honesty, justice and respect to their rights.22 The questionnaire used simple words and was integrated by demographic data, medical history and assessment of pain signs and symptoms. For endodontic diagnosis, the current classification of the American Association of Endodontics 20097 was used, as well as the terms for «positive» and «negative» predictive values to establish current pulp diagnosis. That is to say, a tooth's relationship with positive or negative test. The aforementioned results were diagnosed with methods of A) thermal pulp tests (heat and cold: with heat when a positive result was obtained with hot water or, more specifically, with a stick of hot gutta-percha on the suspected tooth and with cold when positive stimulus was caused with Endo-Ice® on an hyssop applied to the suspected tooth). Different responses to thermal tests of pulp afferents can determine health or disease. In electrical tests conducted with an Element® brand vitalometer, the 1 to 10 scale was used for voltage amount. Sensitivity increased when electric stimulus was applied to the tested tooth, until the moment when the patient exhibited a violent reaction and moved the head away from the instrument. This means that a higher number of violent responses represent a positive response to a vital, diseased pulp; when a negative response is elicited, the pulp tissue is non vital. 2), palpation: 3) percussion (palpation and percussion revealed the involved tooth) Nevertheless very often it was not clarified whether pulp or periodontium were affected. 3) it was likewise the case with diagnostic approaches: a) tincture or transillumination (to observe presence of caries, fissures or fractures which are essential for inclusion criteria. B) Periapical radiographic examination with parallelism technique, using XCP (Dentsply®) as addition, as well as number 2 X-rays, or panoramic x rays (when more than a tooth is suspected, using program SIDEXIS-XG, following the Official Mexican Norm NOM-229-SSA1-2002 for radiation protection, using thus lead apron with thyroid neck for all patients.23
Statistical methodGraphic methods and cross tables were used to describe results. Square chi test for goodness of fit was used for two categories, with Yates correction to compare proportion of patients with secondary uveitis diagnosis with proportion of patients diagnosed with other uveitis types. Since normality supposition was not met, Wilcoxon test was used for samples related in the comparison of number of teeth damaged by periapical and pulp lesions. Results of statistical tests were considered significant when p≤0.05, and trends when 0.05<P<0.10.24,25
RESULTSThe Ophthalmology Department referred to the Dentistry Department 34 patients diagnosed with different types of uveitis: 65% (n=22) suffered primary uveitis and 35% (n=12) were established as suffering from infectious secondary uveitis: 75% (n=9) were female and 25% (n=3) male.
During intraoral clinical inspection and x-ray examination, 58% (n=7) patients with secondary uveitis presented symptoms of anterior uveitis, whilst 41.67% (n=5) presented intermediate uveitis.
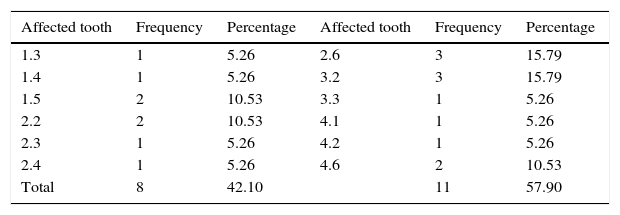
Nineteen teeth with pulp or periapical disease belonging to patients diagnosed with secondary uveitis were examined. In this exam, 26-32% (n=5) of affected teeth exhibited pulp disease and 73.68% (n=14) showed periapical disease. Pulp necrosis was present in 15.78% (n=3) patients, 57.89 (n=11) presented asymptomatic apical periodontitis and 10.52% (n=2) showed symptomatic apical periodontitis. These latter patients presented a painful, inflammatory clinical picture (Figure 2).
The most affected quadrant with respect to pulp or periapical disease was the upper left, with 36.84% (n=4) (Figure 3), whilst the most affected teeth with pulp or periapical disease were 2.6 and 3.2 with 25% (n=3) respectively.
According to obtained data and conducted statistical analysis, it was observed that patient proportion did not significantly differ among patients diagnoses with secondary uveitis and those diagnosed with other types of uveitis (χ2=2.3824, g.l.=1, p=0.1227) that is to say, uveitis resulting from oral infection such as periapical and pulp diseases have the same apparition proportion than other types of primary uveitis.
While studying affected teeth of 12 patients with secondary uveitis a comparison was established with present periapical and pulp diseases, it was observed that the number of damaged teeth did not significantly differ (p>0.05) when comparing both lesion types. Nevertheless, a trend was observed (p<0.10) of a greater number of teeth affected by periapical disease when compared to teeth affected by pulp disease (T=8, p=0.0586), that is to say that periapical diseases exhibit greater propensity to become a risk factor for secondary uveitis.
DISCUSSIONIn the dental field, periapical and pulp diseases can be considered one of the main dental disorders which prompt the patient to attend a dental office. These diseases are able to cause alterations in the stomatognathic system and bear repercussions in the whole body as a true focus of infection, especially secondary manifestations that could appear as is the case of secondary uveitis which is an inflammatory reaction that affects vision.
In a study conducted by Peña M et al1 in 2012 with 26 uveitis patients in search of oral-originated septic foci which might cause uveitis, it was shown that periodontal-type diseases were most frequent. Nevertheless, said diseases were followed by endodontic type diseases, especially periapical diseases, since it is supposed that, when bacteriae and their products come into contact with periapical tissues, these can enter the bloodstream, provoking a meta-focal reaction such as uveitis, since its proximity to the mouth is really of the utmost importance. Periapical type diseases and those diseases where chronicity increases the time in which bacterial products are present, they can become a possible risk factor for the onset of uveitis. The aforementioned observation concurred with the present study, where, upon studying these endodontic types where asymptomatic apical periodontitis is most frequently found, it was observed that these can increasingly become an infection focus which ends up triggering a reaction in the patient's vision.
Immune type diseases such as ankylosing spondylitis or osteoarthritis are main causing factors of uveitis. Nevertheless, when they are caused by an infectious focus, they produce secondary uveitis. Based on this, Gonzalez J et al15 2012, mentioned in their bibliographic research that uveitis appears primarily in ocular location, or either associated to general disease and infectious foci in the dental field such as secondary manifestation of herpes zoster, herpetic stomatitits, or Sjögren's syndrome. In their conclusions, they established that its onset is in the sixth decade of life with no gender predilection. Main symptoms are: blurry vision, pain and reddening of the eye, which appear according to the anatomical site where inflammation of the eye occurs, not omitting that they appear accompanied by lesions present in the mouth. Endodontic-type lesions cause a set of changes along dental pulp, until reaching the tooth's support system, that is to say, the periodontium. Thus, inflammatory processes derived from pulp disease reach healthy tissue at periodontal level. This makes them an imminent infectious focus which can give rise to an ocular disorder such as secondary uveitis.10,11
Frequency of 19 teeth affected with periapical and pulp disease in 12 patients with secondary uveitis, Merida Yucatan, Mexico, 2013.
| Affected tooth | Frequency | Percentage | Affected tooth | Frequency | Percentage |
|---|---|---|---|---|---|
| 1.3 | 1 | 5.26 | 2.6 | 3 | 15.79 |
| 1.4 | 1 | 5.26 | 3.2 | 3 | 15.79 |
| 1.5 | 2 | 10.53 | 3.3 | 1 | 5.26 |
| 2.2 | 2 | 10.53 | 4.1 | 1 | 5.26 |
| 2.3 | 1 | 5.26 | 4.2 | 1 | 5.26 |
| 2.4 | 1 | 5.26 | 4.6 | 2 | 10.53 |
| Total | 8 | 42.10 | 11 | 57.90 |
Source 2013 research data.
Dental numbering system: IDF or double digit.
The manner in which a dental-origin infectious focus can cause inflammatory reaction in the uveal tract is difficult to establish due to scant information. Nevertheless, Diaz J et al,17 published three theories or dissemination pathways for an infection; they are: neurovegetative theory, infectious-allergic theory and immunopathological theory. Pulp, periapical and periodontal conditions are the main lesions that can cause a primary infectious focus in the mouth, where bacteriae, either through the bloodstream or along trigeminal nerve connections, are able to cause bacterial endocarditis, rheumatic fever, rheumatoid arthritis or even ophthalmic disorders such as uveitis.17
CONCLUSIONSIn the presence of an ophthalmic affliction such as secondary uveitis, resulting from an infectious process whose risk factor could be of dental origin, first of all, location must be established as well as the tooth originating focal involvement; it must additionally be established whether there is clear relationship between both entities (with clinical and radiographic tests). These cases require multi-disciplinary treatment involving dentists and ophthalmologists: both medical professionals must conduct these patients’ follow-up.
It is of the utmost importance to point out that, in the present study, signs and symptoms decreased when patients were subjected to endodontic treatment or extractions of teeth suspected to be the risk factor for secondary uveitis. This fact was confirmed in follow-up visits conducted at the institution's specialists such as ophthalmologists. On the other hand, consultation of other articles revealed the suggestion that damaged cells do not experience repair. Nevertheless, it cannot be stated that periapical and pulp diseases are risk factors of infectious secondary uveitis. Studies with larger numbers of patients are needed, therefore, it is suggested to continue research on the important and interesting subject of secondary uveitis, which must not be considered a rare disease.
Full time teacher at the School of Dentistry, Autonomous University of Yucatan, Mexico.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
DDS, private practice.
Full time teacher at the Mathematics School of the autonomous University of Yucatan, Mexico.
General Physician, Graduate from the School of Medicine of the Autonomous University of Yucatán, resident at the Nose, Throat and Ear and Head and Neck Surgery Specialty at the General Hospital in Mexico (Hospital General de Mexico). Health Ministry (Secretaria de Salud).