To determine the success rate of the manovacuometry test in children between 4 and 12 years of age.
MethodsCross-sectional study involving children and adolescents from 4 to 12 years of age, enrolled in three basic education schools. All subjects had the anthropometric and respiratory muscle strength (maximum inspiratory pressure and maximum expiratory pressure) data measured. Students whose parents did not authorize participation or who did not want to undergo the test were excluded. The test was considered successful when the subject reached acceptability (no air leaks) and reproducibility (variation <10% between the two major maneuvers) criteria established by guidelines. Failure was defined when subjects did not meet the above criteria. Data were expressed as mean and standard deviation and the categorical variables in absolute and relative frequency. The comparison between proportions was performed using the chi-square test.
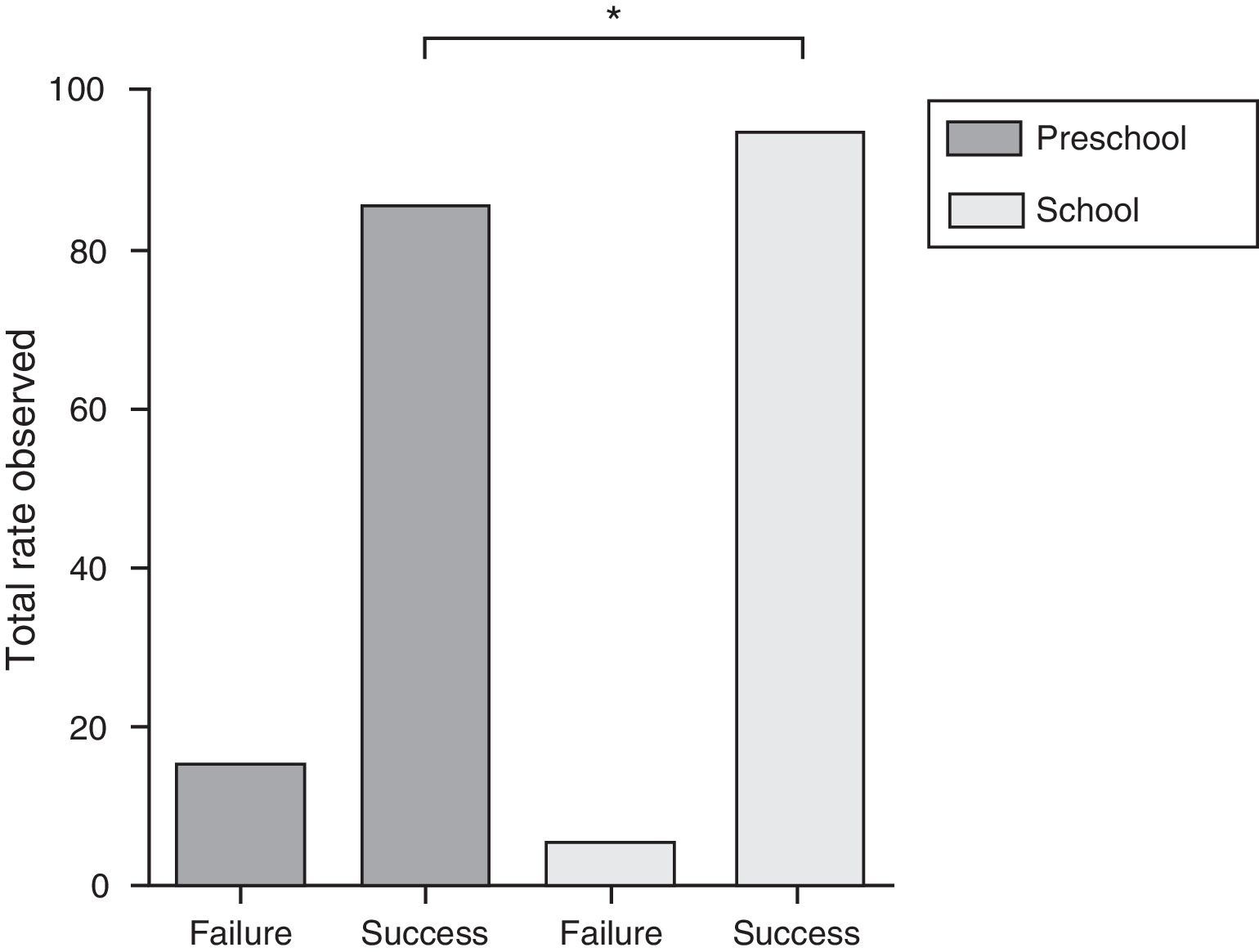
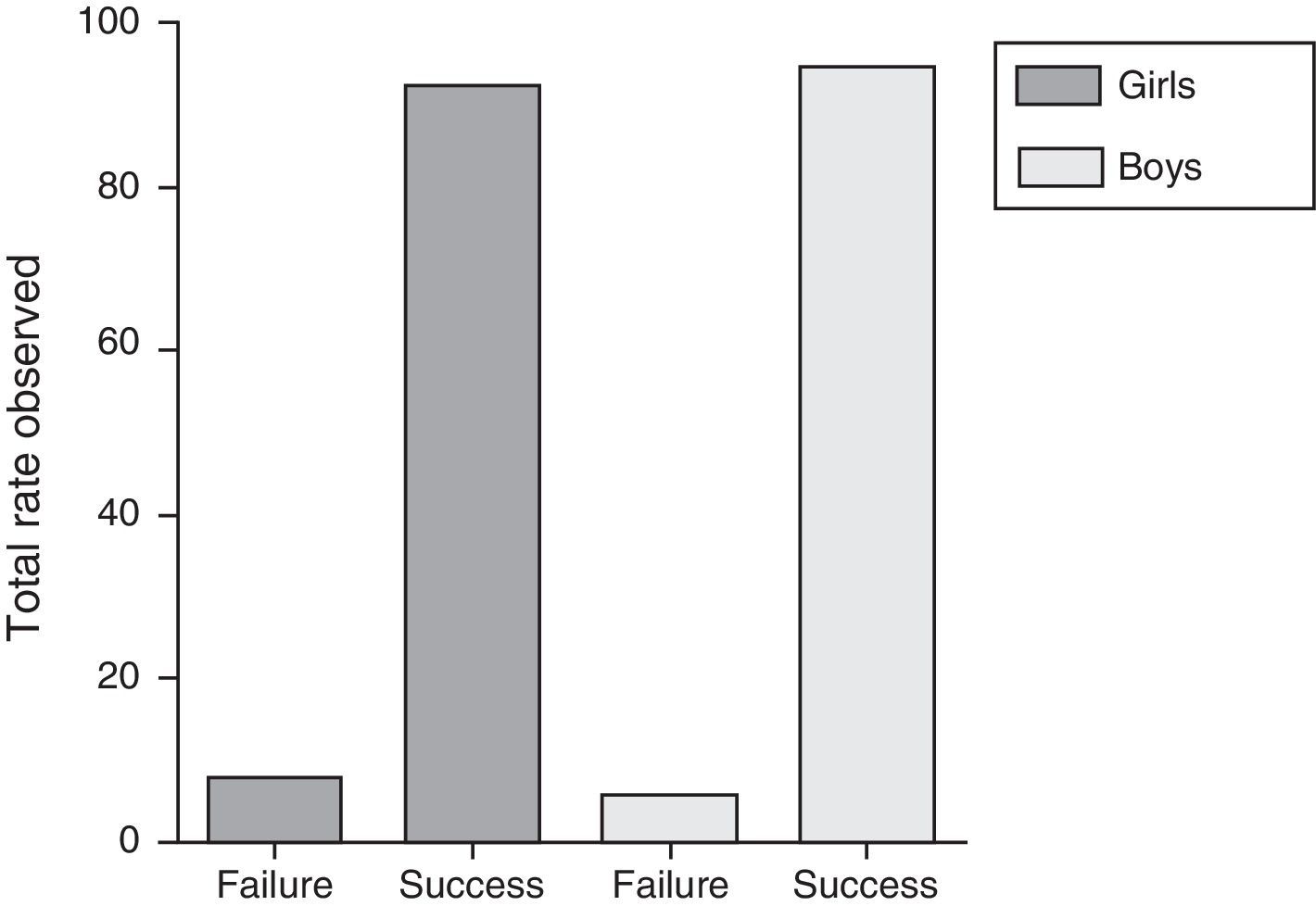
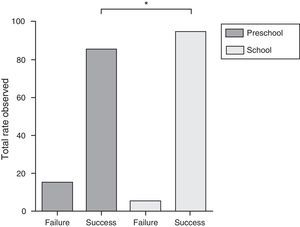
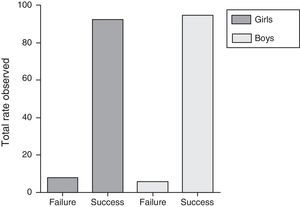
ResultsWe included 196 children and adolescents, mean age of 8.4±2.5 years, 53.1% female. The success rate of the manovacuometry test in children and adolescents evaluated was 92.3%. When comparing the differences between the success rates of preschool children with those children and adolescents of school age, there was a significantly lower success rate in the pre-school (85.1%) group compared to the school group (94.6%) (p=0.032). However, no significant differences (p=0.575) were found when gender comparisons were performed.
ConclusionsThe manovacuometry test showed a high success rate in both preschool and school population assessed. Furthermore, the rate of success appears to be related to aging.
Determinar a taxa de sucesso do teste de manovacuometria em crianças de quatro a 12 anos.
MétodosEstudo transversal que incluiu crianças e adolescentes de quatro a 12 anos, matriculadas em três escolas da rede básica de ensino. Todos os participantes fizeram a mensuração das medidas antropométricas, seguidas do teste de manovacuometria (pressão inspiratória máxima e pressão expiratória máxima). Escolares cujos responsáveis não autorizaram a participação e aqueles que não quiseram fazer o teste foram excluídos. O teste foi considerado sucesso quando o sujeito avaliado atingia os critérios de aceitabilidade (ausência de escape aéreo) e reprodutibilidade (variação <10% entre as duas maiores manobras) estabelecidos pelas diretrizes. O insucesso foi definido como não preenchimento dos critérios descritos acima. Os dados foram expressos em média e desvio padrão e em frequência absoluta e relativa. A comparação entre as proporções foi feita por meio do teste de qui-quadrado.
ResultadosForam incluídas 196 crianças e adolescentes, com idade média de 8,4±2,5 anos, 53,1% do sexo feminino. A taxa de sucesso do teste de manovacuometria em crianças e adolescentes avaliados foi de 92,3%. Quando comparadas as diferenças entre as taxas de sucesso de crianças na faixa etária pré-escolar com crianças e adolescentes na faixa etária escolar, observou-se uma taxa de sucesso significativamente menor no grupo pré-escolar (85,1%), em comparação com o grupo escolar (94,6%) (p=0,032). No entanto, não houve diferença significativa (p=0,575) quando analisadas diferenças entre sexos.
ConclusõesO teste de manovacuometria apresentou uma elevada taxa de sucesso na população pré-escolar e escolar avaliada. Além disso, a taxa de sucesso parece estar relacionada com o aumento da idade.
Although respiratory diseases and other clinical conditions in the pediatric population are some of the main causes of morbidity and mortality in childhood,1,2 many of them have not often been evaluated by objective measures in clinical practice. There are several reasons for this in children, mainly the fact that many tests are not standardized.3 It is difficult for the subjects to understand and cooperate, there is low reproducibility, and also lack of information on certain methods among health care professionals, as part of the evaluation of many lung conditions and diseases.3
In this sense, lung function tests are important tools used to evaluate the respiratory system. They supply objective measures to help diagnose and manage various clinical conditions.3 Among these, the respiratory muscle strength test is a simple, non-invasive resource, easy to apply, and is used to evaluate the maximum static respiratory pressures, which reflect respiratory muscle strength.4 It consists of two measures: one directed at evaluating inspiratory muscle strength through maximum inspiratory pressure (MIP), the other to investigate the expiratory muscle strength through maximum expiratory pressure (MEP).4,5 It is commonly used to determine respiratory muscle weakness and to quantify the severity of certain diseases.4,6 In the pediatric age range, it can help in the management and follow-up of neuromuscular diseases, lung disorders such as asthma and cystic fibrosis, and it is also used in rehabilitation programs.4,7
In clinical practice, respiratory muscle weakness can be associated with hypercapnia, with recurrent infections and inefficient coughing, predisposing to the development of respiratory failure and the onset of more severe morbidities.8,9 Therefore, in the last two decades, studies10–12 have been performed to generate reference values for maximum static respiratory pressures in healthy children and adolescents, in order to make greater use of them in clinical practice, due to the possibility of normalizing and interpreting these respiratory findings. Recently, normality values were published for healthy preschoolers and schoolchildren,10 showing that this evaluation can be performed even in young individuals. The absence of normality values in smaller children has been ascribed mainly to the technical difficulty and the children's lack of understanding while the test is being performed,13,14 demonstrating that the age factor may be the main limitation to evaluating and using respiratory muscle strength in this population group. However, there is as yet no evidence showing how the success rates of the respiratory muscle strength test behave in different age groups.
Therefore, considering the importance of this resource under different conditions and clinical situations, and due to the absence of information about the success rate of the respiratory muscle strength test in the pediatric age group, the purpose of this study was to determine the success rate of the respiratory muscle strength test in children aged 4–12 years old. The use of this evaluative method at early ages may help achieve a better evaluation and follow-up of patients under different situations and conditions in clinical practice.
MethodThis is a cross-sectional, observational study with children and adolescents aged 4–12 years who were regularly enrolled at three basic education schools (two public and one private) in Porto Alegre, state of Rio Grande do Sul, during 2011 and 2012. First, all the children and adolescents were invited to participate in the study, and they received a letter of invitation, together with the free and informed consent form. After the parents and/or guardians had signed and authorized it, they were invited for anthropometric measurements, followed by the respiratory muscle strength test (manovacuometry) at their own school. Students whose parents and/or guardians did not authorize the subjects’ participation in the study, and schoolchildren who did not want to undergo the test on the day when evaluation was performed were not included. The study was approved by the Research Ethics Committee of the Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), under registration number 11/05503. The anthropometric evaluation was performed by measuring weight and height in triplicate, or until two identical values were obtained. Weight was obtained with the individuals in the orthostatic position, wearing a minimum amount of clothes and no shoes, using digital scales (G-Tech, Glass 1 FW, Rio de Janeiro, Brazil) previously calibrated with a 100g precision. Then, height was obtained, with the participants barefoot and feet in a parallel position, ankles joined together, arms extended along the body, and the head in a neutral position. The height was obtained using a portable stadiometer (Altura Exata, TBW, São Paulo, Brazil) with a 1mm precision.
Respiratory muscle strength was evaluated always by the same evaluator (physiotherapist), who presented over a year of previous experience performing the test and who was also trained and supervised by the principal investigator of the study. The test was evaluated using a previously calibrated digital manovacuometer (MVD 300, Globalmed, Porto Alegre, Brazil) with a variation of −300 to +300cmH2O. The instrument was connected to a silicone tube, coupled to an isolating filter and to a connector with an inner diameter of approximately 2.5cm, which was connected to a mouthpiece. The flattish, semi-rigid mouthpiece had an orifice, with a diameter of approximately 2mm to prevent an increase in intra-oral pressure generated by the contraction of the oral cavity muscles.4 Before measuring the respiratory pressures, the technician demonstrated and gave detailed guidance regarding the maneuvers to be performed.
First, MIP was measured from the residual volume, followed by MEP from the total lung capacity.4 While performing the latter measurement, the individuals were told to position their hands on the cheeks to keep air from accumulating on the sides of the oral cavity.15 The measurements were performed with a nasal clip, in a seated position, with the torso erect at a position of 90° to the hip. Both measurements were performed with maximum efforts, at approximately 1-min intervals between the measures, and sustained for at least one second.16 A minimum of three and a maximum of nine measures were used for each test.13 The test was considered successful when the subject performed technically correct maneuvers, including three acceptable measures (without air escaping) and two reproducible ones (variation of less than 10% between the two larger maneuvers). The last value recorded could not be larger than the previous ones,4 and the final result was the highest value obtained. The test was considered inadequate (failure) when the subject evaluated did not reach the criteria of acceptability and reproducibility described above.
The sample size was estimated to detect a failure rate of approximately 10%, with a confidence level of 95% and a maximum acceptable difference of 5%. For that, it would be necessary to include at least 140 individuals. Thus, the sample included in this study surpasses this estimate. Data normality was tested using the Kolmogorov–Smirnov test and presented a normal distribution, so the data were expressed as mean and standard deviation of the mean. The categorical variables were presented in absolute and relative frequency. The comparison between proportions (age groups and gender in relation to the test success rate) was performed using the Chi-square test. All analyses and the data processing were performed using the SPSS software, version 18.0 (SPSS Inc., EUA). In all cases, the differences were considered significant when p<0.05.
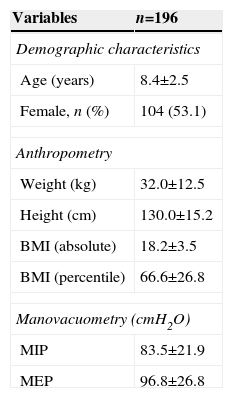
ResultsIn the study, 196 children and adolescents were included, with a mean age of 8.4±2.5 years, weight of 32.0±12.5kg, and 130.0±15.2cm of height; they were predominantly Caucasian (69.4%), and 53.1% were female. The characterization of the sample with the anthropometric data and information on respiratory muscle strength are shown in Table 1.
Characterization of the study sample.
| Variables | n=196 |
|---|---|
| Demographic characteristics | |
| Age (years) | 8.4±2.5 |
| Female, n (%) | 104 (53.1) |
| Anthropometry | |
| Weight (kg) | 32.0±12.5 |
| Height (cm) | 130.0±15.2 |
| BMI (absolute) | 18.2±3.5 |
| BMI (percentile) | 66.6±26.8 |
| Manovacuometry (cmH2O) | |
| MIP | 83.5±21.9 |
| MEP | 96.8±26.8 |
Results presented as mean and standard deviation.
n, total number of subjects evaluated; BMI, body mass index; MIP, maximal inspiratory pressure; MEP, maximum expiratory pressure.
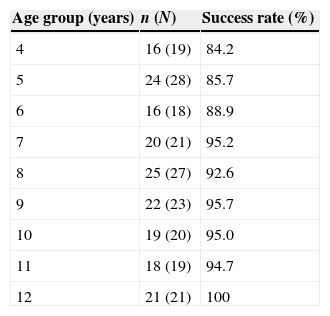
The success rate of the respiratory muscle strength test in children and adolescents evaluated was 92.3%, representing a total of 181 subjects who managed to perform the test adequately. Most of the children and adolescents evaluated are in the age range of the schoolchildren group (6–12 years), 76% of the present sample. In general, the success rate in the test appears to increase according to the age, varying from 84.2% at 4 years of age to 100% at 12 years. The success values for each age group are shown in Table 2.
Success rate of the respiratory muscle strength test according to the age studied.
| Age group (years) | n (N) | Success rate (%) |
|---|---|---|
| 4 | 16 (19) | 84.2 |
| 5 | 24 (28) | 85.7 |
| 6 | 16 (18) | 88.9 |
| 7 | 20 (21) | 95.2 |
| 8 | 25 (27) | 92.6 |
| 9 | 22 (23) | 95.7 |
| 10 | 19 (20) | 95.0 |
| 11 | 18 (19) | 94.7 |
| 12 | 21 (21) | 100 |
n, subjects with a successful test; N, total subjects evaluated.
When the differences between success rates of children in the pre-school age range (4 and 5 years) and children and adolescents in the school age range (6–12) were compared, a significantly lower success rate was seen (p=0.032) in the pre-school group (85.1%), compared to the school group (94.6%) (Fig. 1). Differences in the success rates were also analyzed according to gender. However, there was no significant difference (p=0.575) when the success rates between boys and girls were compared (Fig. 2).
In this study, the success rate observed in children and adolescents evaluated was 92.3%. This shows that the respiratory muscle strength test is a simple resource, easy to apply and highly feasible in this age group. Further, it is a non-invasive method that supplies important information about the function of the respiratory muscles implicated in the breathing process, that are often involved in and/or at a mechanical disadvantage under several conditions or clinical situations, as in lung and neuromuscular diseases.4,5
To the best of our knowledge, this is the first study aiming to determine the success rate of the respiratory muscle strength test in different age groups of the pre-school and school population, which makes it difficult to compare the values found in those of other studies. In any case, considering other lung function tests, we believe that the success rate found in this study is high. Possible contributing factors include a higher level of explanation to the subjects evaluated, a longer measurement time and patience of the evaluator responsible for performing the tests.10 Differently from spirometry, in which specific standards and guidelines were developed to allow its use in younger age groups,17 to evaluate the respiratory muscle strength in this study it was not necessary to use any methodology different from that published by the guideline,4,13 suggesting that it is not difficult to perform the test in these age groups in the clinical practice. When we compared our results to the success rates of the spirometry test, the respiratory muscle strength test is also easy and simple, since the spirometry success rates are close to the results shown here, around 85%.18–21 Additionally, a review of recent literature has shown that although the preschool age group is characterized as an extremely young sample, with its difficulties and motor limitations, the success rate of the spirometry (regardless of previous experience) ranged between 71% and 92%, demonstrating the feasibility of pulmonary evaluation in this age group.22 Although both tests have different methodologies, objectives and functionality, the comparison with a well-known and extensively studied lung function test may indicate a parameter until further success rates are generated for the evaluation of pediatric respiratory muscle strength.
As expected, the success rates of the respiratory muscle strength test appear to increase with the age of the children evaluated. In addition, when compared to the variable sex, no significant difference was found. These findings are similar to those found in various studies that evaluated the lung function success rates in the pediatric population, showing that as the children grow older, the success rate also rises.21,23,24 Previous studies that aimed at generating normality values for the respiratory muscle strength test ascribe the failure of the technique to the difficulty in understanding, low reproducibility and lack of cooperation by the children in this age group.13,14 However, these studies have not demonstrated success rates separately by age groups, hindering a better knowledge and understanding of the age as an influencing factor on this outcome. In this sense, several studies that evaluated the frequency of success of the spirometry test have shown that, in preschoolers, the difficulty of obtaining an adequate test may be explained as being due to reduced attention, easy distraction, difficulty in understanding, motor coordination, and low tolerance for frustration during maneuvers. Besides, the child's emotional stage and stage of development are important factors in determining the success of the test.18,25
Although the present study does not show information about the previous respiratory history of the subjects included, it is believed that those factors would not influence the ability of an individual to perform the test, which was the main outcome of the study. Also, it is unlikely that severe respiratory conditions that could possibly alter the performance of the test would be present in such a young, healthy sample, recruited at a school environment, and with normal nutritional status. On the other hand, even if that is possible, previous studies26,27 have shown that mild to moderate asthmatic subjects do not present respiratory muscle strength reduction, which is usually associated with more severe lung disease, including the presence of hyperinflation and poor nutritional status.28,29
One of the limitations of this study is that the test is performed by an experienced evaluator, who is interested in achieving as much success as possible in the tests, which may have contributed to the high success rate found in this sample. However, these findings only strengthen the idea that it is possible to perform this test in the pediatric age range, and that at least in part, achieving success depends not only on the children and/or adolescents evaluated, but also on the effort and stimulus supplied by the evaluator. In this sense, a previous study30 recently demonstrated that the quality of spirometry tests increased from 57% to 83% after the inclusion of a training program conducted by telemedicine in 15 participating centers. New studies concerning the frequency of success in the pre-school age group should be encouraged to obtain new information about the behavior of success rates in this age group, enabling comparisons among studies and helping to achieve greater use of this resource among the child population.
In brief, the respiratory strength test presented a high rate of success among the pre-school and school population evaluated. Besides, the success rate appears to increase with age. The findings of this study show that the respiratory muscle strength test is a simple and easy to apply resource. Thus, obtaining an adequate test may ensure the quality of the measurements and consequently, success in the control and follow-up of the outcome of different respiratory involvements.
FundingThis study did not receive funding.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank FAPERGS for the scholarship (JPHF).