To determine the prevalence and the severity of wheezing in the first year of life for infants who live in Santo André, São Paulo, Brazil.
MethodsCross sectional study with the administration of the Estudio Internacional de Sibilancias en Lactantes (EISL), which is a standardized and validated written questionnaire applied to parents and/or guardians of infants aged 12-24 months treated at primary health units, vaccination centers, day care centers, or kindergartens. The questionnaire consisted of questions regarding demographic characteristics, presence of wheezing, respiratory infections, and risk factors. Results were analyzed using the SPSS for Windows, 20.0 (SPSS Inc. – Chicago, Il, United States). Logistic regression was applied to verify variables associated to recurrent wheezing.
ResultsAmong the 1,028 infants studied, 48.5% had one or more episodes of wheezing during the first 12 months of life (wheezing once), and 23.9% had three or more episodes (recurrent wheezing). Nocturnal symptoms, severe breathing difficulty, and visits to the emergency room were observed in 67.3%, 42.4%, and 60.7% of infants, respectively. Among the studied infants, 19.4% were hospitalized, and 11.0% had a medical diagnosis of asthma in the first year of life. Use of β2-agonists, inhaled corticosteroids, oral corticosteroids, and leukotriene receptor antagonists were observed in 88.8%, 21.0%, 54.9%, and 3.2% of children with wheezing, respectively. Use of oral corticosteroids, perception of breathlessness by parents, diagnosis of asthma, pneumonia, and hospitalization for pneumonia were more frequent among infants with recurrent wheezing (p<0.001).
ConclusionsIn the city of Santo André, approximately half of infants had at least one episode of wheezing in the first year of life, and almost 25% had recurrent wheezing. Wheezing disorders in Santo André have early onset and high morbidity.
Verificar a prevalência e a gravidade da sibilância no primeiro ano de vida em lactentes no município de Santo André.
MétodosEstudo transversal com aplicação de questionário escrito, padronizado e validado do estudo EISL (do espanhol: Estudio Internacional de Sibilancias en Lactantes) aos pais e/ou responsáveis por lactentes de 12 a 24 meses de idade, em unidades básicas de saúde, durante campanhas de vacinação em creches e escolas maternais. O questionário consiste de questões sobre características demográficas, presença de sibilância, infecções respiratórias e fatores de risco. Os dados obtidos foram analisados com o Statistical Package for the Social Sciences for Windows, versão 20.0 (SPSS inc., Chicago, Il, EUA). A regressão logística foi aplicada para analisar as variáveis associadas à presença de sibilos recorrentes.
ResultadosDo total de 1.028 lactentes estudados, 48,5% apresentaram um ou mais episódios de sibilância nos primeiros 12 meses de vida (sibilância alguma vez) e 23,9%, três ou mais episódios (sibilância recorrente). Sintomas noturnos, dificuldade intensa para respirar e visitas à emergência estiveram presentes em 67,3%, 42,4% e 60,7% dos lactentes, respectivamente, sendo que 19,4% foram hospitalizados e 11,0% tiveram diagnóstico médico de asma. O uso de β2–agonistas, corticoides inalatórios, corticoides orais e antagonistas do receptor de leucotrienos foram observados em 88,8%, 21,0%, 54,9% e 3,2% das crianças com sibilância, respectivamente. Uso de corticoide oral, percepção de falta de ar pelos pais, diagnóstico de asma, pneumonia e hospitalização por pneumonia foram mais frequentes entre os sibilantes recorrentes (p<0,001).
ConclusõesNo município de Santo André, cerca da metade dos lactentes estudados apresentava pelo menos um episódio de sibilância no primeiro ano de vida, e metade deles apresentou sibilância recorrente, com início precoce e alta morbidade.
Allergic disorders are one of the major health problems of modern societies; among them, asthma is the most common chronic disease of childhood,1 and is associated with high rates of hospitalization, visits to emergency services, and significant morbidity, responsible for considerable impact on public health systems.2
Asthma is an inflammatory disease that increases airway response to certain stimuli and reversible bronchial obstruction with or without treatment, characterized by symptoms such as recurrent wheezing, dyspnea, and cough. In children younger than 5 years, it may be confused with other diseases.3
Wheezing is a common clinical finding in children, especially in the first years of life. Epidemiological studies have shown a high prevalence of wheezing in this age group. Studies in developed countries have shown prevalence between 20% and 30%, with high recurrence of episodes.4,5 In developing countries, prevalence rates appear to be higher. In a cohort in Chile, 188 newborns were followed for up to one year of age, and wheezing episodes were identified in 80%, whereas recurrence was observed in 50%.6
Recently, the European and American Academies of Asthma, Allergy, and Immunology published a consensus on wheezing in infants describing four distinct wheezing patterns during childhood, as well as its evolution.3 They are: transient wheezing (wheezing during the first three years of life and discontinuation after this age); non-atopic wheezing (wheezing triggered mainly by viruses that tends to disappear with age); persistent asthma (wheezing associated with clinical manifestations of atopy, eosinophilia, and/or increased total serum levels of IgE or proven sensitization to food and/or aeroallergens, or having a father and/or mother with asthma); and severe intermittent wheezing (occasional acute wheezing episodes associated with few symptoms besides acute conditions and with the presence of atopy characteristics).3
The International Study of Asthma and Allergies in Childhood (ISAAC) protocol proposed a unique method of research and allowed for maximizing the significance of epidemiological research on asthma and other allergic diseases in childhood, as well as supporting international collaboration.7
In Brazil, a cross-sectional study conducted in São Paulo found a prevalence of recent wheezing (one or more episodes in the past 12 months) of 11% among children aged 6-11 months, and 14.3% among those aged 12-23 months.7 In the same city, a cohort of children at high risk for developing asthma showed that, after 30 months of follow up, 52% of these patients had recurrent wheezing.8
The Estudio Internacional de Sibilâncias en Lactentes (EISL), an international multicenter study, was created to compare the prevalence of wheezing in infants with the participation of Latin American countries (Brazil, Chile, Colombia, Mexico, and Venezuela), the Netherlands, and Spain in its first phase. As in the ISAAC study, a written questionnaire (WQ) was prepared and validated in each participating country in order to obtain reliable data on wheezing in infants.9,10 The standardized EISL WQ consists of 45 questions about demographic characteristics, wheezing and other respiratory symptoms, use of medications, medical diagnostics, and potential risk factors, to be answered by the infant's parents or guardians.11
The municipality of Santo André is located in the metropolitan region of São Paulo, which includes a group of municipalities known as Great ABC. It has a population of 673,396 inhabitants (2009 estimate), and occupies an area of 175 km², resulting in a demographic density of 3,816.52 inhabitants/km².12 The climate is subtropical, humid mesothermal and, according to the climate classification of Köppen-Geiger, Cfb type (warm, humid summers, and mild winters). The mean annual temperature is around 19 ºC.12 The region's economy is mainly represented by the industrial sector. In this context, this study aimed to describe and evaluate the prevalence and severity of wheezing in infants in the city, using the EISL standardized questionnaire validated for the Portuguese language, as there are other studies conducted in several Brazilian municipalities.
MethodsThis was a cross-sectional study performed between 2006-2010 in the city of Santo André. Parents or guardians of 1,028 infants from different social classes, who lived in the municipality, were interviewed and answered the WQ. To perform the study, the EISL coordinators determined that the sample should include at least 1,000 infants. The sample size was based on the International Study of Asthma and Allergies in Childhood (ISAAC), considering a prevalence of wheezing of 30% and 25% in two different centers, with a 95% power and a significance level of 1% for this sample, to ensure proper comparisons between the centers and countries, even for questions with a low prevalence of positive answers.11
Children whose parents reported chronic diseases that had an effect on the respiratory system (neuropathies, myopathies, heart diseases, genetic disorders, and severe malformations), as well as those whose questionnaire completion was below 90%, were excluded.
The questionnaire, originally in Spanish, was previously translated into Brazilian Portuguese and validated.13,14 The chosen age range was 12 to 24 months, due to the difficulty in completing the study with infants up to 15 months, and considering the previous validation for the extended range up to 36 months.10
The interviews were conducted in ten basic health units (approximately half of the city's network) during three vaccination campaigns in four public daycare centers and four private centers. Before applying the WQ, parents or guardians were informed of the study objectives, and those who agreed to participate signed the informed consent. Subsequently, they were interviewed by trained researchers.
The WQ-EISL contains 45 questions about demographic characteristics, wheezing, respiratory diseases, pneumonia, and personal and family history, as well as other risk factors.11 In addition, there are questions regarding the use of inhaled medications for relief of symptoms and their frequency, medical diagnosis of asthma, age of onset and frequency of upper airway infections, presence of lower airway infections, individual or family presence of atopy, duration of breastfeeding, immunization, and exclusive breastfeeding time.11 It also contains data on identification, anthropometric measures, environmental conditions, whether the child attended day care and initial age of attendance, presence of pets, environmental pollution, number of siblings, educational level, and ethnicity.15
The wheezing infants were separated by gender, number of wheezing episodes, and asthma diagnosis. Those who had at least one episode of wheezing were evaluated according to gender regarding the frequency of wheezing, presence of symptoms, use of medications and diagnosis of asthma, pneumonia and airway infections, and type of treatment.
The results obtained were transferred to a database, developed in Microsoft Excel 2000 and analyzed using SPSS for Windows, release 20.0 (SPSS Inc. – Chicago, Illinois, USA). Parametric (Student's t-test) and nonparametric tests (chi-squared and Fisher's exact tests) and logistic regression (backward stepwise) were used for variable analysis. The p values <0.05 were considered statistically significant to reject the null hypothesis.
The study was approved by the Research Ethics Committee of the Faculdade de Medicina do ABC (protocol CEP/FMABC No. 108/205).
ResultsOf the 1,038 initial questionnaires, there were inconsistencies in ten, and 1,028 were considered valid. The female parent or guardian answered 846 (82.2%) questionnaires, whereas in 530 cases (51.5%) the responder was male, with no significant difference between the genders.
Episodes of wheezing in the first 12 months of life occurred in 499 (48.5%) infants (at least once); 253 infants (24.6%) had one or two episodes (occasional wheezing) and 246 (23.9%), three or more episodes (recurrent wheezing).
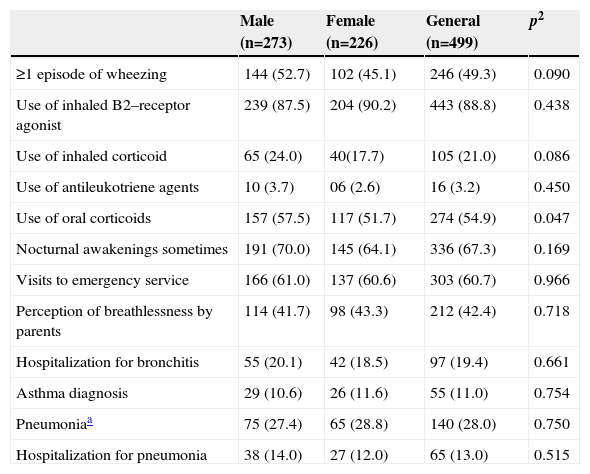
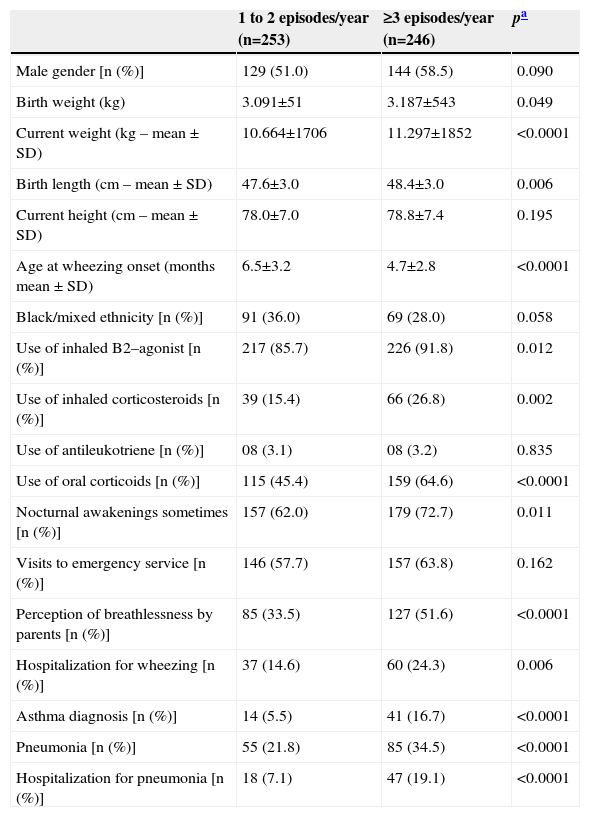
Infants that had at least one wheezing episode were divided by gender and shown in Table 1. Males showed higher values than females for weight and height at birth, as well as at 12 months of life. Table 2 presents the demographic and clinical characteristics of the groups of wheezing infants with one to two episodes (occasional wheezing) and three or more episodes (recurrent wheezing). Three or more wheezing episodes were observed in the first year of life in 499 (48.5%) infants.
Clinical characteristics of infants that had at least one wheezing episode, separated according to gender, expressed in numbers (%)
| Male (n=273) | Female (n=226) | General (n=499) | p2 | |
|---|---|---|---|---|
| ≥1 episode of wheezing | 144 (52.7) | 102 (45.1) | 246 (49.3) | 0.090 |
| Use of inhaled B2–receptor agonist | 239 (87.5) | 204 (90.2) | 443 (88.8) | 0.438 |
| Use of inhaled corticoid | 65 (24.0) | 40(17.7) | 105 (21.0) | 0.086 |
| Use of antileukotriene agents | 10 (3.7) | 06 (2.6) | 16 (3.2) | 0.450 |
| Use of oral corticoids | 157 (57.5) | 117 (51.7) | 274 (54.9) | 0.047 |
| Nocturnal awakenings sometimes | 191 (70.0) | 145 (64.1) | 336 (67.3) | 0.169 |
| Visits to emergency service | 166 (61.0) | 137 (60.6) | 303 (60.7) | 0.966 |
| Perception of breathlessness by parents | 114 (41.7) | 98 (43.3) | 212 (42.4) | 0.718 |
| Hospitalization for bronchitis | 55 (20.1) | 42 (18.5) | 97 (19.4) | 0.661 |
| Asthma diagnosis | 29 (10.6) | 26 (11.6) | 55 (11.0) | 0.754 |
| Pneumoniaa | 75 (27.4) | 65 (28.8) | 140 (28.0) | 0.750 |
| Hospitalization for pneumonia | 38 (14.0) | 27 (12.0) | 65 (13.0) | 0.515 |
Demographic and clinical characteristics of infants according to the number of wheezing episodes in the first year of life (n=499)
| 1 to 2 episodes/year (n=253) | ≥3 episodes/year (n=246) | pa | |
|---|---|---|---|
| Male gender [n (%)] | 129 (51.0) | 144 (58.5) | 0.090 |
| Birth weight (kg) | 3.091±51 | 3.187±543 | 0.049 |
| Current weight (kg – mean ± SD) | 10.664±1706 | 11.297±1852 | <0.0001 |
| Birth length (cm – mean ± SD) | 47.6±3.0 | 48.4±3.0 | 0.006 |
| Current height (cm – mean ± SD) | 78.0±7.0 | 78.8±7.4 | 0.195 |
| Age at wheezing onset (months mean ± SD) | 6.5±3.2 | 4.7±2.8 | <0.0001 |
| Black/mixed ethnicity [n (%)] | 91 (36.0) | 69 (28.0) | 0.058 |
| Use of inhaled B2–agonist [n (%)] | 217 (85.7) | 226 (91.8) | 0.012 |
| Use of inhaled corticosteroids [n (%)] | 39 (15.4) | 66 (26.8) | 0.002 |
| Use of antileukotriene [n (%)] | 08 (3.1) | 08 (3.2) | 0.835 |
| Use of oral corticoids [n (%)] | 115 (45.4) | 159 (64.6) | <0.0001 |
| Nocturnal awakenings sometimes [n (%)] | 157 (62.0) | 179 (72.7) | 0.011 |
| Visits to emergency service [n (%)] | 146 (57.7) | 157 (63.8) | 0.162 |
| Perception of breathlessness by parents [n (%)] | 85 (33.5) | 127 (51.6) | <0.0001 |
| Hospitalization for wheezing [n (%)] | 37 (14.6) | 60 (24.3) | 0.006 |
| Asthma diagnosis [n (%)] | 14 (5.5) | 41 (16.7) | <0.0001 |
| Pneumonia [n (%)] | 55 (21.8) | 85 (34.5) | <0.0001 |
| Hospitalization for pneumonia [n (%)] | 18 (7.1) | 47 (19.1) | <0.0001 |
There was a significant association between recurrent wheezing and weight during the interview, age at wheezing onset, use of oral and inhaled corticosteroids, perception of breathlessness by parents, hospitalization for wheezing, asthma diagnosis, occurrence of pneumonia, and hospitalization for pneumonia. In the multivariate analysis, however, the authors observed independent associations of recurrent wheezing only with the use of oral corticosteroids (OR=1.8, 95%CI: 1.1-2.8, p=0.009) and asthma diagnosis (OR=2.7, 95%CI 1.2-6.0, p=0 .012).
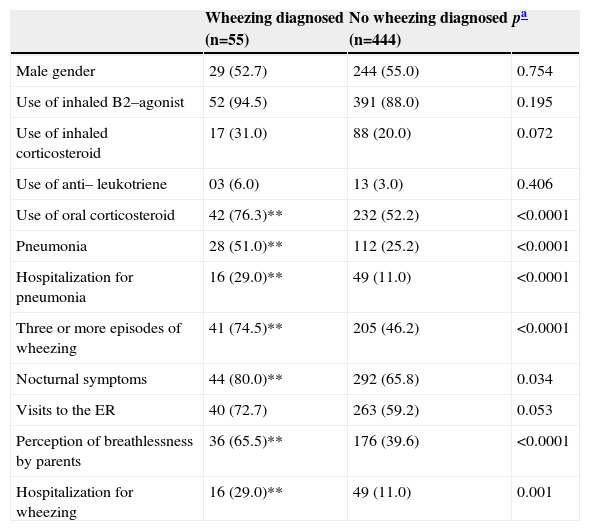
The parents of 55 (5.3%) infants reported a medical diagnosis of asthma, and the vast majority had recurrent wheezing (74.5%).
Table 3 shows the characteristics of infants with and without a medical diagnosis of asthma. In the multivariate analysis, there was an association between asthma diagnosis and use of oral corticosteroids (OR=4.1, 95%CI: 1.7-9.8, p=0.001), occurrence of pneumonia (OR=2.8, 95%CI: 1.4-5.5, p=0.002), and having family members with asthma (OR=2.1, 95%CI: 1.1-4.1, p=0.02).
Personal and clinical characteristics of infants with and without a medical diagnosis of asthma, expressed as n (%)
| Wheezing diagnosed (n=55) | No wheezing diagnosed (n=444) | pa | |
|---|---|---|---|
| Male gender | 29 (52.7) | 244 (55.0) | 0.754 |
| Use of inhaled B2–agonist | 52 (94.5) | 391 (88.0) | 0.195 |
| Use of inhaled corticosteroid | 17 (31.0) | 88 (20.0) | 0.072 |
| Use of anti– leukotriene | 03 (6.0) | 13 (3.0) | 0.406 |
| Use of oral corticosteroid | 42 (76.3)** | 232 (52.2) | <0.0001 |
| Pneumonia | 28 (51.0)** | 112 (25.2) | <0.0001 |
| Hospitalization for pneumonia | 16 (29.0)** | 49 (11.0) | <0.0001 |
| Three or more episodes of wheezing | 41 (74.5)** | 205 (46.2) | <0.0001 |
| Nocturnal symptoms | 44 (80.0)** | 292 (65.8) | 0.034 |
| Visits to the ER | 40 (72.7) | 263 (59.2) | 0.053 |
| Perception of breathlessness by parents | 36 (65.5)** | 176 (39.6) | <0.0001 |
| Hospitalization for wheezing | 16 (29.0)** | 49 (11.0) | 0.001 |
To date, there has been no previous study on the prevalence of wheezing in the first year of life in infants residing in the municipality of Santo André. In Brazil, the EISL questionnaire has been administered to children aged 12 to 15 months in the cities of Belém, Belo Horizonte, Curitiba, Fortaleza, Porto Alegre, Recife, and São Paulo.13,16 Some authors, however, noting the difficulty in diagnosing asthma in children aged up to 3 years, as well as aiming to differentiate wheezing caused by other disorders in this age group, performed the validation of the WQ-EISL in children aged 12 to 36 months. The objectives of this validation were also to verify whether the results obtained in a more restricted age range persisted in older children, in addition to recording its reproducibility and internal consistency.17. Therefore, during the course of this research, it was considered appropriate to extend the age range of questionnaire application from 12-15 months to 12-24 months.
In the city of Curitiba, state of Paraná, Brazil, the prevalence of at least one wheezing episode in the first year of life was 45.4%, and in São Paulo, 46.0%,13,18 much lower results than those found in Porto Alegre (63.3%),14 possibly due to climatic conditions. In Santo André, this study demonstrated that 48.5% of the infants had wheezing in the first year of life, similar to what was observed in São Paulo and Curitiba, which are areas with high prevalence of wheezing and asthma in children and adolescents.15,19 A cross-sectional study conducted in São Paulo found a prevalence of recent wheezing (one or more episodes in the past 12 months) of 11% in children aged 6-11 months and of 14.3% between 12-23 months.20
Several studies have shown a higher frequency of recurrent wheezing in developing countries when compared to developed countries.6,21,22 In São Paulo, in a cohort of infants from low-income families, it was shown that, after 30 months of follow up, 52% had recurrent wheezing.8 Muiño et al. followed a cohort of newborns up to 12 years of age in the city of Pelotas, state of Rio Grande do Sul, Brazil, and observed prevalence of transient wheezing (wheezing up to 4 years and absence of wheezing at 10-12 years) 43.9%; persistent wheezing (wheezing during the entire follow-up) of 6.4%, and late-onset wheezing (wheezing at 10-12 years) of 3.3%.23 The present study observed that 23.9% of the infants had recurrent wheezing, with three or more wheezing episodes in the first years of life, similar to the data observed in Curitiba (23%) and lower than in São Paulo (27%) and Recife (26%) using the WQ-EISL.12,18,24
Male gender is known risk factor for wheezing in infancy due to the smaller airway diameter.4 In the present study, among the wheezing infants, a trend for a higher number of males compared to females was observed (273/226), but a significant difference was only observed regarding the use of oral corticosteroids, which may be due to the greater severity of episodes in males. There was no difference between genders regarding the prevalence of recurrent wheezing, use of other medications, and nocturnal awakening symptoms, as well as asthma diagnosis.
Recurrent wheezers started having episodes at an earlier age than occasional wheezers and had higher weight at the time of the survey, a factor reported by some authors as associated with recurrent wheezing and asthma in childhood.20 In a prospective study by Martinez et al., most children who had wheezing episodes started having them in the first year of life. Of these, 50% persisted with symptoms up to six years of age, considered asthmatics.4
In the present study, according to information provided by the parents, 54.9% of the wheezing infants had used oral corticosteroids for the treatment of a wheezing episode, with this use being associated with greater frequency and severity of episodes. The use of corticosteroids was higher in the recurrent wheezing group, when compared to the occasional wheezing group, both by oral (64.6% versus 45.4%) and inhaled administration (26.8% versus 15.4%). As expected, infants with recurrent wheezing who have a higher risk of developing asthma25,26 showed association with variables that indicate greater severity of episodes, such as asthma diagnosis, pneumonia, and hospitalization for pneumonia.
Wheezing was identified as a risk factor for pneumonia in a study conducted in São Paulo.18 Hospitalization for pneumonia, in addition to increasing healthcare system costs, results in social and psychological costs, nutritional impairment, and risk of opportunistic nosocomial infections.27 According to the Brazilian Ministry of Health, in 2006, 34.5% of hospital admissions of individuals younger than 1 year of age throughout Brazil were caused by respiratory diseases. In São Paulo, this rate was 34.9% and in Santo André, 40%.28
The infants who received a diagnosis of asthma had three or more episodes of wheezing, nocturnal symptoms and more frequent perception of breathlessness by parents, greater use of oral corticosteroids, association with pneumonia, and hospitalization for pneumonia. Similar results were observed in São Paulo, Maceio, and Curitiba.12,18,24
The present study showed significant associations between asthma diagnosis and a greater number of crises, perception of breathlessness by the parents, and oral corticosteroid use. After excluding wheezing caused by viral agents, asthma is the most common cause of wheezing in childhood.29 However, it was observed that only 5.5% of children received this diagnosis. Attaining a correct diagnosis of asthma in childhood from the first year of life is important for infants with recurrent wheezing.12 Pediatricians, when treating a child with recurrent wheezing, often hesitate to use the term “asthma”, tending to emphasize the diagnosis of infections. The term “bronchitis” is closer to this concept and is usually more easily accepted by parents, as it does not mean, from their point of view, the stigma of a chronic and incurable disease. The under-diagnosis and undertreatment of asthma are responsible for many pediatric hospitalizations.
The delay in the diagnosis of asthma in children results in the worsening of symptoms and increased treatment costs.30
Research on wheezing and asthma in childhood are required to assist with the implementation of public health policies aimed at decreasing socioeconomic and educational inequalities among the population and, hence, reduce the prevalence and severity of wheezing in the first year of life, especially in developing countries.31 The implementation of campaigns against passive smoking should be encouraged, considering that exposure to cigarette smoke in the pre- and/or postnatal period is one of the major risk factors for wheezing in infants.32 The study of a cohort of children in Germany33 showed that having one smoker parent, associated with family history of asthma, increased the risk of wheezing by threefold when compared to family history of asthma alone.
It is concluded that in the city of Santo André, half of the infants assessed had at least one episode of wheezing in the first year of life. Half of these infants are recurrent wheezers, and this recurrent condition is associated with high morbidity. However, few infants received a diagnosis of asthma.
Conflicts of interestThe authors declare no conflicts of interest.
FundingFaculdade de Medicina do ABC.