Traumatic dental injuries (TDI) are very common, they are mainly originated from blows caused by objects or due to falls, sport injuries as well as injuries sustained during leisure activities and car accidents. Most cases involve anterior teeth, of which upper central incisors are more frequently affected. Andreassen's TDI classification, sanctioned by WHO in 1978 in «International disease classification», is described here. When new technologies are incorporated into dental practice, computer-assisted design and computer-assisted manufacture (CAD/CAM) provide the restorative clinician with new treatment options, thus improving design and application of metal-free ceramic restorations, which, along last decade, have haven proven to provide suitable clinical performance. Three patients were treated at the Advanced Restorative Dental Graduate Program clinic. The first one sought treatment within the first 48hours after TDI, in central and right lateral teeth; two patients exhibited TDI in one central incisor, the first one was a 28 year old male with a five year evolution of the injury and no previous treatment, the second case was a nine year old child who arrived having been subjected to root canal treatment, with a six month evolution.
Las lesiones dentales traumáticas (LDT) son comunes, siendo las principales causas: golpes por caídas u objetos, traumatismos deportivos, actividades físicas de ocio y accidentes automovilísticos. Casi todos los casos abarcan los dientes anteriores, con mayor frecuencia los incisivos centrales superiores. De las clasificaciones de LDT, se describe la propuesta por Andreassen y aceptada por la OMS en su «Clasificación internacional de las enfermedades» des-de 1978. Sumando tecnologías a la práctica odontológica, el diseño asistido por computadora y la fabricación asistida por computadora (CAD/CAM), proporcionan al rehabilitador nuevas modalidades de tratamiento, mejorando el diseño y la aplicación de restauraciones cerámicas libres de metal, que a lo largo de la última década ha demostrado un buen desempeño clínico. Se presentan a la clínica de la Especialidad de Odontología Restauradora Avanzada, tres pacientes, de los cuales el primero se presentó en las primeras 48 horas luego de la LDT en centrales y lateral derecho; dos pacientes presentaban LDT de uno de los incisivos centrales, el primero un adulto de 28 años de edad con una evolución de cinco años y sin ningún tratamiento ejecutado aún; el segundo caso, un niño de nueve años de edad que se presenta con un tratamiento de sistemas de conductos con una evolución de seis meses.
A literature review carried on from 1995 onwards showed worldwide high prevalence of traumatic dental injuries (TDI) in primary and permanent dentitions. Statistics of most countries reveal that a fourth of all school age children and almost a third of adults have suffered TDI, nevertheless, there are differences in these figures according to different countries. Main TDI causes are blows due to falls, objects, sport, collisions, leisure physical activities and traffic accidents. These incidents are more frequent in the autumn.1–3
It is considered that 47% of all TDI receive treatment, nevertheless, this treatment is inadequate in 59% of all cases, and only in 4% of these cases are patients treated by a dental specialist.4 Almost all lesions are located in anterior teeth, mainly upper central incisors; generally, one tooth is affected. Facial pattern is another aspect to be taken into consideration, subjects exhibiting protruded incisors suffer almost twice the possibilities to experience TDI than other subjects with normal horizontal overbite.5–7
OBJECTIVETo achieve description of multi-disciplinary clinical treatment of three patients exhibiting traumatic dental injuries (TDI) who attended the Clinic of Advanced Restorative Dentistry at the Graduate and Research School, School of Dentistry, National Autonomous University of Mexico (UNAM).
Traumatic dental injuriesThey can be classified according to involved structures. Although many TDI classifications exist in scientific literature, the present article will use the one described by Andreassen and accepted by WHO in their «International classification of diseases» of 1978.5,8
Dental tissue and pulp lesions- •
Dental crown infringement: cracks in the enamel without structure loss.
- •
Crown fractures.
- -
Enamel fracture.
- -
Enamel and dentin fracture.
- -
Compound fracture involving enamel, dentin and pulp.
- -
- •
Root fracture.
- •
Crown and root fracture.
- -
Non-compound fracture of root and crown without pulp exposition.
- -
Compound fracture of root and crown with pulp exposition.
- -
- •
Concussion: no displacement or mobility are observed, there is pain upon percussion.
- •
Dental displacement such as intrusion, extrusion, and lateral luxation.
- •
Subluxation (mobility).
- •
Avulsion (tooth loss).
- •
Alveolar bone fracture.
- •
Alveolar process fracture.
- •
Fracture of upper or lower jaw (maxilla or mandible).
When compared to other traumatic lesions, dental lesions are considered less severe. Nevertheless, since teeth exhibit low potential to recover a healthy state after a trauma incident, most of the lesions located in this region require urgent diagnosis and treatment. Although, oftentimes, signs and symptoms are complex, precise treatment depends on accurate diagnosis.2,5,9,10
Clinical assessmentInitial observation plays a key role in order to establish suitable diagnosis and design the best therapy to follow.
Extra-oral explorationWhen a patient arrives with oral and facial trauma, observation of incised wounds, contusions and abrasions to face and lips must be undertaken. It must be remembered that any type of chin lesion might involve possible fractures of the mandible, which, in children, is frequently located at condylar level. Another element to explore is the possibility of molar fractures, caused by the blunt blow of lower arch on upper arch. Suspicion of the presence of maxillary, malar and mandibular fractures must be taken into account when asymmetries are observed upon asking the patient to open and close his mouth. In cases when in a dental crown fracture there were lacerations of the lips, before suturing, the possibility of fragments included in the muscle mass must be considered.5
Intra-oral explorationTo assess tooth mobility in vertical and horizontal directions. An alveolar process fracture must be suspected in those cases when upon moving a tooth, many others move as well.1,5
A periodontal ligament lesion must be suspected when pain is elicited upon soft percussion on a tooth. When assessing tooth hypersensitivity or mobility, comparison should be established with the non-affected area. Possibility of pulp exposure must be considered when observing fractured teeth.3,5
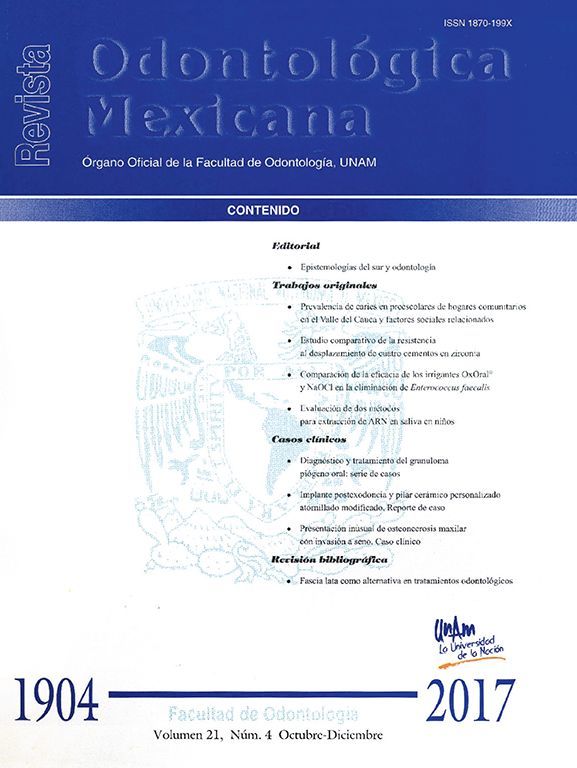
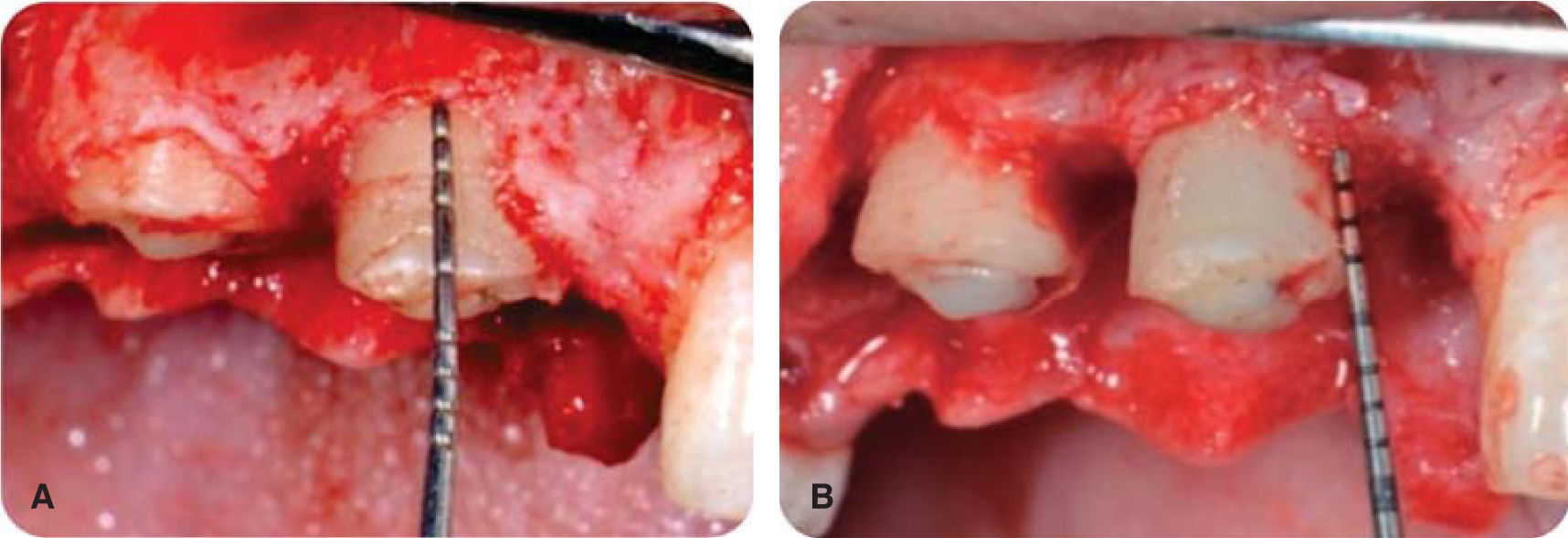
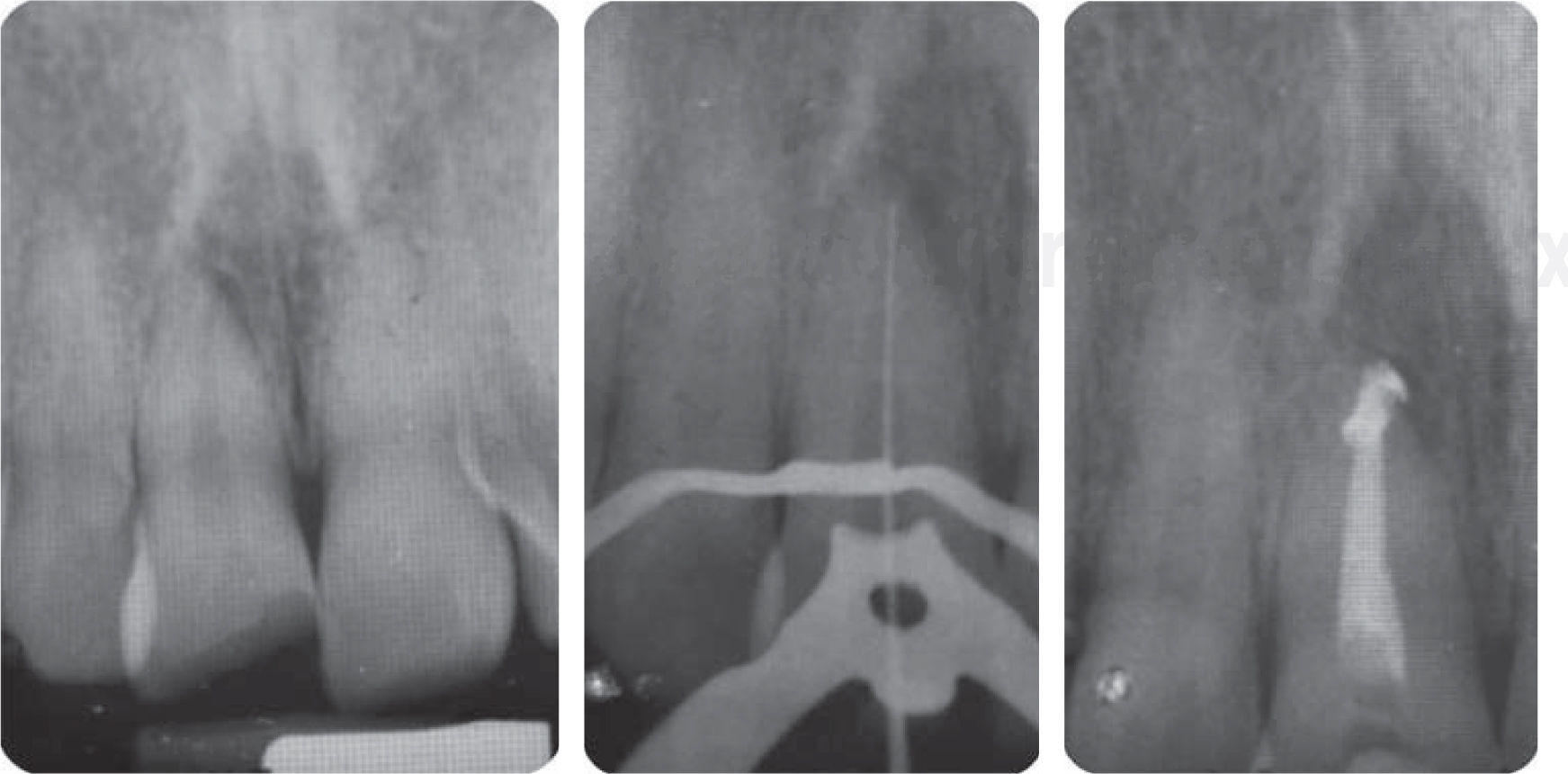
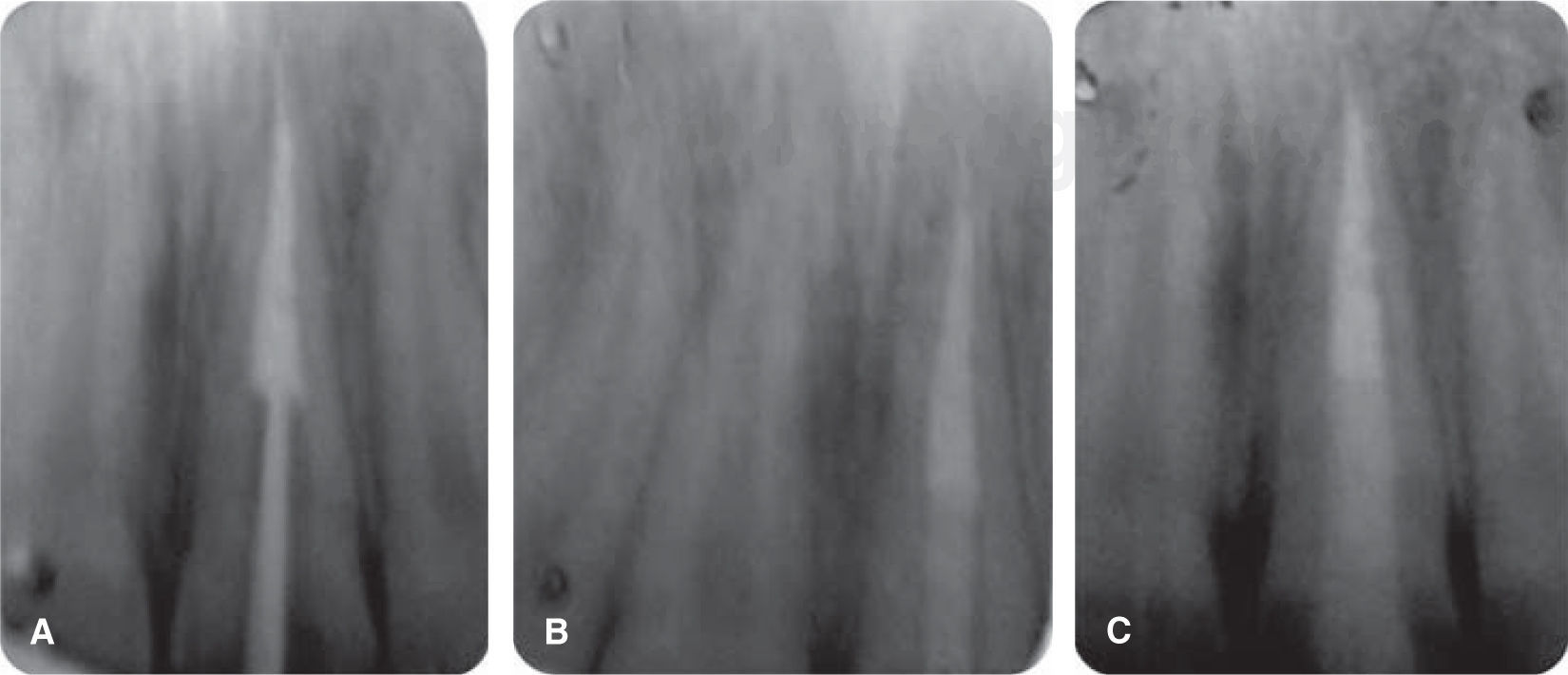
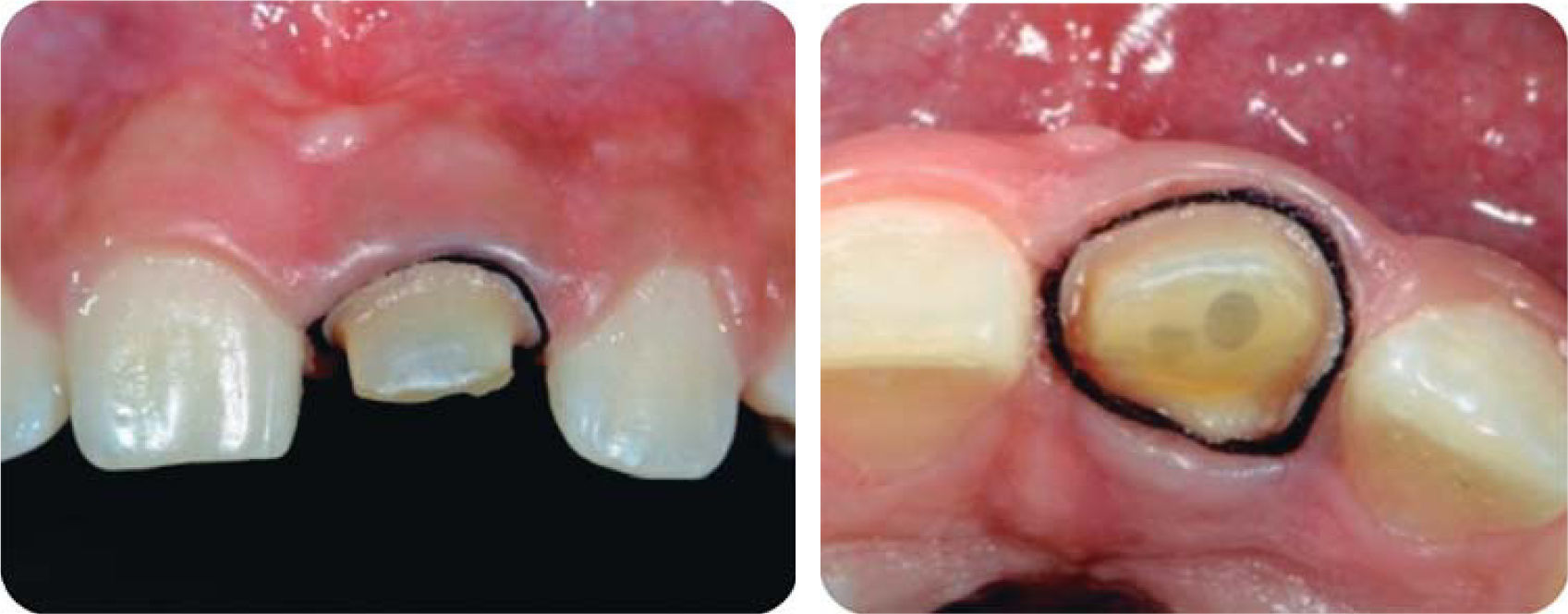
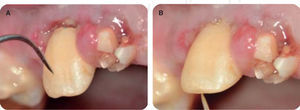
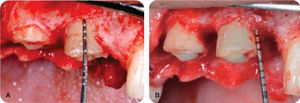
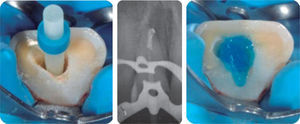
CLINICAL CASE 1A 21 year old healthy patient sought treatment for TDI caused by a bicycle fall. Lesions included compound crown fracture in teeth numbers 12, 11 and 21. Injury evolution was 48hours (Figure 1). Due to the fact that the lesion had a two day evolution since the accident, upon exploration, the patient suffered pain and inflammation. Intraoral exploration revealed pulp exposition of involved teeth (Figure 2), and warranted emergency treatment to be instated in order to decrease pain and inflammation.
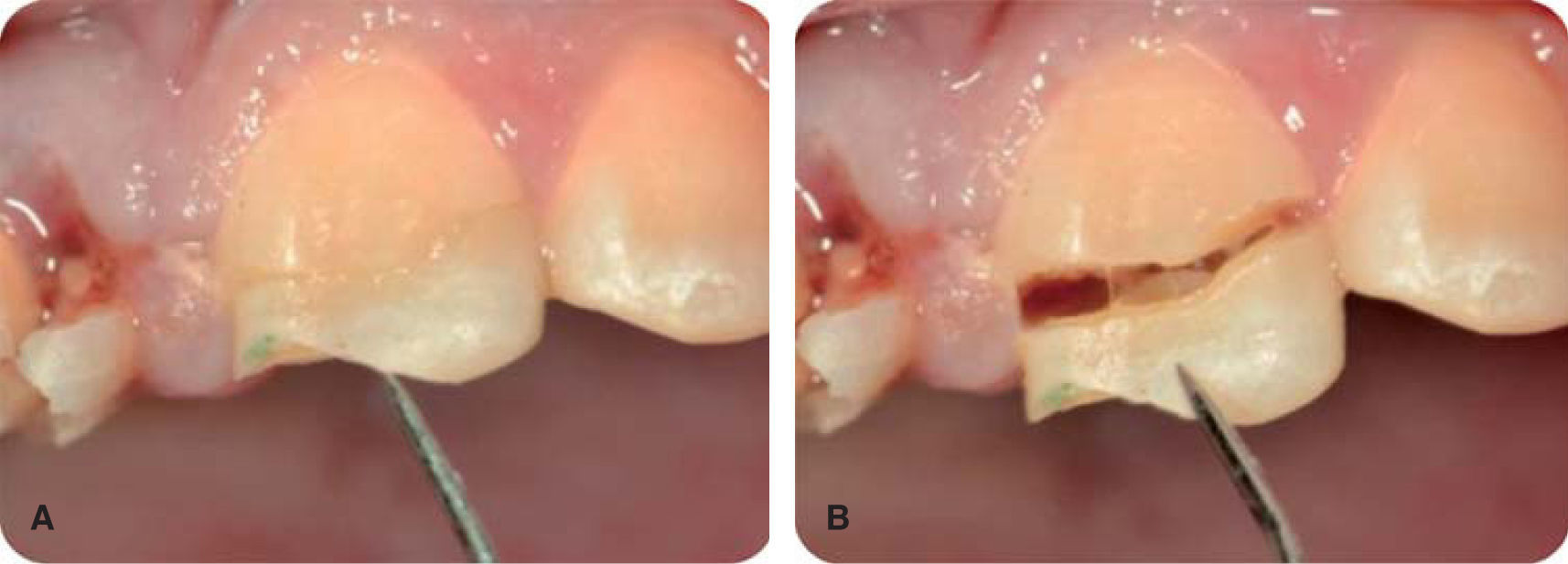
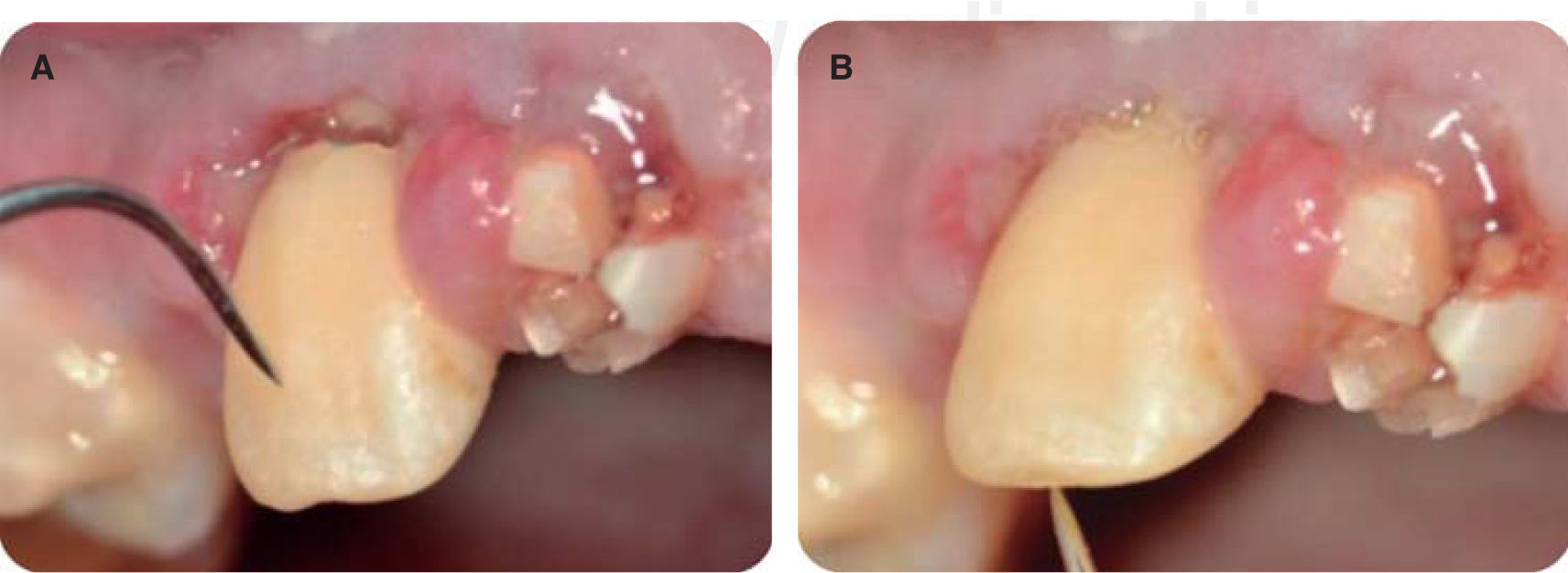
Emergency treatmentEmergency treatment consisted on tooth fragments’ removal (Figures 3 to 6) in order to achieve better visibility of the area and visualize possible treatments. This procedure was conducted under local anesthesia (lidocaine 2%, 1:10,000 epinephrine). Pulpectomy of teeth 12, 11, and 21 was conducted and medication of calcium hydroxide 35% (UltraCal® XS, pH 12.5 Ultradent) was left in place; glass ionomer was used as temporary curing agent (Figure 7).11,12
DiagnosisThe patient exhibited gingival smile, he suffered the following fractures: compound fracture in the crown of tooth 21 at the crown's middle third (Figure 3) and of tooth 12 at the cervical third (Figure 4), compound fracture of crown and root in tooth 11 (Figure 5), gingivitis induced by dental plaque (Figure 7), transposition of teeth 13 and 14, true anodontia of teeth 15, 35 and 45, and presence of primary teeth 55, 75 and 85.
Treatment planPeriodontal phaseInter-consultation with the Orthodontics Department to tailor an inter-disciplinary treatment targeting alignment of tooth 13 and orthodontic extrusion of teeth that suffered TDI.13
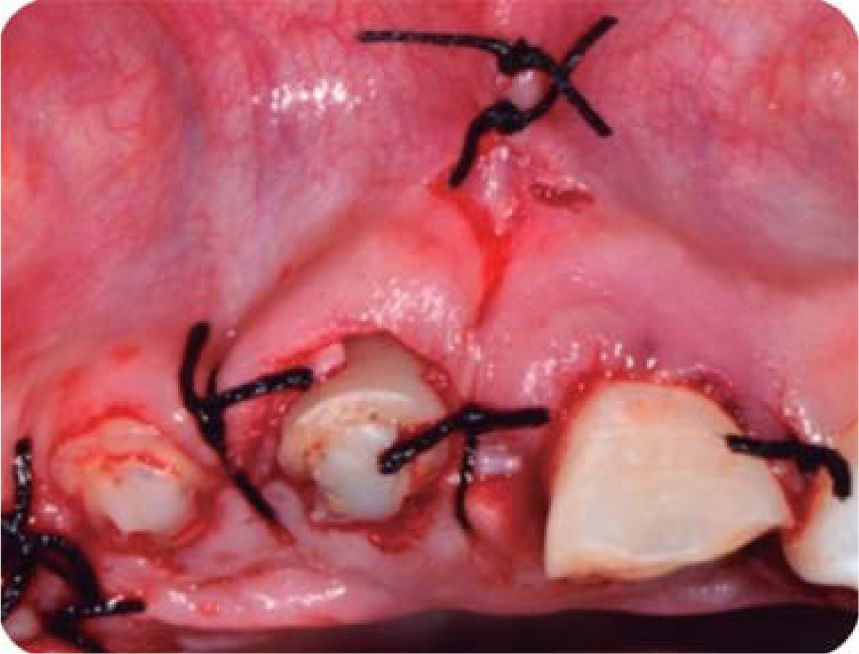
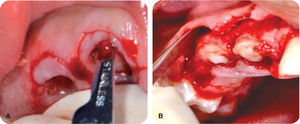
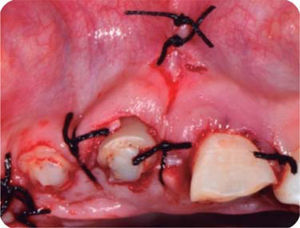
Crown lengthening for endodontic and restorative purposesAn internal bevel incision was performed with a 15 c scalpel blade, after which an incision inside the ridge (intra-ridge) was performed in order to eliminate a collar of gingival tissue and continue raising a full-thickness flap to expose remaining root structure (Figure 8). Measurements were undertaken with a periodontal probe in order to determine the amount of bone tissue to be eliminated with osteotomy and osteoplasty, so as to ensure the necessary splint effect required for provisional restorations. Measurements were taken with a probe to ensure a minimum 3mm osteotomy (Figure 9); suture was achieved with simple stitches (Figure 10).14
During history taking, the patient revealed that his upper central incisor teeth suffered diastema, thus, during surgery the upper labial frenulum exhibiting low insertion was released with a frenilectomy (Figure 10).15
Canal system treatmentOnce the crown lengthening surgery had healed, more dental structure was available; this facilitated and ensured isolation to shape canals with manual instruments (K-FlexoFile, Dentsply Maillefer) and balanced forces (Figure 11). A 5.25% sodium hypochloride irrigation protocol was followed with vertical obturation following Schilder's technique using endodontic cement MTA Fillapex (Angelus®).16–18
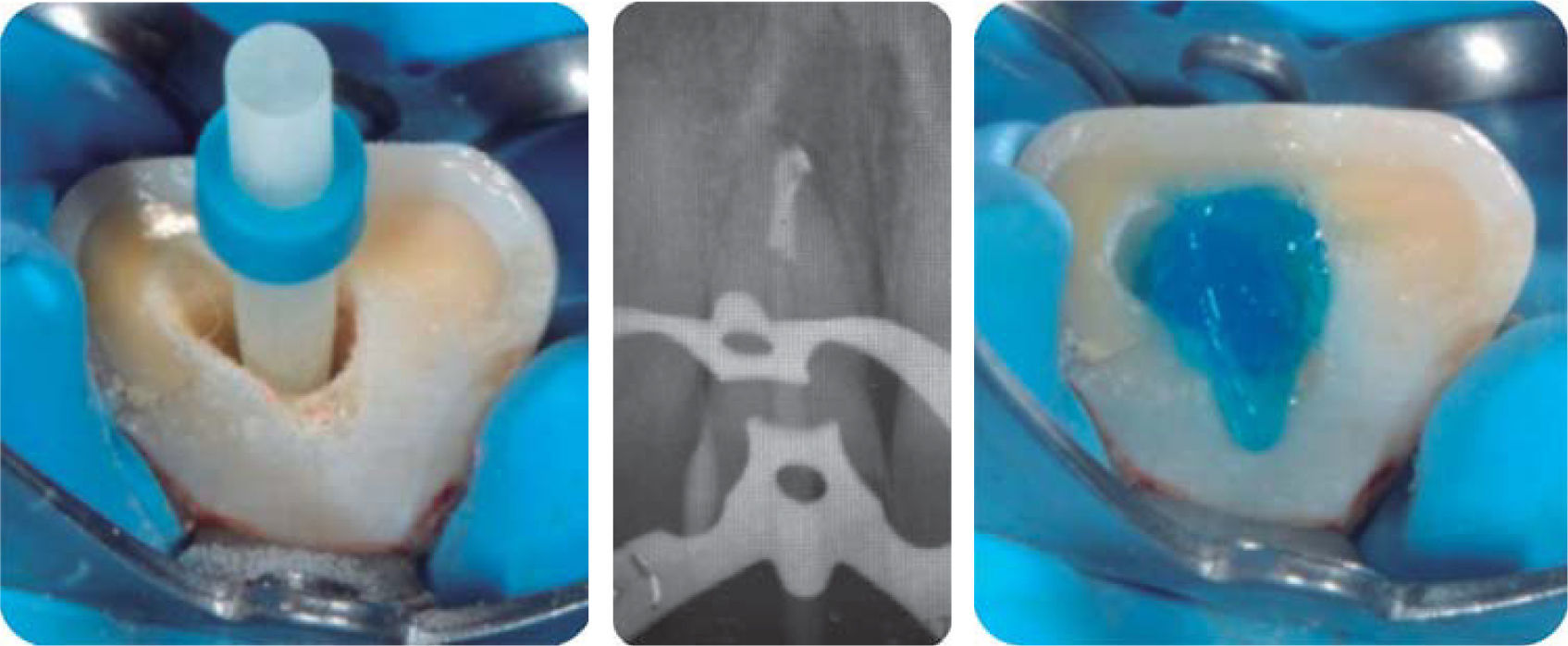
Reconstruction with fiber glass postsUnder total isolation, unblocking, was achieved with Schilder's vertical compaction instruments, de-obturation control x rays were taken and fiber glass posts were fitted (RelyX™ ± Fiber Post® 1.3Ø (diameter) yellow (3M ESPE). Etching was conducted with 37% phosphoric acid for 20seconds, the canal was washed with water spray and dried with paper points; fiber glass endodontic post cementing and crown reconstruction were conducted with resinous cement system Rebilda DC® (VOCO) (Figure 12); control X-ray of cementation was equally taken.19,20 Strictly observing adhesion protocol, once reconstruction and preparation were completed, it was planned to cement long-lasting provisional teeth (Telio Lab, Ivoclar, Vivadent) with glass ionomer so as to achieve patient's comfort and esthetics (Figure 13).21
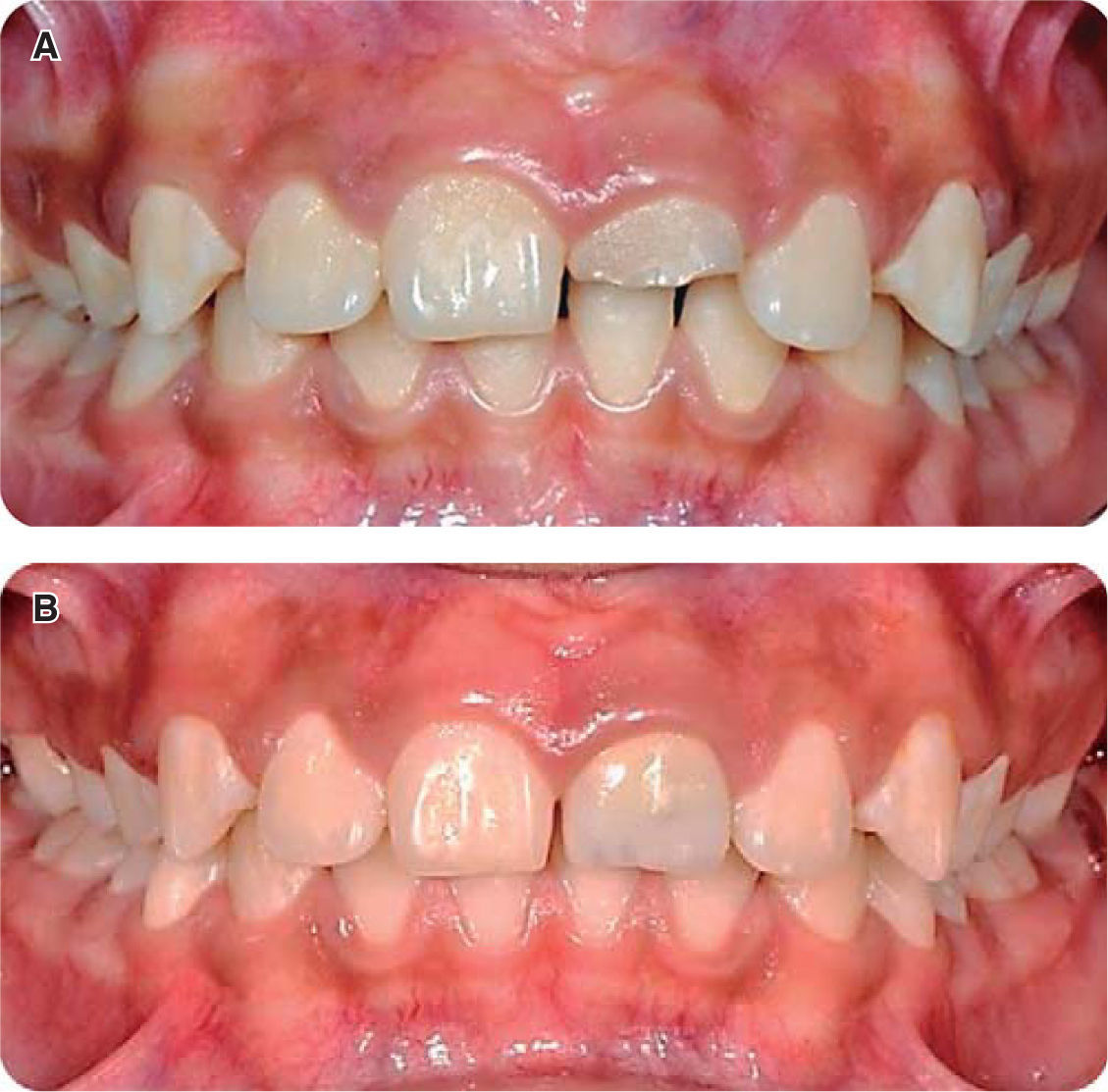
Provisional teeth cementationProvisional teeth were cemented with Ketac™ Cem (3M ESPE) glass ionomer, the patient was then referred to the Orthodontics Department to receive treatment.
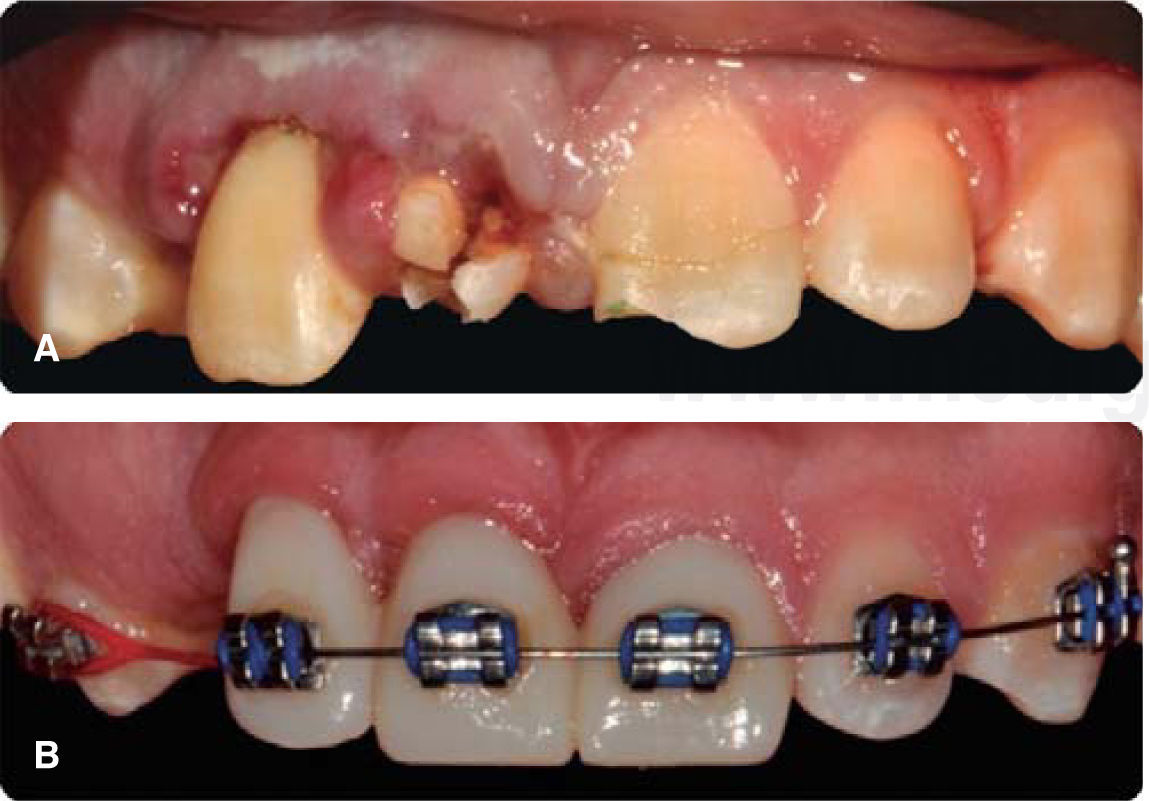
Periodontal control during initiation of orthodontic treatmentThe patient was called to conduct personal plaque control procedures and to receive instructions on tooth brushing with current orthodontic appliances (Figure 14).
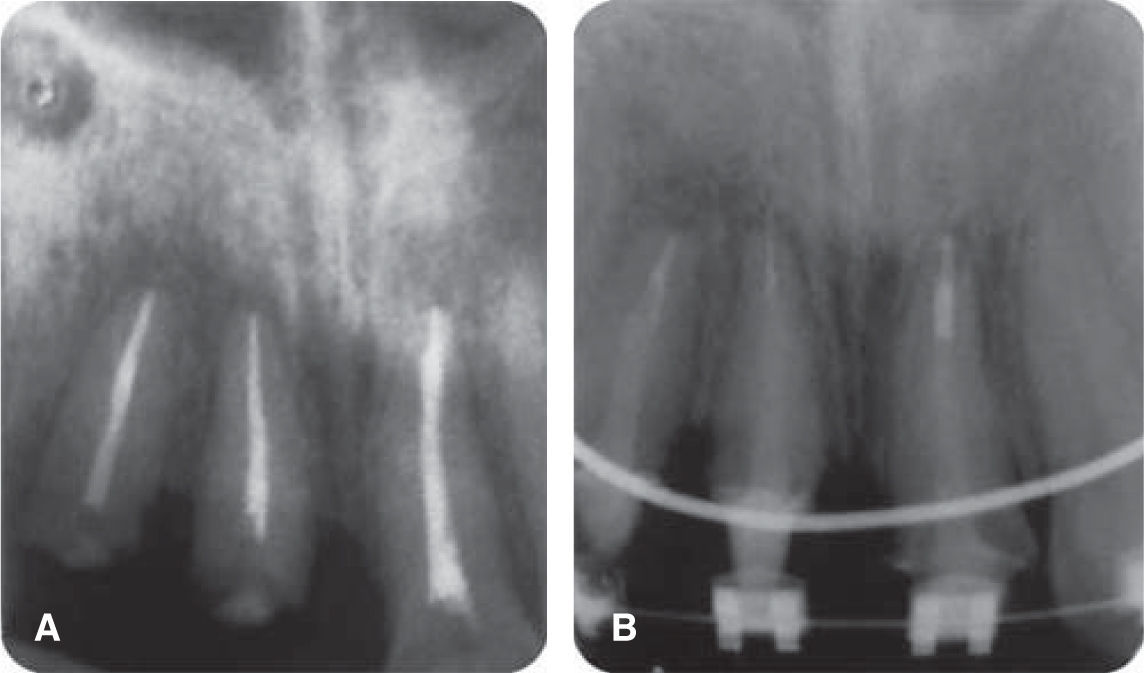
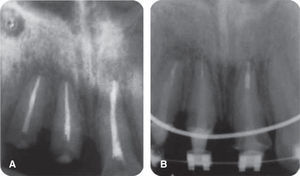
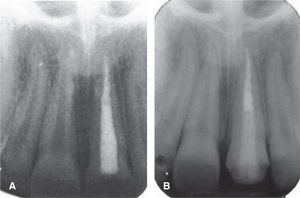
During this periodontal control appointment, dentoalveolar X-rays were taken, which revealed root resorption. This can be attributed to an inflammatory response of the periodontal ligament as reaction to trauma or to orthodontic movements (Figure 15).
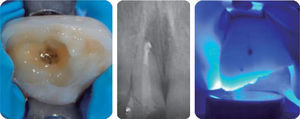
CLINICAL CASE 2A 28 year old male with TDI in the right upper central incisor sought treatment. The injury had been caused when he fainted before a surgical procedure undertaken to remove a tumor in the left kidney. Lesion exhibited a five year evolution.
Extra-oral exploration revealed a scar in the lower lip (Figure 16); the patient informed that he personally had removed the fragment of incisor 11 one day after the TDI.5
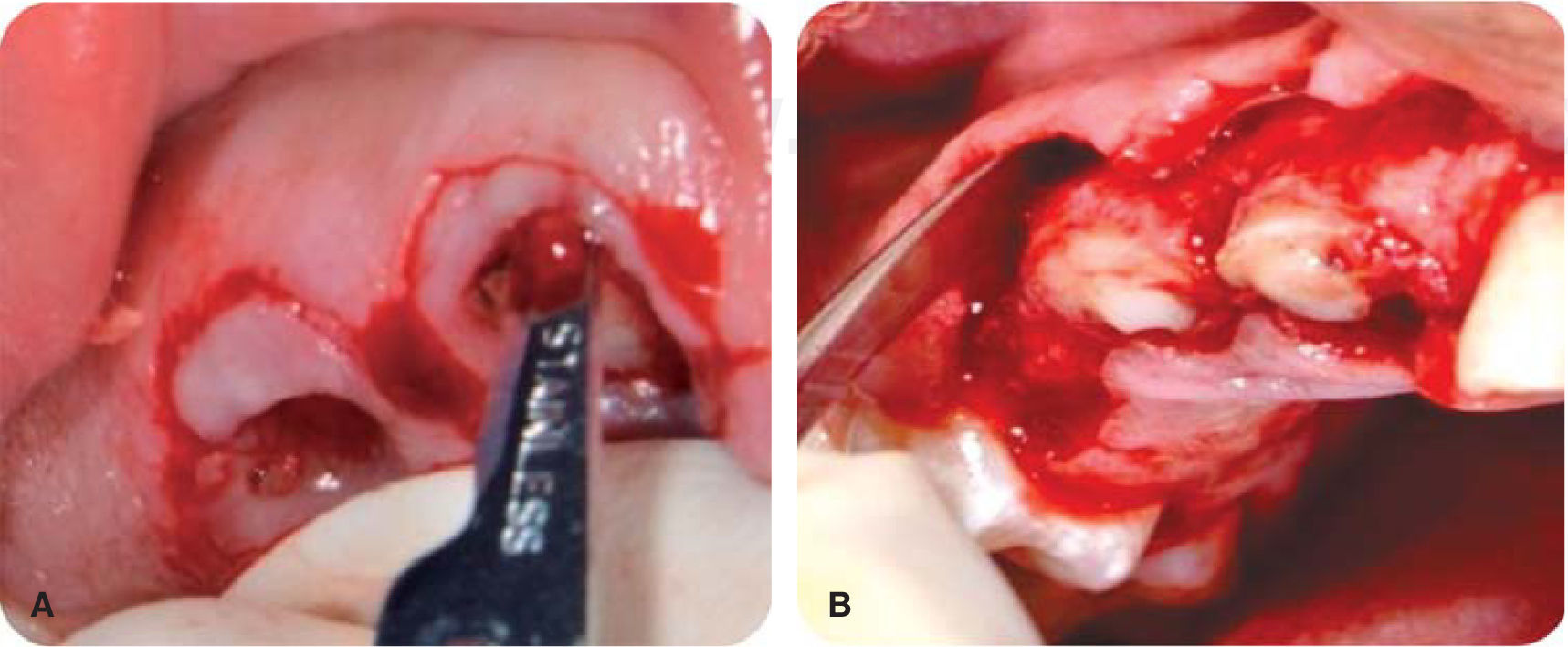
Intra-oral examination revealed a fistulous lesion at the apex of tooth 11, the patient informed of symptoms decrease with the passing of time (Figure 17).
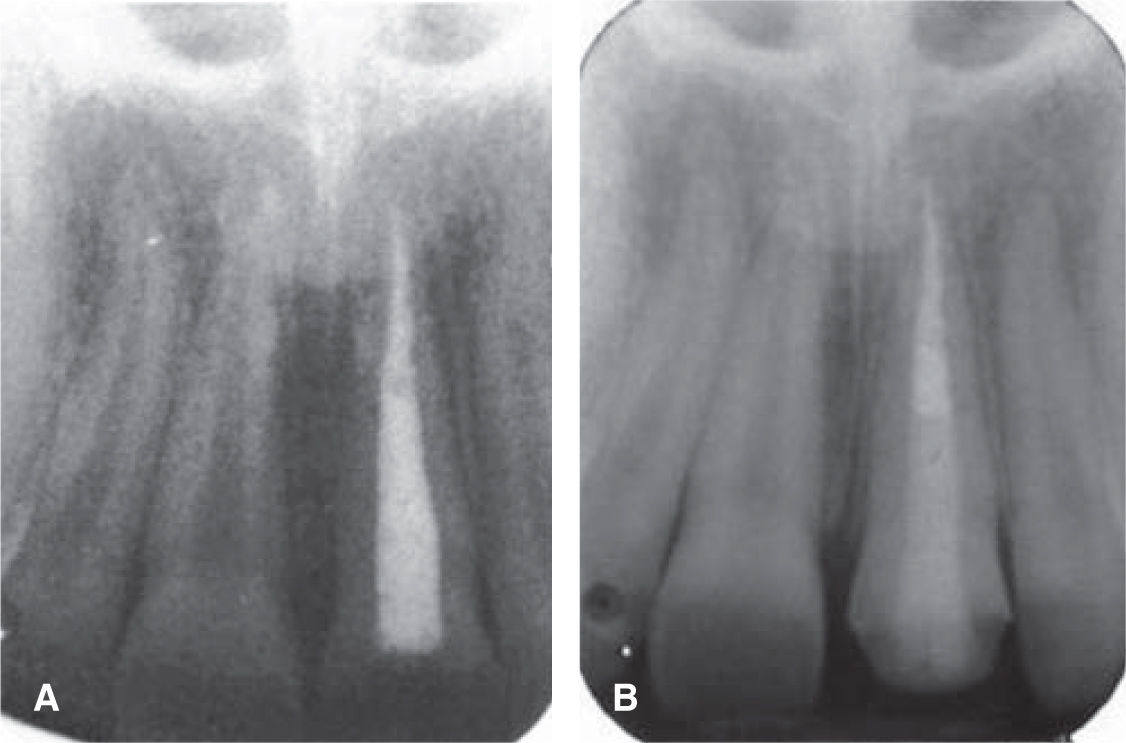
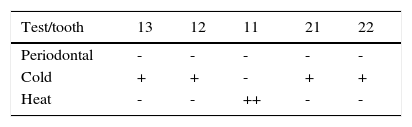
These signs and symptoms (Table I) in addition to radiographic image, confirmed pulp damage of tooth 11.
Diagnosis was as follows: non-compound fracture of tooth 11, with pulp necrosis with suppurative chronic apical periodontitis, gingivitis induced by bacterial plaque and gingival enlargement in tooth 12.
Treatment planPhase 1-periodontalGingivectomy and gingivoplasty of tooth 12These procedures were undertaken in order to generate a new gingival margin and thus conform marginal gingiva (Figure 18).14
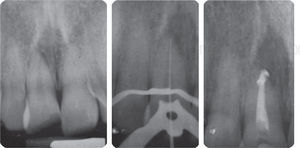
Root canal system treatmentNecropulpectomy of tooth 11 (Figure 19). Apical-crown instrumentation technique (balanced forces)22 with type K manual files (Dentsply® Maillefer) of the second series, protocol of irrigation with 5.25% sodium hypochlorite and lateral obturation technique using endodontic cement MTA Fillapex® Angelus®.17
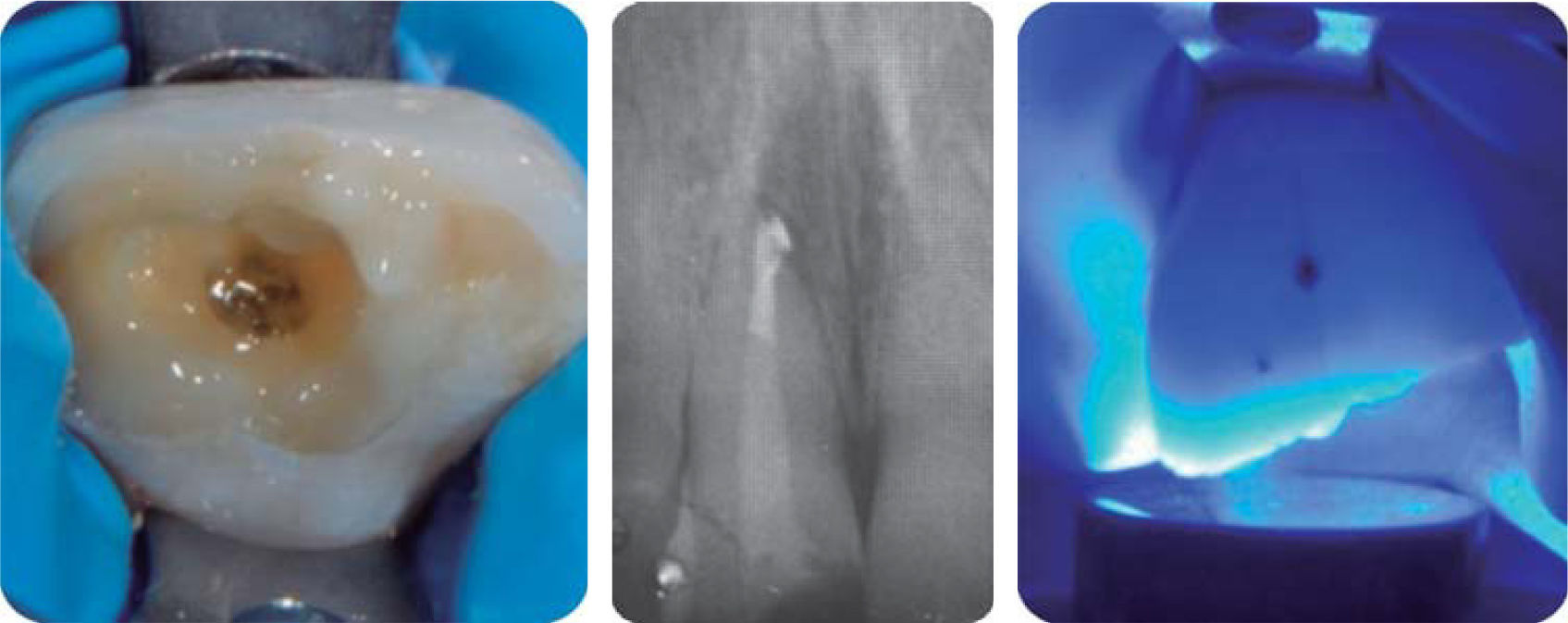
Reconstruction with fiber glass postDe-obturation was conducted under total isolation, using Schilder® vertical compaction instruments. Control X-rays were taken of de-obturation and fit of fiber glass post (Rely Post® 1.90Ø, manufacturer 3M™ ESPE), to continue with procedures of canal etching, washing and drying (Figure 20). This was followed by fiber glass endodontic post cementing and finally, crown restoration was completed with resinous cement system Rebilda® DC (VOCO) and cementation control X-ray (Figure 21).19,20
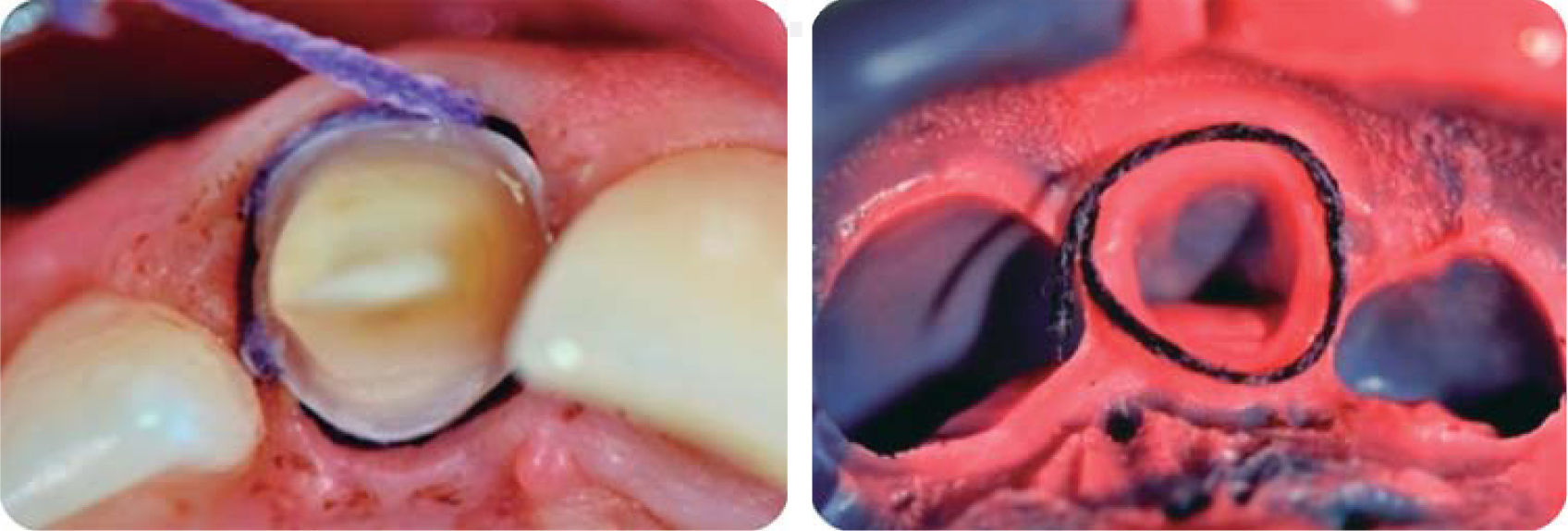
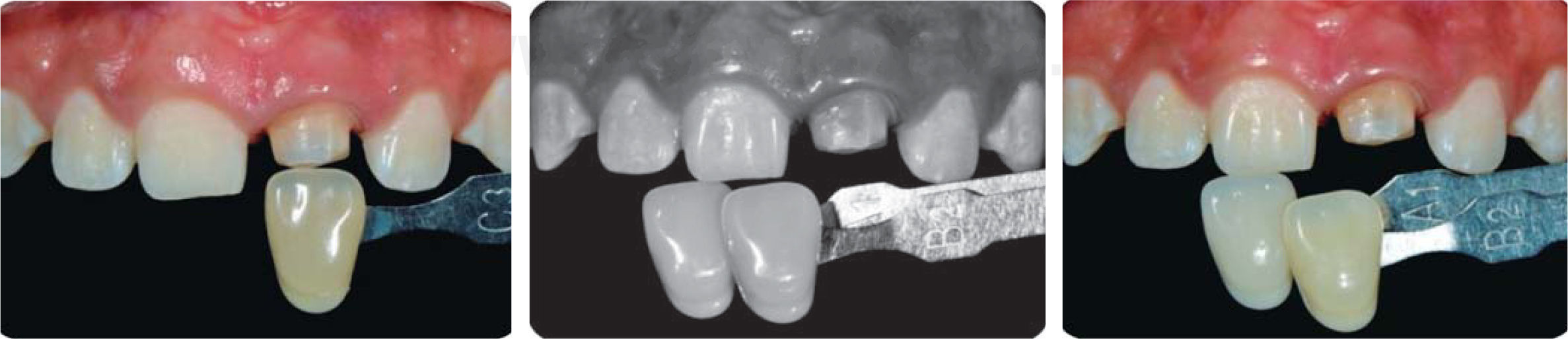
Stump preparationA polyester impression (Impregum Soft® 3M) was taken in order to restore with a lithium23 disilicate crown. Double thread technique was used for gingival separation (Figure 22).24
Color matchingProvisional cementation was achieved with Chromascop colorimeter®(Figure 23) and biacrylic Protemp 4® resin (Figure 24). Provisional cementing was achieved with RelyX Temp® (3M ESPE), with the aim of shaping tissues before cementing final restoration. It is likewise important to point out that color matching was conducted on the preparation stump as well as the homologous tooth so that the technical operator could count with greater information at the moment of stratification and thus create harmony with the choice of tones in the ceramic materials to be used.
Final restorationBefore treatment, and for adhesion protocols, stratified lithium disilicate restoration (IPS e.max®, Ivoclar, Vivadent®) was cemented with Variolink® N; for 20seconds it was etched with 9% hydrofluoric acid, it was then cleansed with a water spray for 20seconds and submerged into a sodium bicarbonate solution to neutralize effect of the acid, afterwards it was washed and dried to then continue with silane application process for 60seconds.25
Chemical onslaught dissolves crystalline structures and allows for blocs’ additional retention with silane and resin cement.23,26
Surface of the preparation was primed with 37% phosphoric acid for 15seconds, it was then washed with water spray, dried, and adhesive ExciTE F DSC was applied in order to continue with the mix of Variolink N base to apply it to the crown, take the crown to its final position removing surplus and polymerizing for 10seconds in order to verify that there is no overflow of cementing material which might compromise periodontal health, to then finish the procedure with a 20 second polymerization (Figures 25A and25B).23
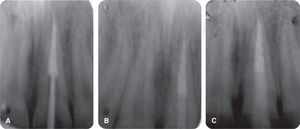
CLINICAL CASE 3A 9 year old patient exhibiting TDI in the left upper central incisor caused by a blow sustained upon falling from his skateboard. During emergency procedures, root canal treatment of tooth 21 was performed.
Intra and extra oral examination only revealed dental fracture (Figure 26). X-rays disclosed root canal treatment (Figure 27).
DiagnosisCompound fracture of tooth 21. Crown X-ray revealed a pulp-less tooth with root canal treatment and absence of periapical lesion. From the periodontal point of view the patient exhibited gingivitis caused by dental plaque (Figure 28).
Treatment planPhase I periodontalReconstruction with fiber glass postDe-obturation with Schilder's vertical compaction instruments, trying to obtain better sealing at the moment of thermo-plasticizing the gutta-percha. A de-obturation control X-ray was taken, taking care that the drill of the used system remains with spaces (Figure 29A), fiberglass post FRC Postec® size 3 (Ivoclar, Vivadent) was adjusted (crown diameter 2mm apical diameter 1mm) (Figure 29B). The fiber glass post was cut in a single event with high speed hand-piece, thick grain diamond burr and abundant irrigation. After this it is etched, washed, the canal was dried and the fiber glass endodontic post was cemented, with its crown section toward the apical section of the canal in order to better match the diameter of a young tooth; apical surplus of the post was introduced as complementary post in the crown aspect of the canal. Cementation and crown reconstruction were achieved with Rebilda® DC (VOCO) resinous cement system. Finally a cementation control X-ray was taken (Figure 29C).
Stump preparationWe observed a particularly conservative protocol; aiming at restoring with cerometer crown (SR Adoro, Ivoclar, Vivadent) an impression was taken with polyvinysiloxane (3M Express®) following double thread gingival separation technique (Figure 30).
Color matching and provisional applianceProvisional appliance was achieved with VITA classical colorimeter and 3M Protemp 4® bi-acrylic resin, the provisional appliance was cemented with RelyX Temp® (3M ESPE) cement, priming tissue before cementing final restoration. It is likewise important to point out that color matching is conducted with the stump of the preparation (Figure 31A) as well as the homologous tooth (Figures 31B and31C).
Final restorationA ceromer was used (Adoro).27,28 The restoration was cemented with Variolink II, color A3; restoration had been previously treated for adhesion protocol, it was primed with 37% phosphoric acid, washed with a water spray for 20seconds, dried to continue with silanizing process for 60seconds (Monobond S, Ivoclar, Vivadent) to facilitate chemical bonding. After cleansing the stump, 37% phosphoric acid gel was applied and allowed to act for 20seconds. The gel was removed with water, excess humidity was eliminated so as to be able to see a non-dehydrated dentin surface (Figure 32).
Enamel and dentin were saturated with abundant amounts of ExciTE DSC, surplus was lightly removed and solvent (alcohol) evaporated in the air.
Surplus of resinous material used in cementation was removed from the restoration while still in partially polymerized or in a soft state. For example, with the help of a single-use brush or dental sponge, Variolink II must be polymerized with a high intensity light (900 mW/cm2); exposition time at this power was 40s per segment (Figure 33).
DISCUSSIONIn dentistry, the most difficult decision is to choose upon the best treatment, that is to say, the decision of restoring one or more upper incisors which have been weakened as a result of TDI.1 An optimum result frequently implies a multidisciplinary approach including areas of periodontics, endodontics and restorative dentistry, making use of inter-consultation with oral and maxillofacial surgeons as well as orthodontists.29–32
Clinical operators act upon this type of TDI seeking to protect the pulp and reconstruct affected tooth morphology. Dental treatment (pulpectomy) is urgent in cases of teeth with closed apexes, with pulp exposition.3,7,10 It must be considered that almost immediately pulp is exposed to bacterial contamination, therefore, treatment must target plaque elimination, chemical and biomechanical preparation to detoxify canal system and achieving three-dimension canal hermetic sealing; all the aforementioned factors are vital in order to ensure treatment success.33–35 When the apex is still open, as is the case in recently erupted teeth, treatment is based on removal of inflamed pulp and preservation of remaining vital pulp (pulpotomy).5,9
Restorative decisions are made and conditioned by the need of periodontal and orthodontic contributory treatments, as well as the patient's age, thus it is important to consider the need for long term provisional restorations made of ceromers, lithium disilicate and zirconium oxide which are all conservative with respect to remaining structures. Metal-porcelain restorations have been considered the gold standard for teeth restorations. They possess suitable mechanical properties, pleasing esthetic results and acceptable biological behavior which are all necessary for periodontal health.36,37 Nevertheless, there are some circumstances that can limit their use, by instance, esthetics are limited by the metallic structure and the opaque porcelain layer required to mask the greyish metallic shadow. Recently, the cost of precious metals has notably increased, thus rendering restorations made of these metals unattractive from the financial point of view.36,38,39
In clinical case 1, crown lengthening was performed so as to achieve dental structure that would allow an ideal absolute isolation. Likewise, when achieving 1mm of cervical-radicular splint effect for restorations when completing lengthening procedures it could be seen that the zeniths were not leveled. Since the patient exhibited high smile and tooth malposition, esthetic zenith leveling was left for orthodontic treatment, to achieve success with forced extrusion.13,14
Gingivectomy a frequently conducted procedure in the dental office, was selected for case 2, as part of periodontal treatment, since the patient revealed history of kidney tumor and thus could be suffering hormonal alterations, this had to be added to his poor oral hygiene which caused a gingival enlargement lesion found in tooth number 12, which was simply eliminated with a gingivectomy procedure.39,40
CONCLUSIONThe smile is a valuable social communication element, thus the existing need for exhibiting healthy, functional, harmonious and esthetic teeth. These parameters are therefore the gaol to achieve in anterior restorations.
TDI located in esthetic areas must be evaluated bearing in mind several aspects, among which we find: type of smile, age, tooth vitality, involved tissues, fracture location and amount of remaining dental structures. In the cases presented in this study a multidisciplinary approach encompassing endodontic, surgical and prosthetic-adhesive treatments provided suitable results inasmuch as preserving structural integrity of the tooth and providing long-term, predictable restorations.
There are many available proposalst to treat this type of TDI. The ideal treatment is frequently the most conservative option offering to meet with functional and esthetic requirements.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam