Focal osteoporotic bone marrow defects are rare conditions of the jaws, appearing normally as asymptomatic radiolucent lesions in posterior mandible of middle-aged women. A 52-year-old woman presented an extensive and symptomatic well defined hyperdense lesion in maxilla that was protruding into the right maxillary sinus. The lesion was totally excised and the association of histopathological and clinical features led to the diagnosis of focal osteoporotic bone marrow defect associated to osseous repair. The present case has some particularities as an unusual site, image exam's appearance and the presence of swelling and pain, which are not commonly reported in literature.
Defeitos osteoporóticos focais da medula óssea são condições raras nos maxilares, aparecem normalmente como lesões radiolúcidas assintomáticas em região posterior de mandíbula em mulheres de meia-idade. Uma mulher de 52 anos de idade apresentou uma extensa lesão hiperdensa bem definida e sintomática em maxila, a qual se estendia para dentro do seio maxilar direito. A lesão foi excisada completamente e a associação dos aspectos clínicos e histológicos levou ao diagnóstico de defeito osteoporótico focal da medula óssea associada a áreas de reparo ósseo. O presente caso possui algumas particularidades como sítio incomum, aparência nos exames de imagem, bem como presença de aumento de volume e dor, os quais não são comumente reportados na literatura.
Foci of hematopoietic marrow that persist into adulthood in certain areas of the jaws, is usually restricted to the condylar process, angle of the mandible, and the maxillary tuberosity.1,2 The focal osteoporotic bone marrow defect (FOBMD) is a rare condition of the jaws, and has been reported since 1954, by Cahn, who described variations of the normal location of bone marrow within the jaws present as focal defects.2
The etiology of the FOBMD is still unknown and it is reported that it may be caused by situations such as: (a) persistence of fetal marrow; (b) altered repair of bone trabeculae in area of trauma or inflammation; (c) an increased systemic need for blood cells that stimulates the development of hematopoietic bone marrow foci or (d) an ischemic change of the bone marrow tissue.3,4
The radiographic appearance of these defects is not sufficiently characteristic to permit an exact diagnosis. However, a radiolucent lesion with either distinct or poorly defined irregular borders, located in the posterior mandible of a middle-aged woman should suggest an FOPMD.1 It's asymptomatic fortuitously discovered and may be associated with local pain and swelling. A definite diagnosis requires microscopic examination of the tissue. Microscospic findings including cellular hematopoietic bone marrow, fat cells and trabeculae bone and no treatment is necessary.1–5
In this article, we report a case of FOBMD in a 52-year-old Brazilian woman who presented an extensive and symptomatic well defined hyperdense lesion located in right maxilla.
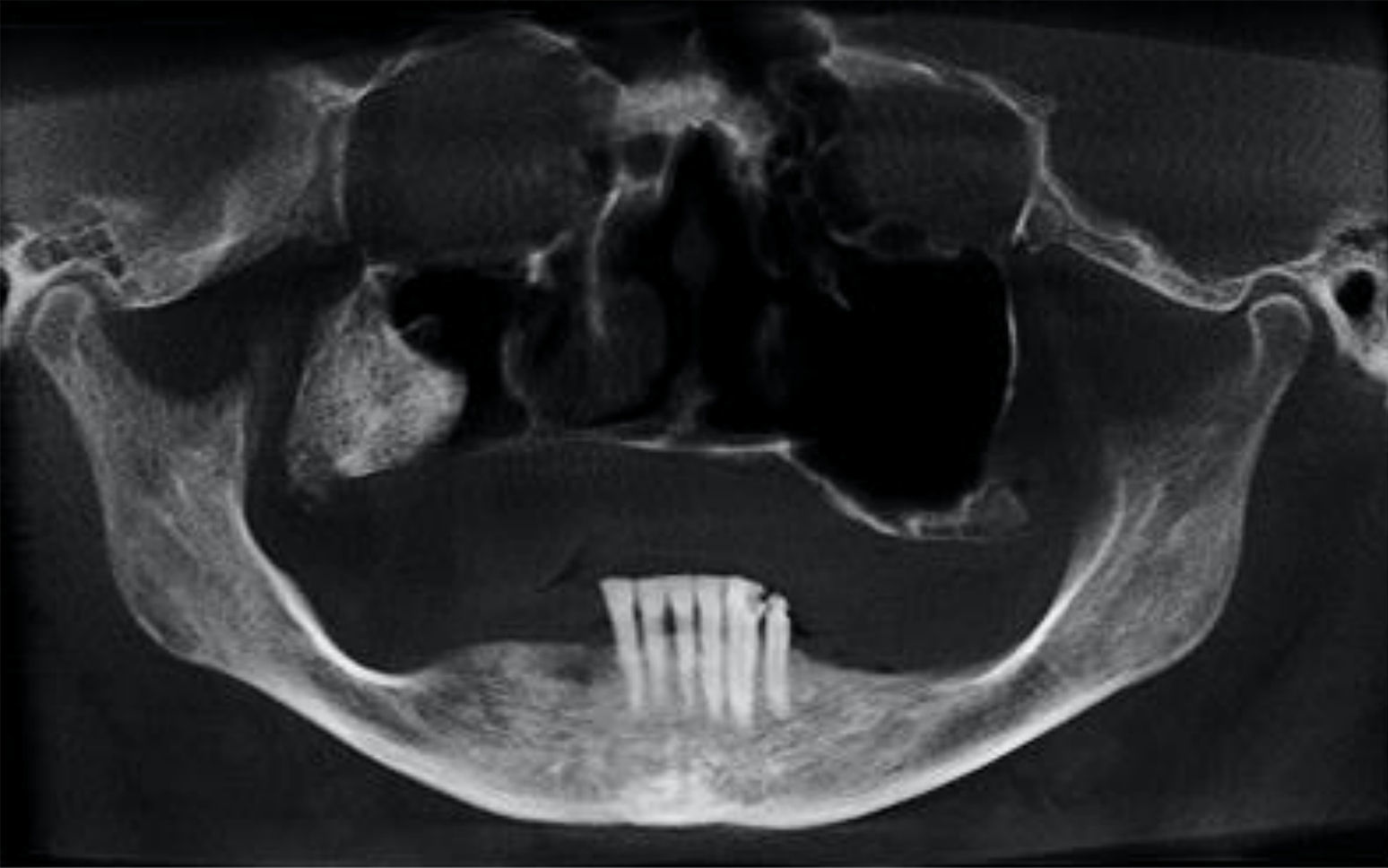
Case reportA 52-year-old female patient was referred to a Buco-Maxilo-Facial Center, complaining of a difficult in maxillary prosthesis's adaptation due to a painful one-year-swelling of the maxilla. Intraoral examination revealed a swelling on right alveolar ridge, with hardened consistency (Figure 1). No systemic disorders were recorded on her medical history. Cone beam computed tomography showed a 2.5cm×2.3cm extensive well defined hyperdense lesion, with hypodense areas, similar to bone tissue in pre-molar and molar edentulous right region, growing into maxillary sinus (Figure 2). The main part of the lesion was protruding into the right maxillary sinus (Figure 3).
Under local anesthesia, an incisional biopsy was performed in the posterior alveloar ridge of the first quadrant of the maxilla. Four fragments of tissue were removed and fixed in 10% formalin for examination. On The specimens had a brownish coloration with a hardened calcified aspect. The smallest fragment measured 0.1cm×0.1cm×0.2cm and the biggest fragment measured 0.2cm×0.2cm×0.4cm. Microscopic examination revealed tissue fragments with the presence of a trabecular bone arranged on plates and fibrovascular connective tissue between them. Even though the fragments removed were not representative, the preliminary diagnosis was suggestive of osteoma or fibro-osseous dysplasia. However, the final diagnosis could only determined with an excisional biopsy.
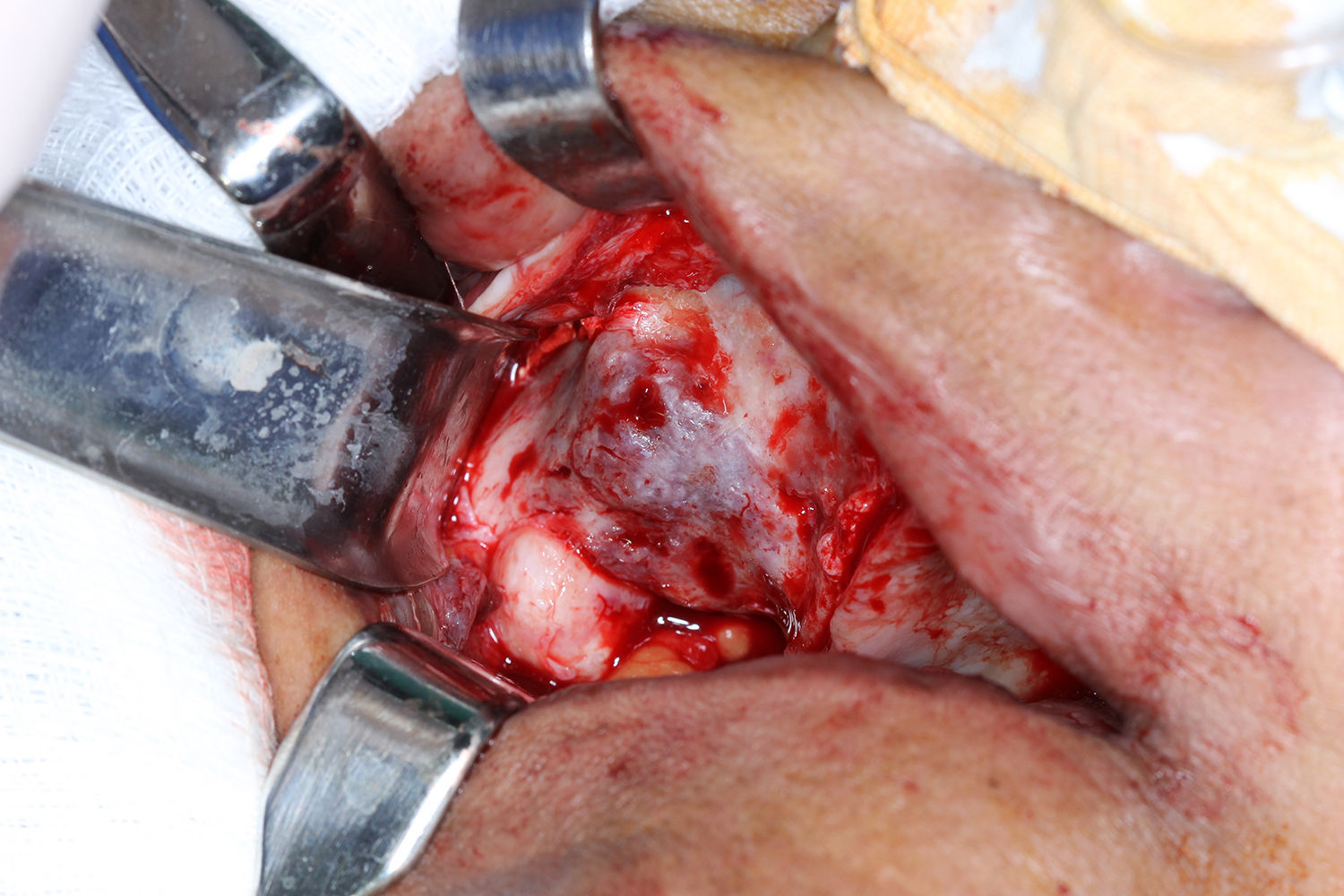
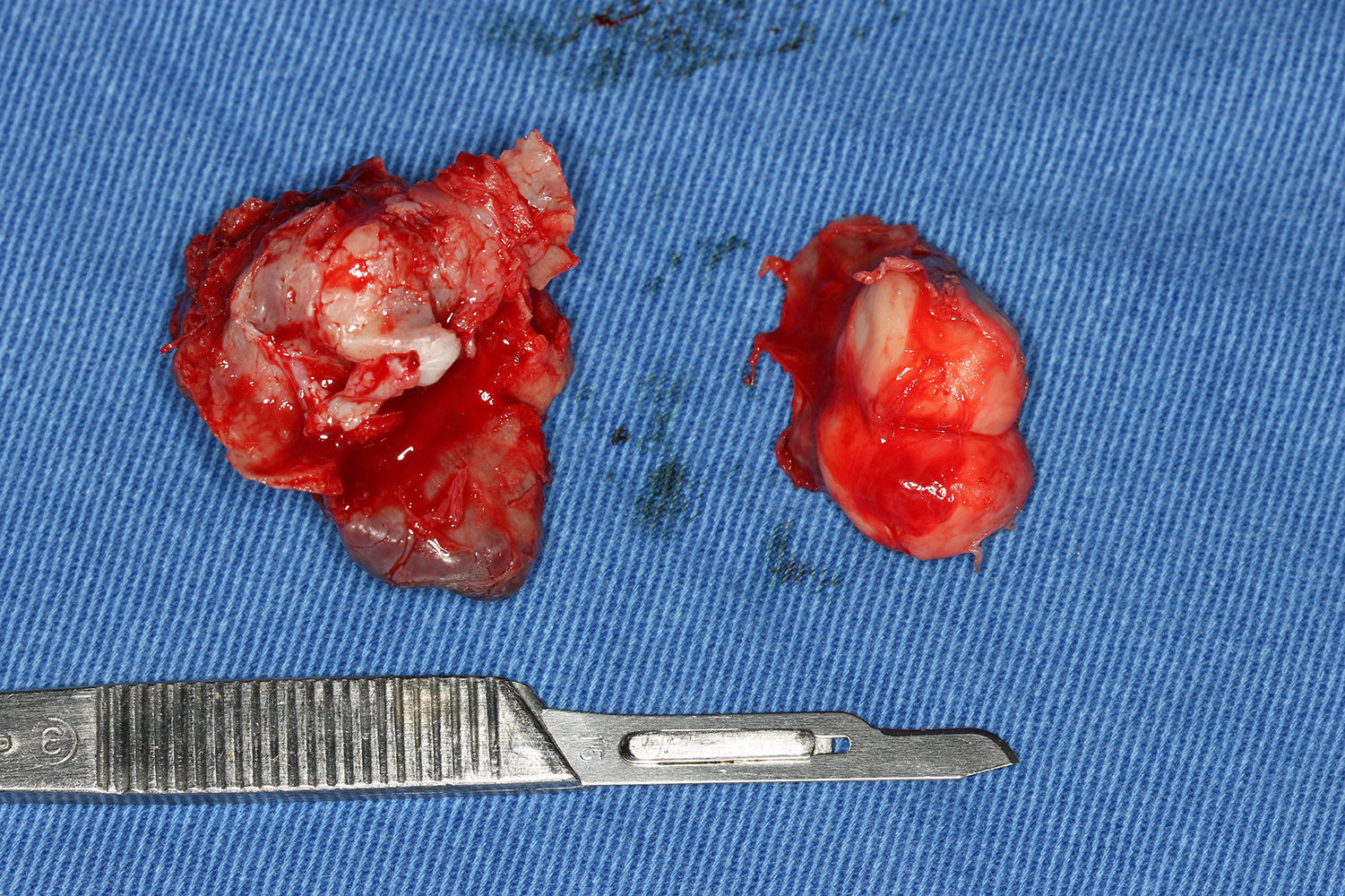
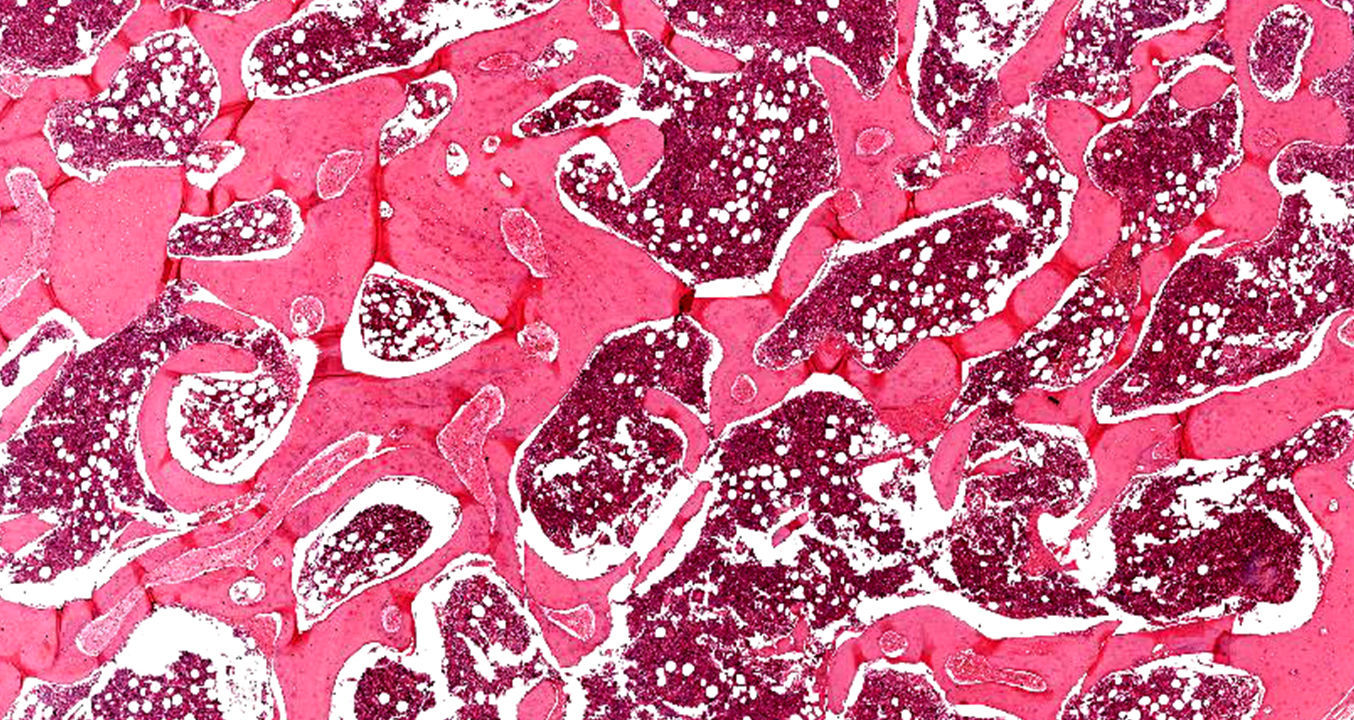
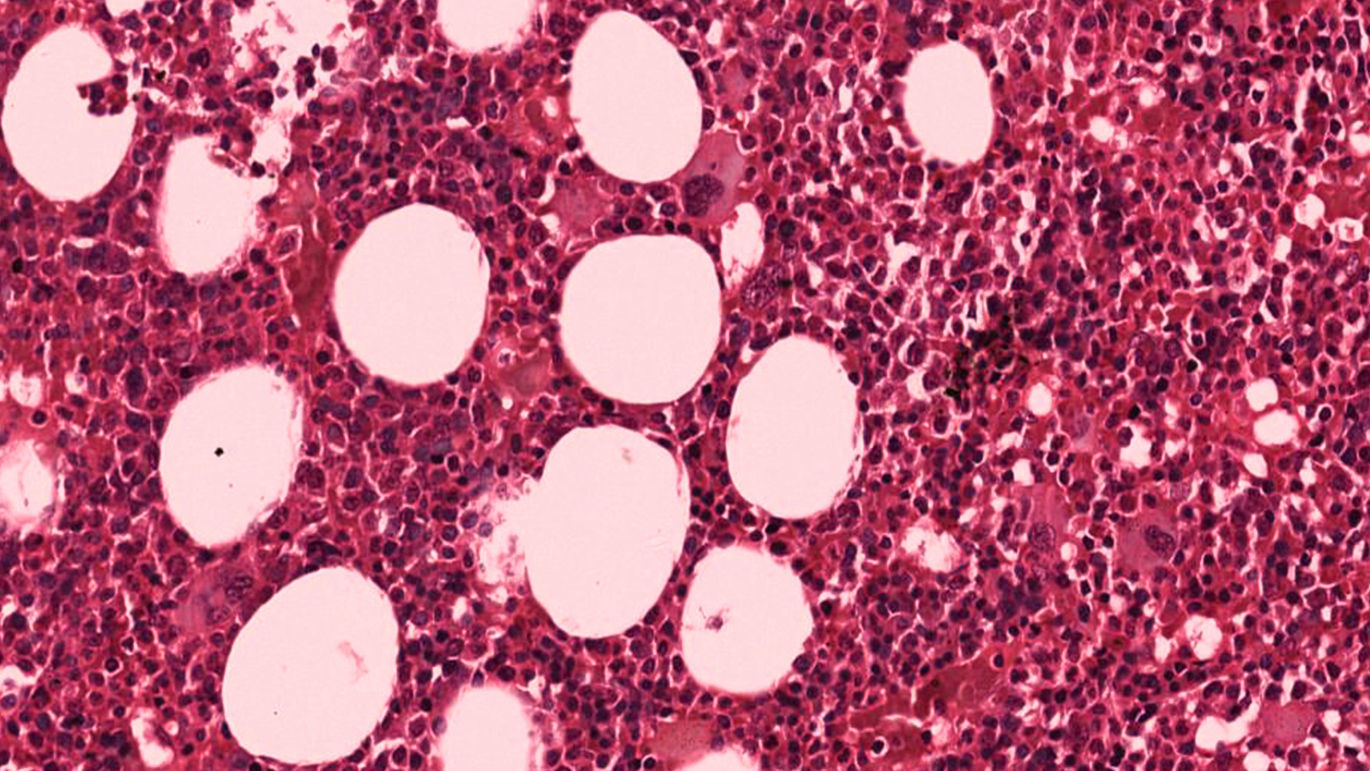
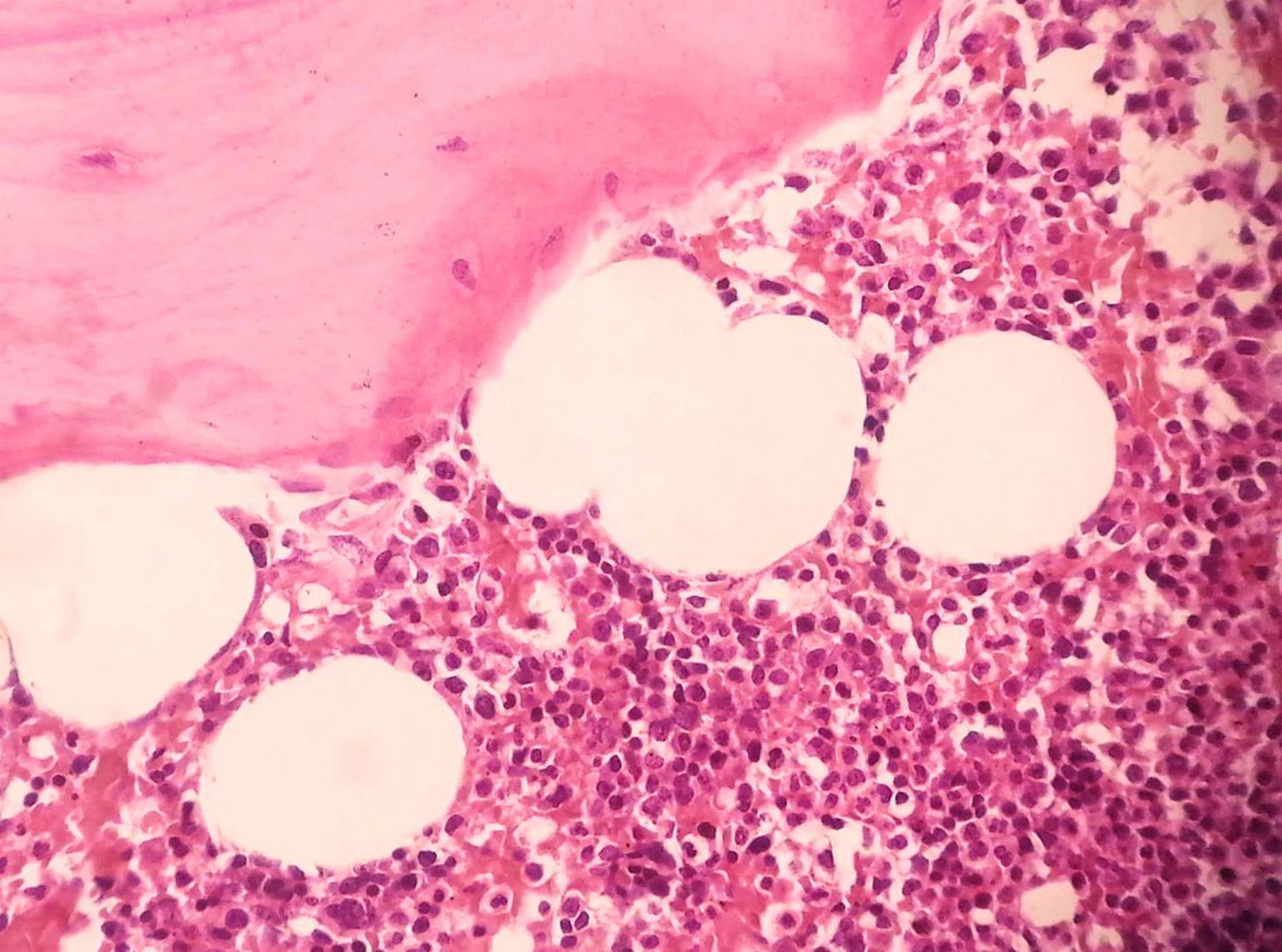
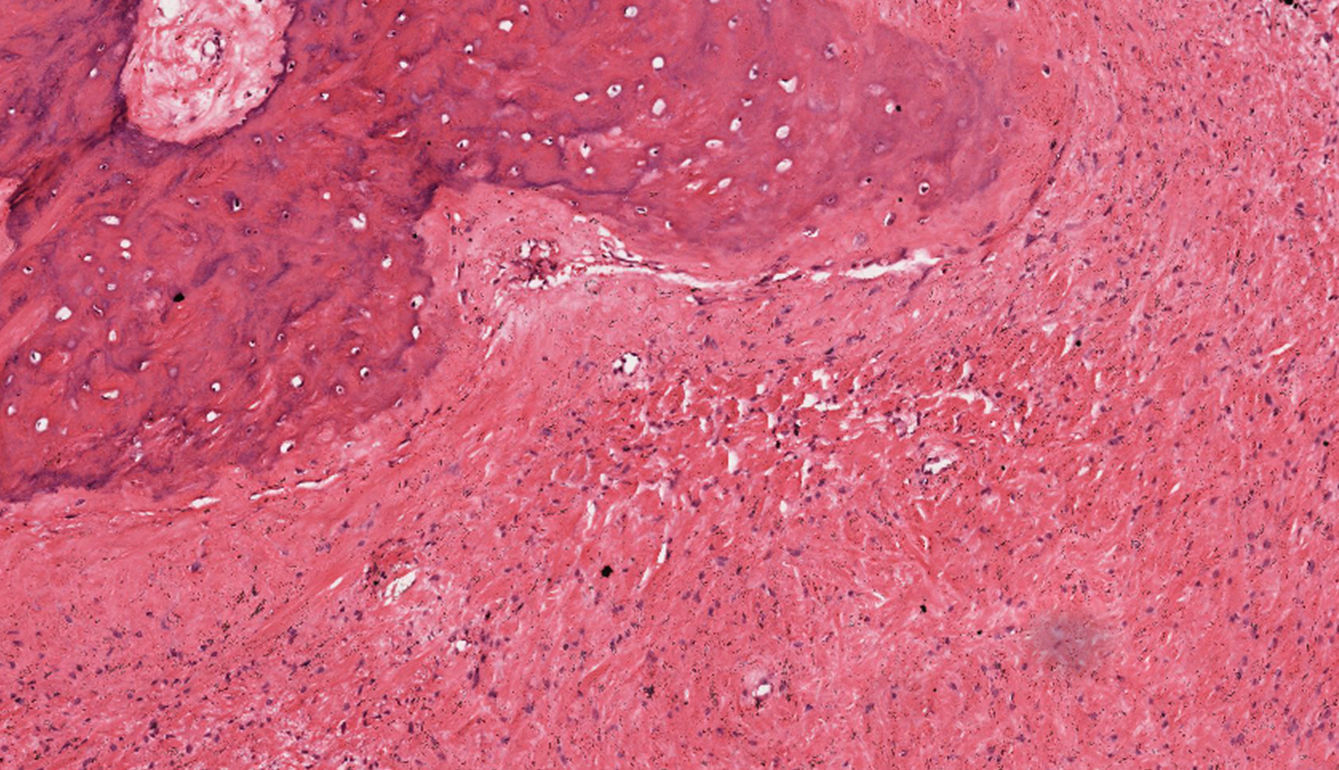
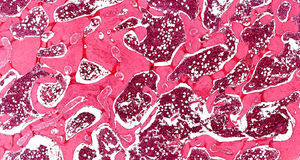
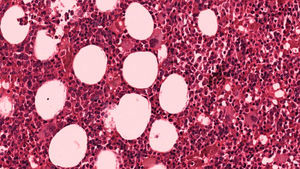
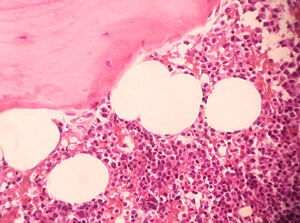
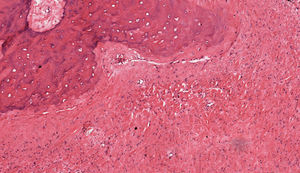
Under general anesthesia with endotracheal intubation, the lesion was then completely removed with a peripheral osteotomy and sent for histological evaluation. Surgical site after the procedure and gross specimen are observed in Figures 4 and 5. Microscopic examination revealed hematopoietic bone marrow composed of erythroid, granulocytic, monocytic and lymphocytic series, as well as megakaryocytes associated with fatty marrow and bone trabeculae, without signs of malignancy (Figures 6–8). In other areas, immature trabecular bone with basophilic lines was detected and some of the trabecular bone presented loss of osteocytes in its lacunae and surrounded by an exuberant fibrous tissue was also observed (Figure 9). The diagnostic of focal osteoporotic bone marrow defect associated to osseous repair was established. A 7-month follow-up revealed no recurrence and the surgery site healed without complication.
FOBMD of the jaws are asymptomatic radiolucent lesions, that occur predominantly in mandibular molar regions of middle-aged women, between 30 and 50 years old, and the cases are diagnosed fortuitously. The etiology of FOBMD is unknown, but it frequently occurs in an edentulous region where tooth extraction was previously performed, as an altered repair of bone trabeculae in an area of previous trauma or local inflammation.1,3 Other possibilities include persistence of fetal marrow, bone resorption secondary to marrow hyperplasia in response to an increased demand for blood cells, or an ischemic change of the bone marrow tissue.3 Some systemic conditions, such hematologic disorders as anemia and sickled anemia are associated to FOBMD.1 In the present case, the history of tooth extraction was not recent and we could speculate that the FOBMD is of long duration due to the presence of exuberant fibrous tissue associated with the bone marrow defect. Also, the patient blood analysis was normal excluding a possible association with anemia.
In the present case, the uncommon location and the clinical peculiar presentation was a challenge for the diagnostic. Previous reports showed that FOBMD is most commonly found in the posterior mandible1–4,6,7 and only 5–35% of the cases are diagnosed in maxilla, representing the minority of the reported cases.1,3,8 Most of the cases are asymptomatic and have no swelling,4 found incidentally on routine radiographs, however in rare situations, this condition may be accompanied by pain or swelling.6 Otherwise, some authors indicates the presence of pain and swelling in approximately 62–65% of the patients.3,9 In other reported cases, patients with swelling in maxilla, also presented painful symptoms, as in our case.4,5 We may speculate that the expansion observed in the maxilla of patient may favor an area of trauma and inflammation leading to a painful lesion.
Radiographic appearance of FOBMD is generally described as a sharply defined radiolucency with distinct sclerotic borders to extremely ill-defined areas. Trabeculations were occasionally visible within the radiolucent areas.1,8 The current case reveled an unusual radiographic finding, with an exuberant hiperdense areas, corresponding to trabeculae osseous component, what led to the suggestion of fibrous dysplasia in the incisional biopsy. As reported, fibrous dysplasia is commonly seen in maxilla, with slow growth, and a radiographic aspect of polish glass, as a result of superposition of some calcified trabeculae in a disorganized pattern, but it was not our case.10
The differential diagnosis of the classical appearance of osteoporotic bone is: odontogenic cystic lesions, aneurysmal bone cyst and metastatic carcinoma. All these conditions have a specific histological features which are not seen in the present case. This entity can be associated with other conditions such as impacted teeth, fibro-osseous lesions, osseous dysplasia, exostoses, enostoses, fibrous dysplasia, chronic osteomyelitis.1,3,10 These differential diagnoses of a classic FOBMD do not apply to this case, due to the unusual findings of the clinical and radiographic findings of this current FOBMD.
On the one hand, fibrous dysplasia was our first hypotheses in this case, which the most common site is maxilla, the cases are diagnosed during the first and second decades without any gender or racial predilection, characterized by painless osseous expansion with facial asymmetry, the radiographic features vary depending upon the stage of the disease. Early onset lesions are radiolucent and later progressively calcify, culminating in a “ground glass” or mottled mixed radiolucent/radiopaque pattern. The present case has some similarities with this condition as swelling and radiographic appearance, however the patient's age and facial asymmetry did not match. Our diagnosis hypothesis of FD was due to the clinical, radiographic and histopathology findings of the incisional biopsy. However, the fragments were probably removed only from the surface area of the lesion, leading us to a false diagnosis.
On the other hand, the lesion that should not be discharged during diagnosis process of this case is the osteoma. Osteoma is an osteoblastic benign tumor characterized by the proliferation of either compact or cancellous bone. Most of the cases reported in the literature are presented as peripheral solitary lesions, involving preferably the posterior region of the mandible. However, central osteomas are quite rare, especially in the maxillary bone. They are characterized by a well circumscribed mass composed by the proliferation of compact and/or cancellous bone, fibrovascular spaces, and may present a variable amount of marrow tissue. However, in the present case, it is a central lesion, not peripheral as it more common presentation of osteoma and the histological features shows an exuberant quantity of bone marrow tissue, which is not seen on osteoma.11
Microscopically, the tissue removed from the FOBMD defects consists of normal red marrow, fat marrow or a combination of the two. Megakaryocytes and small lymphoid aggregates may be present. The trabeculae of bone usually present are long, thin, irregular and devoid of an osteoblastic layer.1,8 In the present case, the presence of hematopoietic bone marrow and fat tissue permeated by trabeculae bone and areas with osseous repair demonstrated a long duration lesion. On the majority of the histological sections there was just a little area with loss of osteocytes in their lacunae. This could be due to the processing device, like on descaling step tissue.12
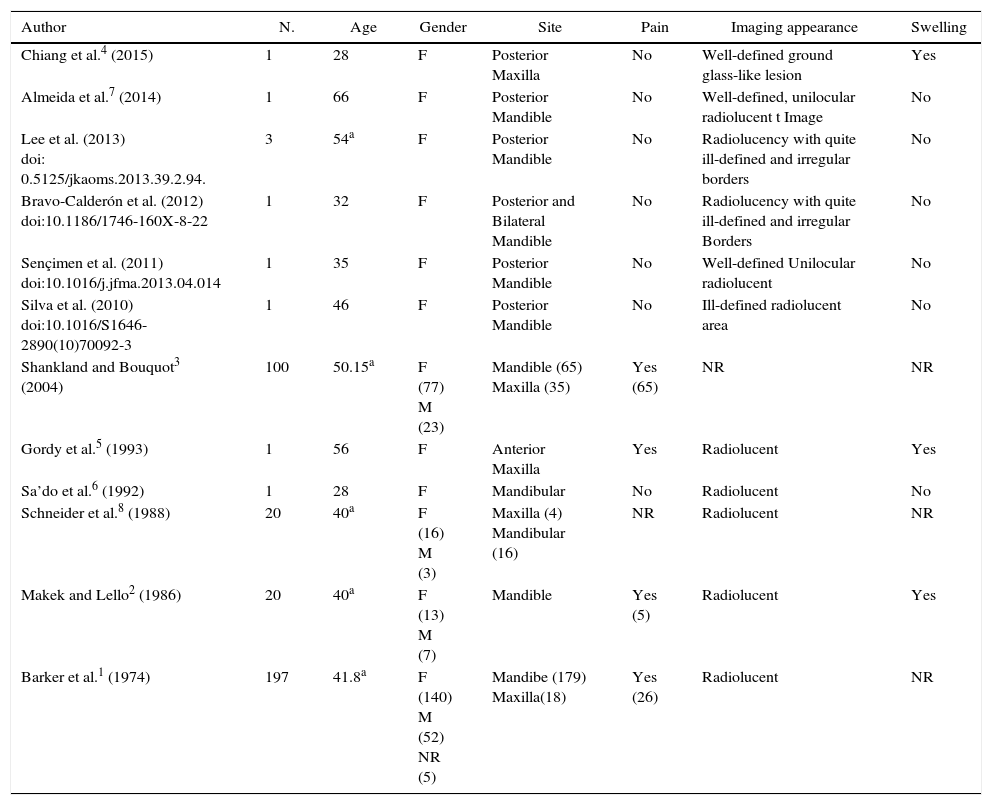
In our literature review, we found approximately 347 published cases of FOBMD. From these, the mean age was 43 years and the mandible was the most affected site (83%; n=288), generally without symptoms/swelling and with a radiolucent image (Table 1). In the present case the patient had difficulty in the maxillary prosthesis adaptation, due to a painful swelling that had been lasting for a year. Moreover, an extensive, symptomatic and well-defined hyperdense lesion was located in the maxilla. This lesion was protruding into the right maxillary sinus, which is an unusual site. These particularities for FOBMD are not commonly reported in literature.1,2,4
Focal osteoporotic bone marrow defect cases from the literature.
| Author | N. | Age | Gender | Site | Pain | Imaging appearance | Swelling |
|---|---|---|---|---|---|---|---|
| Chiang et al.4 (2015) | 1 | 28 | F | Posterior Maxilla | No | Well-defined ground glass-like lesion | Yes |
| Almeida et al.7 (2014) | 1 | 66 | F | Posterior Mandible | No | Well-defined, unilocular radiolucent t Image | No |
| Lee et al. (2013) doi: 0.5125/jkaoms.2013.39.2.94. | 3 | 54a | F | Posterior Mandible | No | Radiolucency with quite ill-defined and irregular borders | No |
| Bravo-Calderón et al. (2012) doi:10.1186/1746-160X-8-22 | 1 | 32 | F | Posterior and Bilateral Mandible | No | Radiolucency with quite ill-defined and irregular Borders | No |
| Sençimen et al. (2011) doi:10.1016/j.jfma.2013.04.014 | 1 | 35 | F | Posterior Mandible | No | Well-defined Unilocular radiolucent | No |
| Silva et al. (2010) doi:10.1016/S1646-2890(10)70092-3 | 1 | 46 | F | Posterior Mandible | No | Ill-defined radiolucent area | No |
| Shankland and Bouquot3 (2004) | 100 | 50.15a | F (77) M (23) | Mandible (65) Maxilla (35) | Yes (65) | NR | NR |
| Gordy et al.5 (1993) | 1 | 56 | F | Anterior Maxilla | Yes | Radiolucent | Yes |
| Sa’do et al.6 (1992) | 1 | 28 | F | Mandibular | No | Radiolucent | No |
| Schneider et al.8 (1988) | 20 | 40a | F (16) M (3) | Maxilla (4) Mandibular (16) | NR | Radiolucent | NR |
| Makek and Lello2 (1986) | 20 | 40a | F (13) M (7) | Mandible | Yes (5) | Radiolucent | Yes |
| Barker et al.1 (1974) | 197 | 41.8a | F (140) M (52) NR (5) | Mandibe (179) Maxilla(18) | Yes (26) | Radiolucent | NR |
N., number of cases; F, female; M, male; NR, not reported.
Although no treatment is necessary,5,6 incisional biopsy of FOBMD is eventually performed in order to rule out any pathological change.8 However, in our case, the presence of pain, swelling and the unusual image finding of the lesion motivated the completed resection of the lesion. A 2-year follow-up examination revealed no recurrence and the surgery site healed without complication, as usually observed in the literature.7
ConclusionFOBMD is generally a painless/no swelling condition that predominates in posterior mandible of middle-aged women, with no treatment required. When FOBMD presents with unusual findings a definite diagnosis requires microscopic examination of the tissue. The association of histopathological and clinical features is required to allow precise diagnosis of the condition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.