To evaluate the influence of body position on the displacement of nasal prongs in preterm infants.
MethodsThis prospective, randomized, crossover study enrolled infants born at a mean gestational age of 29.7±2 weeks, birth weight of 1353±280g and 2.9±2.2 days of life, submitted to continuous positive airway pressure by nasal prongs. The main outcome was the number of times that the nasal prongs were displaced following infant positioning in the following body positions: prone, right lateral, left lateral, and supine, according to a pre-established random order. Moreover, cardiorespiratory variables (respiratory rate, heart rate, and oxygen saturation) were evaluated for each body position. Data for each position were collected every 10min, over a period of 60min. An occurrence was defined when the nasal prongs were displaced from the nostrils after 3min in the desired position, requiring intervention of the examiner.
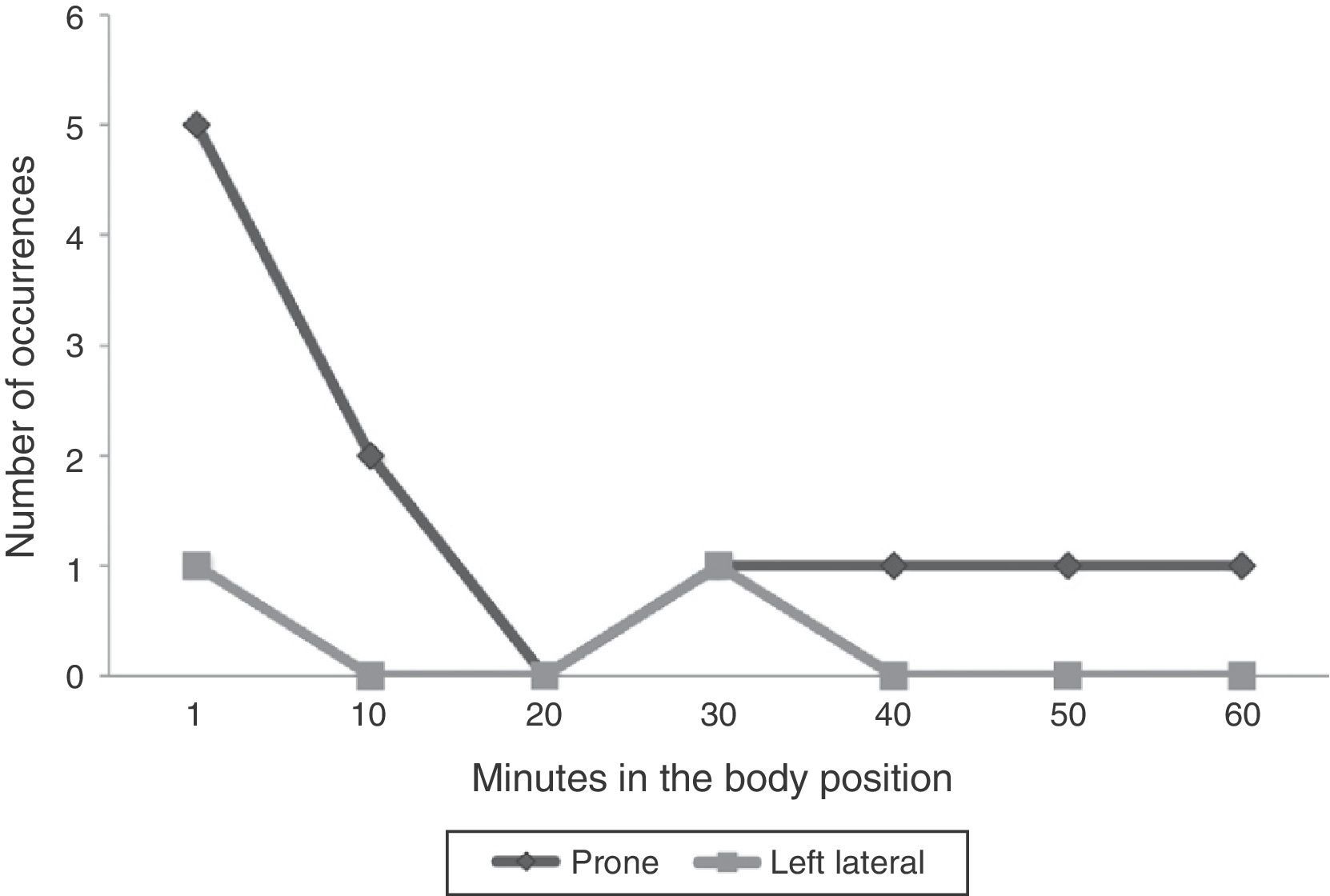
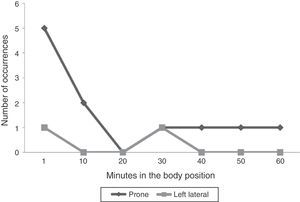
ResultsAmong the 16 studied infants, the occurrence of nasal prong displacement was only observed in the prone position (9 infants – 56.2%) and in the left lateral position (2 infants – 12.5%). The number of times that the prongs were displaced was 11 in the prone position (7 within the first 10min) and 2 in the left lateral position (1 within the first 10min). No clinically significant changes were observed in the cardiorespiratory variables.
ConclusionsMaintenance of the nasal prongs to provide adequate noninvasive respiratory support was harder in the prone position.
Analisar a influência da posição corporal no deslocamento da pronga nasal em recém-nascidos pré-termos.
MétodosEstudo prospectivo, randomizado e tipo crossover. Foram estudados recém-nascidos com média de idade gestacional de 29,7±2semanas, peso de nascimento de 1.353±280g, 2,9±2,2dias de vida e em uso da pressão positiva contínua de vias aéreas. Avaliou-se o número de vezes em que o dispositivo nasal sofreu deslocamento, além de variáveis cardiorrespiratórias, como frequência respiratória, cardíaca e saturação de oxigênio, conforme a criança foi colocada nas posições corporais prona, lateral direita, lateral esquerda e supina, segundo ordem aleatória previamente estabelecida. As informações em cada posição foram coletadas a cada 10minutos, por 60minutos. Foi considerada ocorrência quando o dispositivo nasal se deslocou do orifício das narinas, após o período de três minutos na posição desejada, e houve necessidade de intervenção do examinador.
ResultadosNas 16 crianças estudadas, o deslocamento do dispositivo nasal ocorreu somente nas posições prona (nove crianças – 56,2%) e lateral esquerda (duas crianças – 12,5%). A pronga se deslocou 11 vezes na posição prona, sete delas nos primeiros dez minutos, e duas vezes na posição lateral esquerda, uma nos primeiros dez minutos. Não se detectaram alterações clinicamente significativas nas variáveis cardiorrespiratórias.
ConclusõesA posição prona mostrou maior dificuldade para se manter o dispositivo nasal de suporte pressórico não invasivo na forma adequada.
Nasal prongs are a type of device used in infants receiving noninvasive pressure support through continuous positive airway pressure (CPAP). Nasal CPAP is frequently used in preterm infants at birth or after mechanical ventilation discontinuation.
Some advantages of using nasal CPAP as first choice of ventilatory support have been demonstrated, such as a decrease in the need for invasive ventilatory support, better pulmonary mechanics results and reduced respiratory work.1 This support, when used after tracheal extubation, is indicated by the Brazilian Consensus on Mechanical Ventilation as level “A” of evidence.2 Therefore, the neonatal care team should be encouraged to use the system.
The professional team involved in neonatal care is critical to the success of the nasal CPAP technique. Adequate knowledge of the technique by the team and care directed to the nasal device handling allow the decrease in complications, such as nasal septal lesions, nasal bleedings and inadequate prong positioning.3
Proper positioning of the nasal prongs is the one that does not deform the face, does not compress the nasal septum and does not allow the displacement of the interface inside the nostrils.4 Inadequate positioning of the nasal device generates increasing pressure in the columella, causing reduced blood flow and a consequent risk for ischemia and tissue damage.5 Thus, it is important to pay attention to the positioning of the nasal prongs in a preventive manner, in order to reduce the incidence of nasal lesions induced by the device.6
In order to attain better device fixation and stability on the face and in an attempt to keep the nasal CPAP interface properly and comfortably positioned, several fixation models have been developed. However, scientific studies have not described whether a certain body position could facilitate or hinder the permanence of nasal prongs in the correct place. The body positioning could influence the correct permanence of the prongs, as the adequate body position has shown to be important in certain clinical situations, such as increased gastric volume,7 in cases of apnea8 or for the sleep rhythm9 of the infant.
Therefore, this study aimed to analyze the influence of body positioning on the nasal prong displacement in preterm infants during nasal CPAP use.
MethodThe study design was analytical, prospective, crossover and observational, carried out between January and December 2009. The assessed preterm infants were followed at the Pediatric Intensive Care sector of a tertiary public hospital. The study was approved by the Institutional Review Board, protocol #024/2008. The informed consent forms were shown to and signed by the infants’ parents or guardians.
For inclusion in this study, preterm infants <34 weeks gestational age, weight <2000g and using nasal CPAP in the first week of life were selected. Infants with congenital anomalies, post-surgical cases, those with hydrocephaly, neonatal infection, diagnosed with bronchopulmonary dysplasia and neonates that showed agitated body movements, continuous crying and contracted facial expression demonstrating pain were excluded.
Nasal CPAP was applied using Hudson® (Hudson RCI infant nasal CPAP cannula system, Teleflex Incorporated, USA) siliconized nasal prongs. All newborns received hydrocolloid in the nostrils, keeping the orifices open for the introduction of the nasal prongs. The size of the prongs was chosen based on the reference table provided by the manufacturer, which associates the child's weight with the recommended diameter of the device, with all of the prongs being well adapted to the nostrils.
For nasal CPAP, the gases were humidified and warmed and the fraction of inspired oxygen was controlled by the oxygen blender. The premature infants were stable, requiring a maximum of 30% oxygen and positive-end expiratory pressure (PEEP) no higher than 6cmH2O, with little continuous flow variation from 7 to 8L/min. The mean airway pressure measured at the ventilator did not exceed 7cmH2O.
The infants were placed in the following positions: supine (A), right lateral (B), prone (C) and left lateral (D) position, evaluated according to the criteria of crossover trials.10 Each child was randomly placed in the abovementioned body positions, beginning with the sequence position. The possible sequences of body positions were organized aiming not to repeat the order of decubitus, thus being selected: Sequence 1 (A, D, C, B); Sequence 2 (C, A, B, D); Sequence 3 (B, C, D, A), Sequence 4 (D, B, A, C).
The four sequences were randomized into four groups, so that each selected child was allocated to a sequence of positions according to the previous drawing of lots. The infant remained for 60min in each body position. The study began 1h after feeding, which was offered through an orogastric tube. When the child was fed between the positioning maneuvers, a 1-h interval was allowed for placement in the study position. All infants were followed by the same examiner in order to maintain the same positions for all infants. The body positions that needed cushion support were the left and right lateral positions. During the observation period, the infants were not submitted to any manipulation.
An occurrence was considered when the nasal device was displaced from the orifice of the nostrils after 3min in the desired position, requiring repositioning by the examiner. We analyzed the number of occurrences within 1h of observation of each body position per infant. Moreover, cardiorespiratory variables were observed: respiratory rate, measured by observing the chest for a full minute, heart rate and oxygen saturation, both using the Dixtal-DX2010 monitor with neonatal sensor located at the foot. Data were collected every 10min during 60min, with a total of seven collections for every position.
The sample was selected by convenience, as it is a homogeneous group. However, sample calculation was subsequently employed to estimate the proportion, with permissible estimation error of 5%. The characteristics of the study group were descriptively shown as mean and standard deviation. To compare the occurrence of nasal device displacement, according to body position, the chi-square test was applied to the contingency table related to the occurrence, with p<0.05 being considered significant. To detect possible differences in cardiorespiratory indicators among the four groups, analysis of variance was used for repeated measures, using the software Statistica 7.0.
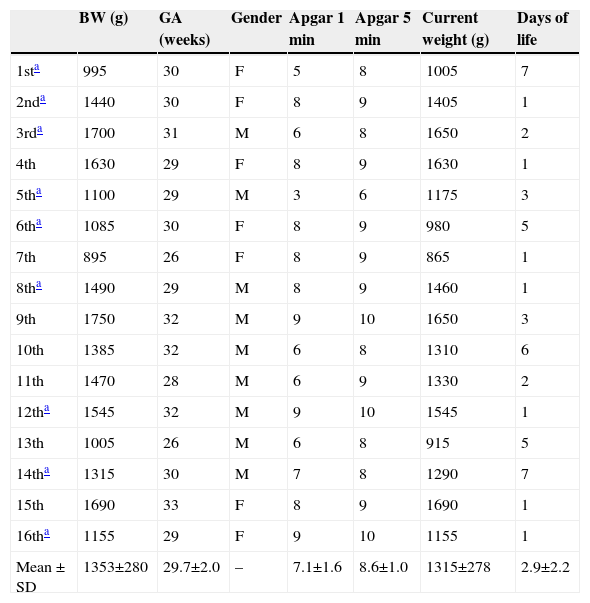
ResultsA total of 19 infants born during the study period met the inclusion criteria and were eligible for the study; 3 were excluded. Two newborns were agitated and cried continuously before data collection started and one, after collection of data on the first body position of the sequence, required venipuncture, becoming agitated. Therefore, we studied 16 preterm infants, who were randomly assigned to each of the four previously established sequences. All infants were appropriate for gestational age and their main characteristics are shown in Table 1.
General characteristics of preterm infants studied.
| BW (g) | GA (weeks) | Gender | Apgar 1min | Apgar 5min | Current weight (g) | Days of life | |
|---|---|---|---|---|---|---|---|
| 1sta | 995 | 30 | F | 5 | 8 | 1005 | 7 |
| 2nda | 1440 | 30 | F | 8 | 9 | 1405 | 1 |
| 3rda | 1700 | 31 | M | 6 | 8 | 1650 | 2 |
| 4th | 1630 | 29 | F | 8 | 9 | 1630 | 1 |
| 5tha | 1100 | 29 | M | 3 | 6 | 1175 | 3 |
| 6tha | 1085 | 30 | F | 8 | 9 | 980 | 5 |
| 7th | 895 | 26 | F | 8 | 9 | 865 | 1 |
| 8tha | 1490 | 29 | M | 8 | 9 | 1460 | 1 |
| 9th | 1750 | 32 | M | 9 | 10 | 1650 | 3 |
| 10th | 1385 | 32 | M | 6 | 8 | 1310 | 6 |
| 11th | 1470 | 28 | M | 6 | 9 | 1330 | 2 |
| 12tha | 1545 | 32 | M | 9 | 10 | 1545 | 1 |
| 13th | 1005 | 26 | M | 6 | 8 | 915 | 5 |
| 14tha | 1315 | 30 | M | 7 | 8 | 1290 | 7 |
| 15th | 1690 | 33 | F | 8 | 9 | 1690 | 1 |
| 16tha | 1155 | 29 | F | 9 | 10 | 1155 | 1 |
| Mean±SD | 1353±280 | 29.7±2.0 | – | 7.1±1.6 | 8.6±1.0 | 1315±278 | 2.9±2.2 |
GA, gestational age in weeks; BW, birth weight in grams; SD, standard deviation.
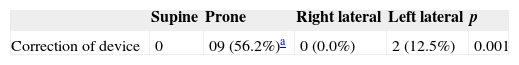
For each evaluation period, we verified the number of corrections of the double nasal prong in infants in different body positions. Table 2 shows the number of infants in whom displacement of the double nasal prong occurred in different body positions, in all assessed periods. The prone position showed a higher incidence of nasal device displacement. In this group, nine children (56.2%) required the intervention of the examiner for the device repositioning. When comparing the occurrence of nasal device displacement between the four postural positions, the prone position showed a greater number of displacements, which was statistically significant (p=0.001) when compared to the other positions. In the first 10min of observation, there were seven displacements in the prone position in seven infants and one in the left lateral position. In total, there were 11 device displacements in the prone position and 2 in the left lateral position (Fig. 1).
Number of newborns requiring re-position of the nasal device during the seven observations for each evaluated decubitus.
| Supine | Prone | Right lateral | Left lateral | p | |
|---|---|---|---|---|---|
| Correction of device | 0 | 09 (56.2%)a | 0 (0.0%) | 2 (12.5%) | 0.001 |
p value according to chi-square test.
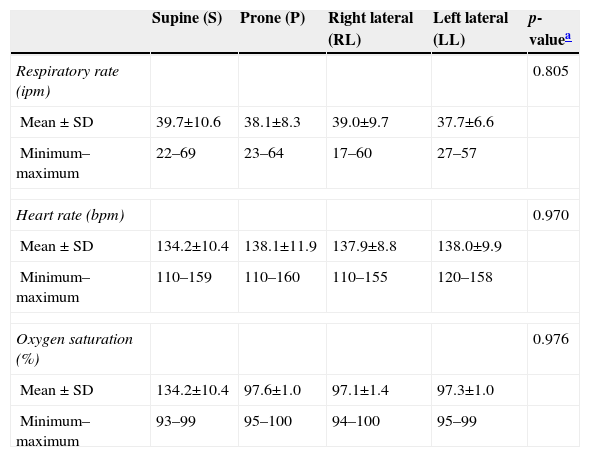
The mean values found for the cardiorespiratory indicators in the four body positions were within the expected normal range. The difference between the minimum and maximum values of respiratory rate was 30–47 inspirations; for heart rate, 38–50 beats per minute and for oxygen saturation, of 4–6%. The lowest variations were observed in the left lateral position. There were no differences between the cardiorespiratory results at the seven times observed with the different groups (Table 3).
Cardiorespiratory variables and interaction between body positions and time from 11 preterm infants that required correction of the nasal device, in mean±standard deviation (minimum and maximum values).
| Supine (S) | Prone (P) | Right lateral (RL) | Left lateral (LL) | p-valuea | |
|---|---|---|---|---|---|
| Respiratory rate (ipm) | 0.805 | ||||
| Mean±SD | 39.7±10.6 | 38.1±8.3 | 39.0±9.7 | 37.7±6.6 | |
| Minimum–maximum | 22–69 | 23–64 | 17–60 | 27–57 | |
| Heart rate (bpm) | 0.970 | ||||
| Mean±SD | 134.2±10.4 | 138.1±11.9 | 137.9±8.8 | 138.0±9.9 | |
| Minimum–maximum | 110–159 | 110–160 | 110–155 | 120–158 | |
| Oxygen saturation (%) | 0.976 | ||||
| Mean±SD | 134.2±10.4 | 97.6±1.0 | 97.1±1.4 | 97.3±1.0 | |
| Minimum–maximum | 93–99 | 95–100 | 94–100 | 95–99 | |
SD, standard deviation; ipm, inspiration per minute; bpm, beats per minute; %, percentage.
The nasal CPAP technique success is directly associated with the adequate use of the nasal device. When the nasal device is displaced from the nostrils, there is need for correction by the health team. Therefore, the team must be very attentive and available for these corrections. The risk of nasal complications increases when the device is not maintained in the adequate position and may cause hyperemia and/or nasal bleeding.11 A body position that results in better adaptation and fewer corrections of the nasal device could improve the technique success and give the team peace of mind.
In the present study, we analyzed the influence of body position on the nasal device adequacy in preterm infants using nasal CPAP. The two body positions that required device correction in the nostrils were the prone (56.2%) and the left lateral positions (12.5%). Regarding the prone position, the CPAP circuit was in direct contact with the bed, as newborns in the prone position remained with cervical rotation to the left side, with the face being supported by the bed. This factor could bring some disadvantages. When the infant moved the cervical spine joint, the bed itself functioned as an obstacle to the device, prompting its displacement. The moment of device displacement was verified, with greater need for correction of the double nasal prong in the first 10min. It is possible that, in the prone position, the compression of the nasal device on the face worked as a stimulus, triggering automatic response movements of the cervical spine and causing displacement of the double nasal prong. After some time, sensory accommodation may have occurred. However, despite the reduction in dislocations, these continued to occur in the prone position during the entire 60min of observation. In the left lateral position, the displacement of the nasal device occurred only in two infants and at different times; thus, there is no justification to associate this position with the occurrence of CPAP displacement.
No study described in the literature has assessed nasal device displacement in different body positions. Rego and Martinez11 evaluated the permanence of the nasal device according to the model used and the child's weight. Newborns weighing between 1500 and 2500g were more difficult to maintain adequately connected to the nasal CPAP (p=0.04), when compared with those whose weight was ≤1000g. The number of times the device was displaced from the nostril per time unit was not associated with the length of stay in nasal CPAP.
Well-positioned nasal prongs without displacement can result in lower risk of nasal injury and ensure less loss of continuous positive airway pressure. Therefore, body position is directly related to factors that interfere with nasal CPAP response. The body position that receives greater emphasis in premature infants is the prone position, which seems to yield best oxygen saturation results. Studies have shown that newborns in the late weaning process responded with increased oxygen saturation when maintained in the prone position.12,13
Heimann et al.8 evaluated episodes of desaturation in 18 preterm infants breathing spontaneously. In the supine position, when compared with the prone, there were more episodes of moderate (between 85% and 80%, p=0.04) and severe desaturation (<80%; p=0.03). The prone and supine positions were also object of study in infants with and without use of supplemental oxygen at postnatal age of 2–10 weeks. The followed group was divided into 10 infants using oxygen therapy (30 weeks; 1.175g) and 10 non-oxygen-dependent infants (31 weeks and 1.589g). The oxygen saturation values in the prone position were higher than in the supine position (p=0.01) in the oxygen-therapy group. The oxygen saturation values remained between 94% and 97% in the prone position and between 94% and 95% in the supine position. Among the non-oxygen-dependent infants, there was no statistical difference (p=0.25).14
In a previous study, we observed that the supine position could be the best choice for premature newborns receiving nasal CPAP. Oxygen saturation and respiratory and heart rate indicators were assessed in the four body positions (prone, supine, right and left lateral positions) in premature newborns using nasal CPAP. The indicators showed similar behavior, not demonstrating a position of preference for preterm infants in stable condition and well adapted to the continuous positive airway pressure system; however, the left and right lateral positions were less beneficial for the oxygen saturation indicator.15 The present study also showed no differences between body positioning and cardiorespiratory indicators assessed in infants that underwent position correction of the nasal device.
It was not possible to identify in the literature other studies that evaluated the occurrence of displacement of the nasal CPAP device in children. The study sample consisted of 16 infants and we consider its low sample power as one of the main study limitations. Additionally, the profile of the selected infants, which were clinically stable and, at the time of observation, were calm and not undergoing any manipulation, may have favored the lower displacement of the nasal device.
This study demonstrated that the prone position is the most difficult one to maintain the noninvasive device of nasal pressure support adequately positioned in premature infants in stable clinical condition. Displacement occurs especially in the first 10min after body positioning.
FundingThis study did not receive funding.
Conflicts of interestThe authors have no conflicts of interest to declare.