Cementoblastoma is a benign odontogenic tumor, classified as a rare lesion, of slow growth, with expansion of the cortical bone; it is associated with the root of a tooth with pulp vitality, appearing more commonly in the posterior region of the mandible. In this paper, a rare case report of a surgically treated benign cementoblastoma affecting the maxilla of an 11-year- old patient is presented. Furthermore, the diagnostic methods, the clinical, imaging and histopathological features, and the treatment options are discussed. Finally, correlations are made with findings in the scientific literature.
O cementoblastoma é uma neoplasia odontogênica benigna, classificada como uma lesão rara, de crescimento lento, com expansão da cortical óssea, associada à raiz de um dente com vitalidade pulpar, apresentando-se mais comumente em região posterior de mandíbula. O presente artigo tem o objetivo de relatar um caso clínico raro de cementoblas- toma benigno localizado no maxilar superior de uma paciente de 11 anos de idade, tratado através de enucleac¸ão cirúrgica, bem como discutir o método diagnóstico, aspectos clínicos, radiológicos e histopatológicos e formas de tratamento desta lesão, correlacionando com dados da literatura especializada.
Cementoblastoma is defined as a tumor of the odontogenic ectomesenchyme, according to the Classification of the World Health Organization (WHO) of 2005.1,2 It is also called a true cementoma, where it is a rare, slow-growing, benign neoplasm, which originates from cementoblasts and is associated with the root of a permanent tooth with vitality.1–3
The most common clinical characteristic of this tumor is bulging, showing expansion of the cortical bone, which produces facial asymmetry1–6 and anteroposterior dental crowding.7 The main radiological feature of this lesion is a radiopaque or mixed-density image, well defined by a radiolucid halo fused to the root of the tooth.1–4,7–10 It manifests preferentially in molar and premolar regions in the mandible,2–4,7,9,10 but affects the maxilla as well5 and in some cases the region of the incisors.8,11 There is no gender predilection,1–3 and the tumor is more predominant in the second and third decades of life.1,2,4,6,8,10
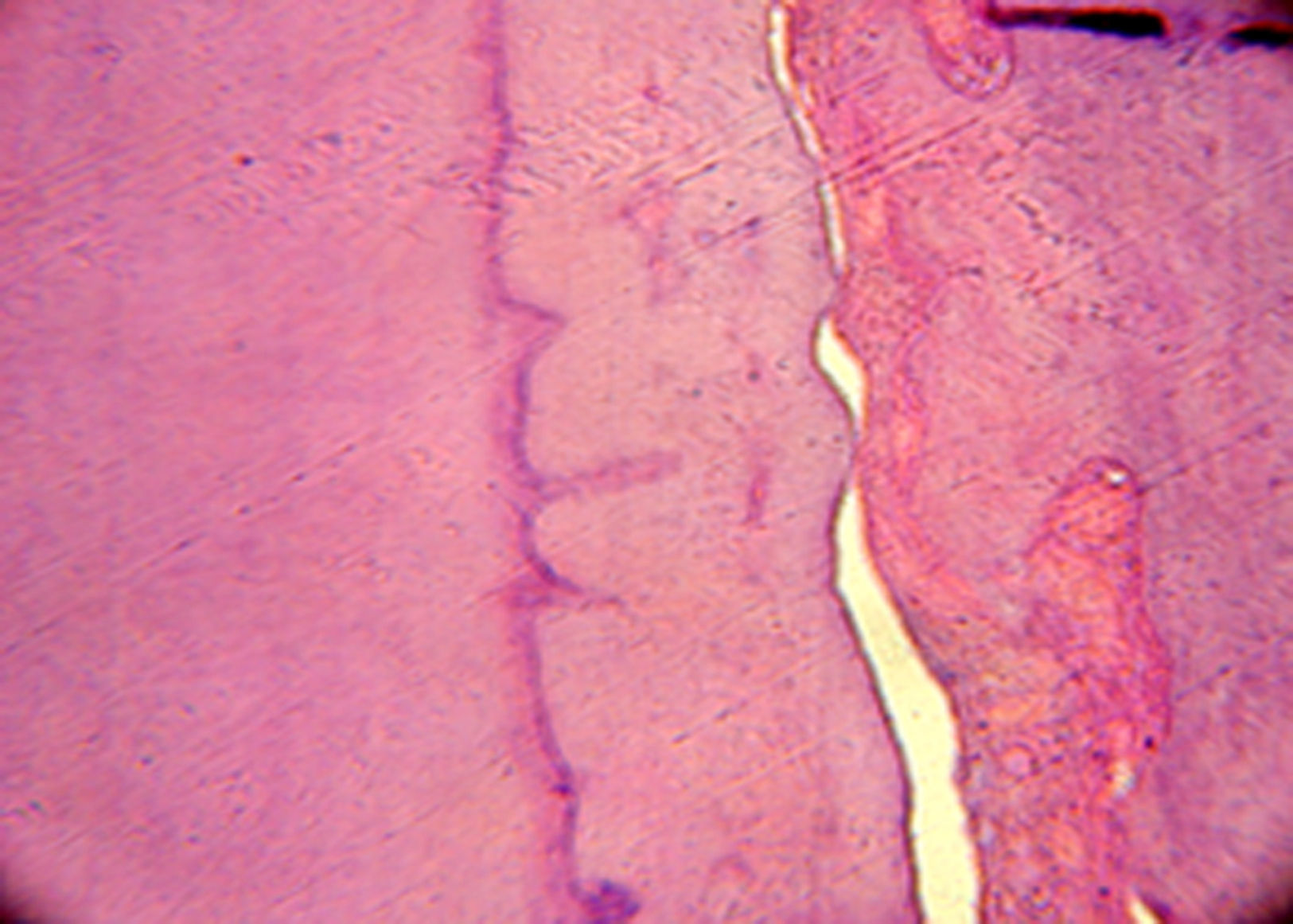
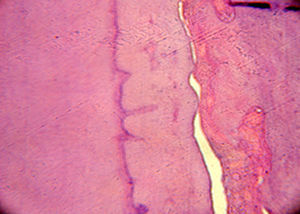
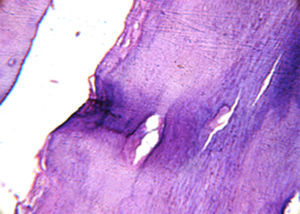
Histopathologically, it appears as a mass that resembles mineralized cement and fibrovascularized stroma, interposed by cementoblasts.2,3,5,6,8,9,12 Some radiopaque lesions share similar characteristics, and the differential diagnosis of benign cementoblastoma includes lesions such as osteoblastoma,1–3 odontoma, focal sclerosing osteomyelitis and hypercementosis,3 as well as cemento-osseous dysplasia and periapical sclerosing osteitis.4 The only distinctive criterion is the true connection with the surface of the root of a tooth in the case of cementoblastoma.1
The treatment proposed for the lesion is complete enucleation of the tooth-lesion mass, due to its intimate relation with the tooth root, and curettage.2,3,6–10 Recurrences are generally associated with mistakes in the form of treatment, which have not been described in cases of benign cementoblastoma.1,3,6,8
The aim of this paper was to report a case of benign cementoblastoma in the maxilla, as well as to discuss its clinical, histopathological and imaging features with findings in the current scientific literature.
Case reportThe patient, a dark-skinned 11-year-old girl, was seen at the outpatient clinic of the Surgery Department of Universidade Estadual de Feira de Santana (UEFS), complaining of delayed tooth eruption and facial swelling on the left side. On extraoral physical examination, a discrete facial asymmetry was observed, with increased volume in the region of the nasolabial sulcus and small elevation of the nasal wing on the left side. On intraoral physical examination, the absence of some teeth was seen. According to the chronology of eruption, maxillary lateral incisors should have already been present. A loss of depth of the vestibular sulcus in the region of the left maxillary lateral incisor was also seen (Fig. 1). During palpation, a swelling of hard consistency was noted.
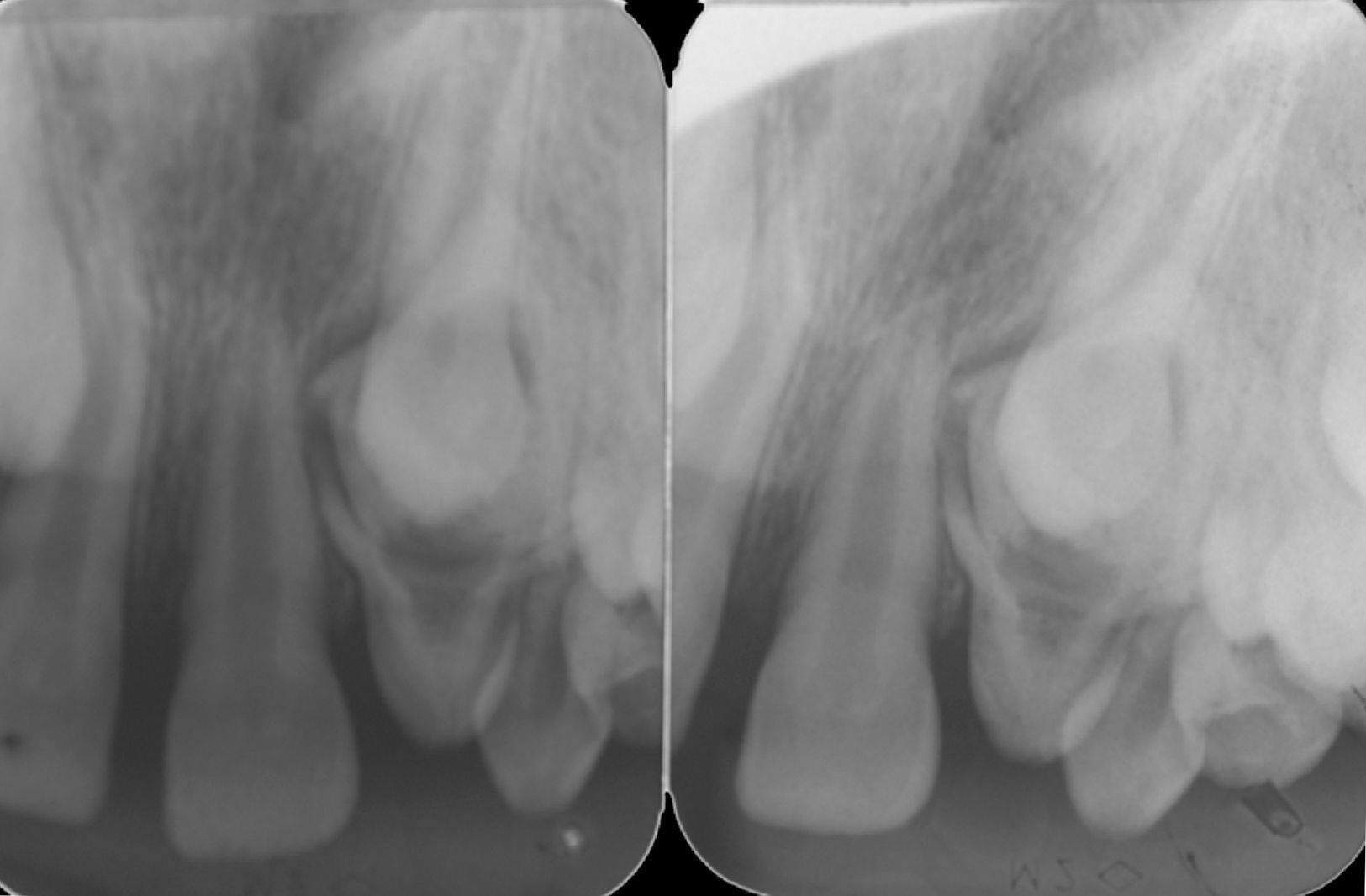
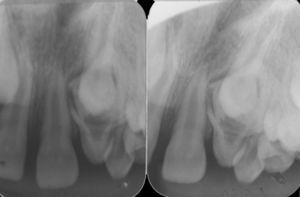
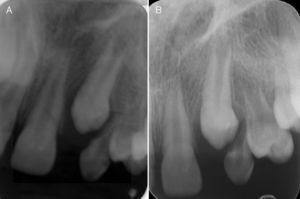
Radiographic examinations were performed, which included periapical and occlusal radiographs, localization by Clark's method, and panoramic radiographs, where the following aspects were observed: agenesis of right maxillary lateral incisor, and a radiopaque lesion with radiolucid halo associated with the root of a tooth that was supposedly, by localization, the left maxillary lateral incisor. This tooth had an enlarged pulp chamber. The presence of a superposed left maxillary canine was evident. The right maxillary lateral incisor was missing, and displacement of the lesion was not noted in the Clark radiographic localization technique (Figs. 2 and 3).
In accordance with the clinical and imaging characteristics observed, the diagnosis proposed was compound odontoma or hypercementosis, because of the interference of the lesion with the eruption of the permanent canine and the lateral incisor affected by the lesion. In agreement with the mother and after signed informed consent, it was decided to access the lesion surgically to visualize the radiopaque lesion and to make an intraoperative diagnosis, as well as to obtain a biopsy for histopathological analysis. Routine preoperative examinations were conducted, confirming the patient's picture of overall health, making it possible for her to undergo the surgical procedure.
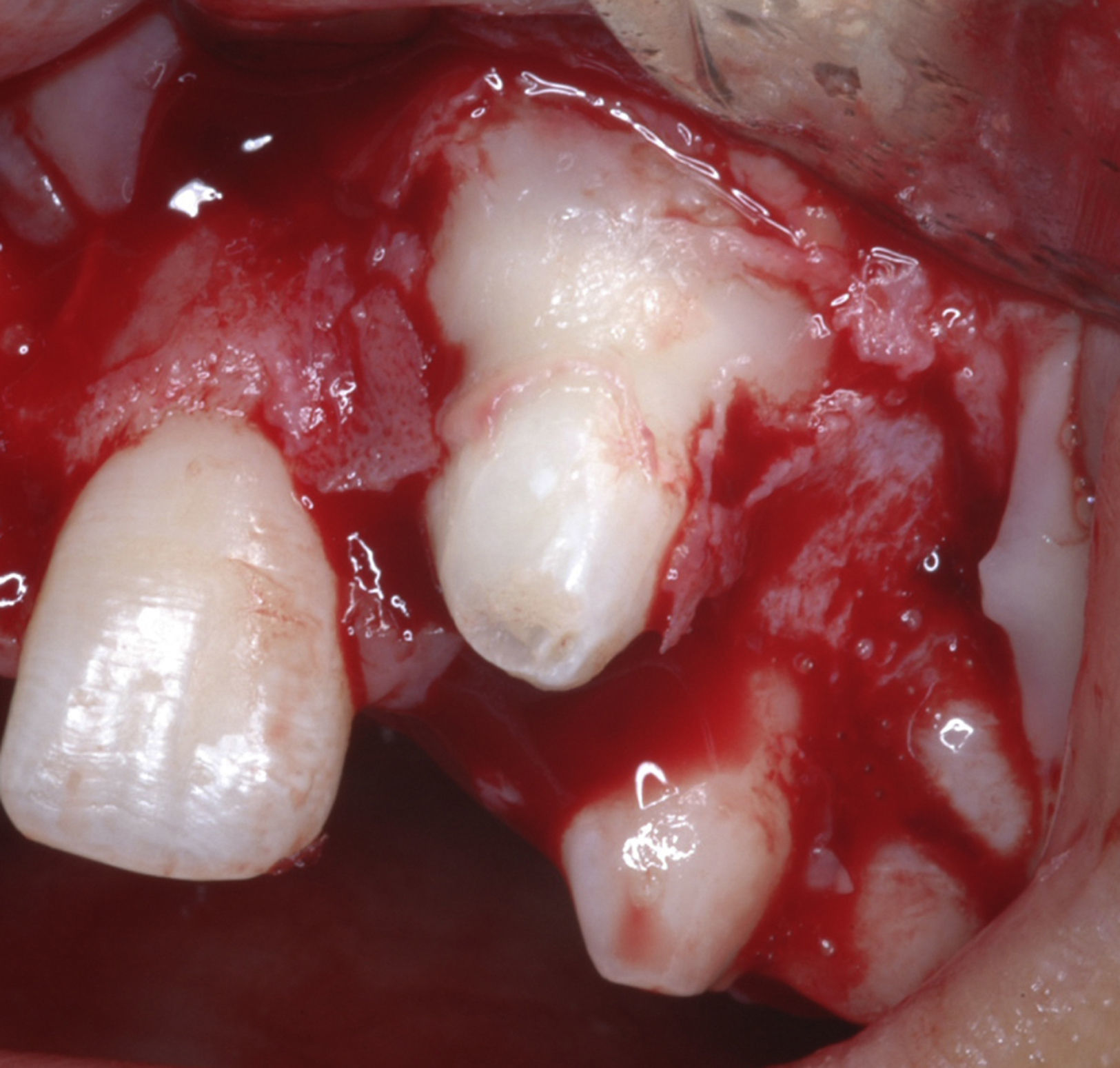
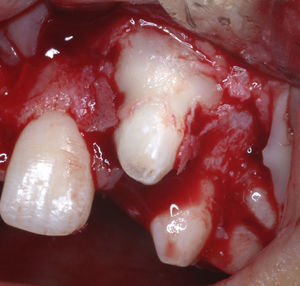
The patient was premedicated with the anxiolytic midazolam 7.5mg and dexamethasone 4mg, the protocol used to control postoperative inflammation. The anesthetic technique utilized was bilateral anterior superior alveolar and nasopalatine regional nerve block with infiltrative terminal block. Puncture aspiration was carried out before incision, which was negative for the presence of fluid, confirming the solid nature of the lesion. A vestibular incision was made in an L-shape, with a releasing incision in the distal portion of the right maxillary central incisor. Mucoperiosteal detachment and initiation of osteotomy were performed with a low-speed motor and abundant irrigation on top of the lesion (Fig. 4).
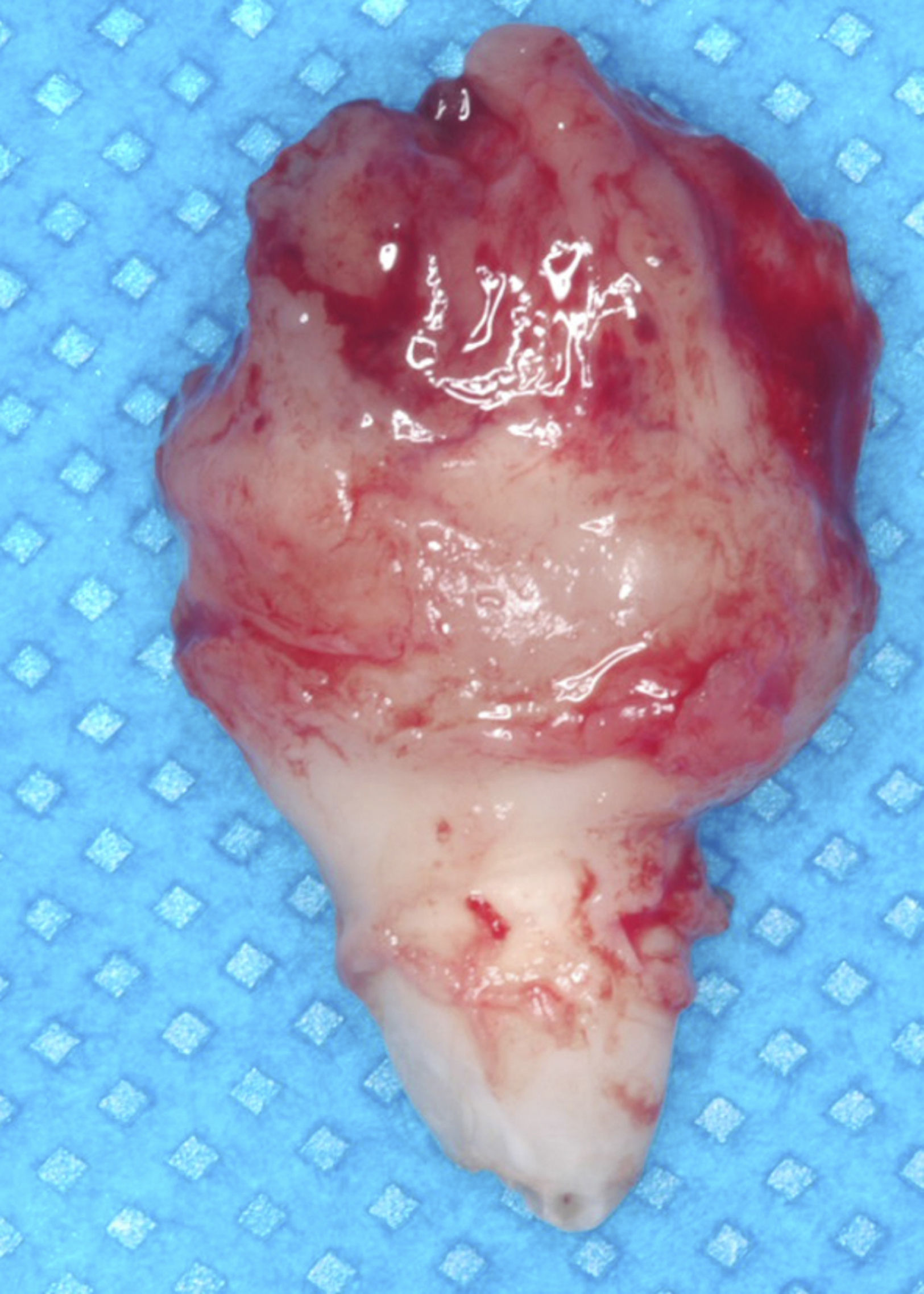
During osteotomy, the lesion was found to be adhered to a tooth supposedly the left maxillary lateral incisor, therefore enucleation of the tooth-lesion mass and curettage of the alveolar bone were performed. The surgical cavity was irrigated and cleaned and then closed with simple sutures. The postoperative medications prescribed were a nonsteroidal antiinflammatory (nimesulide) and peripheral analgesic (sodium dipyrone). The surgical specimen measured 2×1cm (Fig. 5) and was sent for histopathological examination, with the slides being submitted to hematoxylin–eosin (HE) staining; the definitive diagnosis was benign cementoblastoma (Figs. 6 and 7).
One week after surgery, the patient returned for removal of sutures, which was done without problems. The test for pulpar vitality in the central incisor was not necessary because the surgical intervention was far from the apex of this tooth. After 6 months of postoperative monitoring satisfactory wound healing was noted, as well as tooth eruption following the chronological order (Figs. 8 and 9). Currently, the patient is under follow-up by the Surgery Department without signs of recurrence.
Discussion and conclusionsCementoblastoma is classified by the WHO Classification of 2005 as a tumor of ectomesenchyme origin, with or without inclusion of epithelium.1,2
Although authors affirm that there is no gender predilection,1–3 there are numerous reports of this tumor in males in the second and third decades of life,4,5 along with reports of occurrence in females in the same age range.7 However, there are only 17 reported cases of benign cementoblastoma affecting the maxilla of young female patients, this being the 18th.13 Of these, only 3 previous cases were reported in the anterior region of the maxilla, with 2 being associated with canines14,15 and 1 a central incisor,11 and thus, this is the first case involving a lateral incisor.
Clinically, benign cementoblastoma is characterized by slow growth,3 presence of a bulge2–6,8 and usually a symptomatic nature,2,3,8,10 although some cases do not reveal painful symptoms.5,7 These features result in a certain facial asymmetry2–6,8 and dental crowding.7 These characteristics were found in the case presented here, but in a milder form because of the age of the patient, at which there was mixed dentition and agenesis of some teeth, and thus, these features are in accordance with those described in the literature.
Usually, the patient seeks dental treatment after noting facial and dental alterations. There are some difficulties with the suspected diagnosis, because some teeth may be partially or totally impacted, which can be the case during a routine dental examination, and thus, it is confirmed by histopathologic examination.3,5,6,8,9,12 These aspects were observed in the patient presented here.
Due to progressive facial deformity, sequelae and painful occurrence at the tumor site, the patient should be informed of the necessity of surgical resection. This is done by simple enucleation through intraoral access and curettage.2,3,6–10 Recurrence is rare and the prognosis is excellent,2,3,6,8 which was corroborated by the fact that the patient did not show signs of recurrence to date.
Cementoblastoma is observed in conventional radiographs, which show a radiopaque or mixed-density image, well-defined by a radiolucid peripheral zone associated with the root of a tooth.1–4,7–10 These findings were evident in the patient presented, but are not specific for the disease.
As it is a rare lesion, the diagnosis of benign cementoblastoma introduces many uncertainties, since it displays similar characteristics as other lesions, and thus, it is necessary to look for more relevant aspects as alternatives for diagnosis. Complex odontoma, for example, differs from cementoblastoma by showing a radiopaque image of dentin-enamel, despite the two lesions being associated with the root of a vital tooth.2–4 Periapical sclerosing osteomyelitis is limited to the periapex of a non-vital tooth and does not involve a tumor, and thus, it does not show continuous growth.2,3 The same occurs with hypercementosis; it has similar clinical signs and imaging features as cementoblastoma, but it is also not a tumor.2 Osteoblastoma is a neoplasm with aspects intimately related to cementoblastoma, except that the lesion is not involved with a tooth.2 Cemento-osseous dysplasias can be exteriorized, show signs of infection (pus, edema, sequestrae) and can show a mixed image, depending on the phase in which it is detected.2,3
The treatment of cementoblastoma by surgical excision and enucleation of the tooth-lesion mass is in accordance with the literature.3,6,8 Such treatment has a good outcome since there are no reported cases of recurrence.
The present case is the first report of a cementoblastoma affecting a maxillary lateral incisor. This is a rare case as it involved a semi-impacted tooth, localization in the maxilla and occurrence at 11 years of age. This is a younger age than that reported in the international literature for this type of lesion affecting the maxilla of a female patient. The proposed treatment of surgical enucleation of the lesion together with the involved tooth appeared adequate and in agreement with the literature. The patient shows no signs of recurrence after two years of follow-up.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.