It has been related that only 7% of MCs are in contact with the mandible buccal cortex. This case report illustrates one mandibular canal with an atypical trajectory with fenestration at the buccal mandible cortex through a cone beam computed tomography exam from a 45 years old, Caucasian female patient, through ICat Vision® (Imaging Science International, Hatfield, PA) and InVivo software (Dental Anatomage, Version 5.1.10). This anatomic variation was not observed in the left side. Preoperative planning should consider a well-recommended cone beam computed tomography, which will allow identification of trajectory variations that are not visualized in panoramic radiographs.
São descritos que apenas 7% dos MC estão em contato com o cortical bucal mandibular. Este relato de caso ilustra um canal mandibular com trajetória atípica e fenestração na cortical bucal da mandíbula, através de um exame de tomografia computadorizada de feixe cónico em paciente, mulher, 45 anos de idade, leucoderma, obtido por ICAT Vision® (Imaging Science International, Hatfield, PA) e software InVivo (Dental Anatomage, versão 5.1.10). Esta variação anatómica não foi observada no lado esquerdo. O planeamento pré-operatório deve considerar a indicação da tomografia computadorizada de feixe cônico, o que irá permitir a identificação de variações de trajetória que não são visualizadas em radiografias panorâmicas.
Injuries to the inferior alveolar nerve (IAN) may be caused by nerve traction, trauma, bone screw placement, or cutting from instruments during surgical procedures.1 To avoid iatrogenic injuries to the IAN, the course, shape, curve, and direction of the mandibular canal must be considered, and damages may cause paresthesia and vessel injuries, bleeding, or hematoma.1–3 Sometimes, the mandibular canal (MC) course is close to the roots of the teeth or to the lower border of the mandible,4 and MC anatomical or trajectory variation has been described.3–5 Even though textbooks do not provide a detailed description of the MC course, it has been reported that nerve and vascular bundles may be close to the buccal cortex. It was related that 7% of the MC are in contact to mandible buccal cortex.6 The aim of this case report is to illustrate one unusual CM with an atypical trajectory at the buccal mandible cortex through a cone beam computed tomography (CBCT) exam.
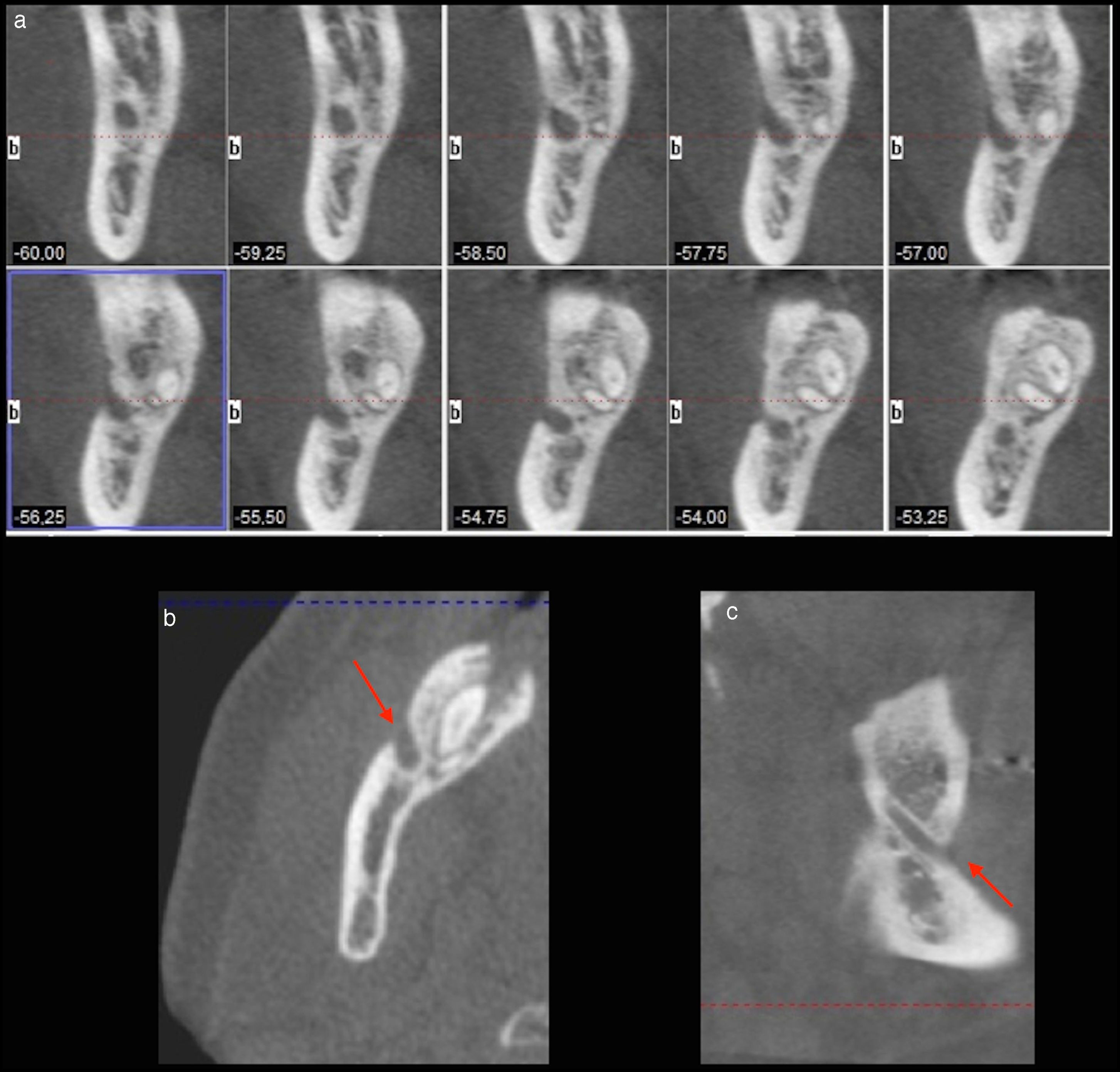
Case reportA 45-year-old Caucasian female patient was referred for a CBCT exam in order to evaluate jaw bone conditions prior to dental implant placement surgery. The scan was performed using an i-CAT Classic device t with 8cm×0.3 voxel size×20s of protocol scanning. During the evaluation of tomographic images using i-CAT Vision software (Imaging Science International, Hatfield, PA), an atypical IAN fenestration in the buccal right surface of the mandible was observed near the third molar, with 4.5mm of extension (Fig. 1). This anatomical variation was not observed on the left side. This IAN fenestration was a variation of the MC trajectory at the mandible buccal surface. There was no tomographic evidence of a MC bifurcation, no pathological process, and one exodontia 10 years ago. There was no other tomographic alteration.
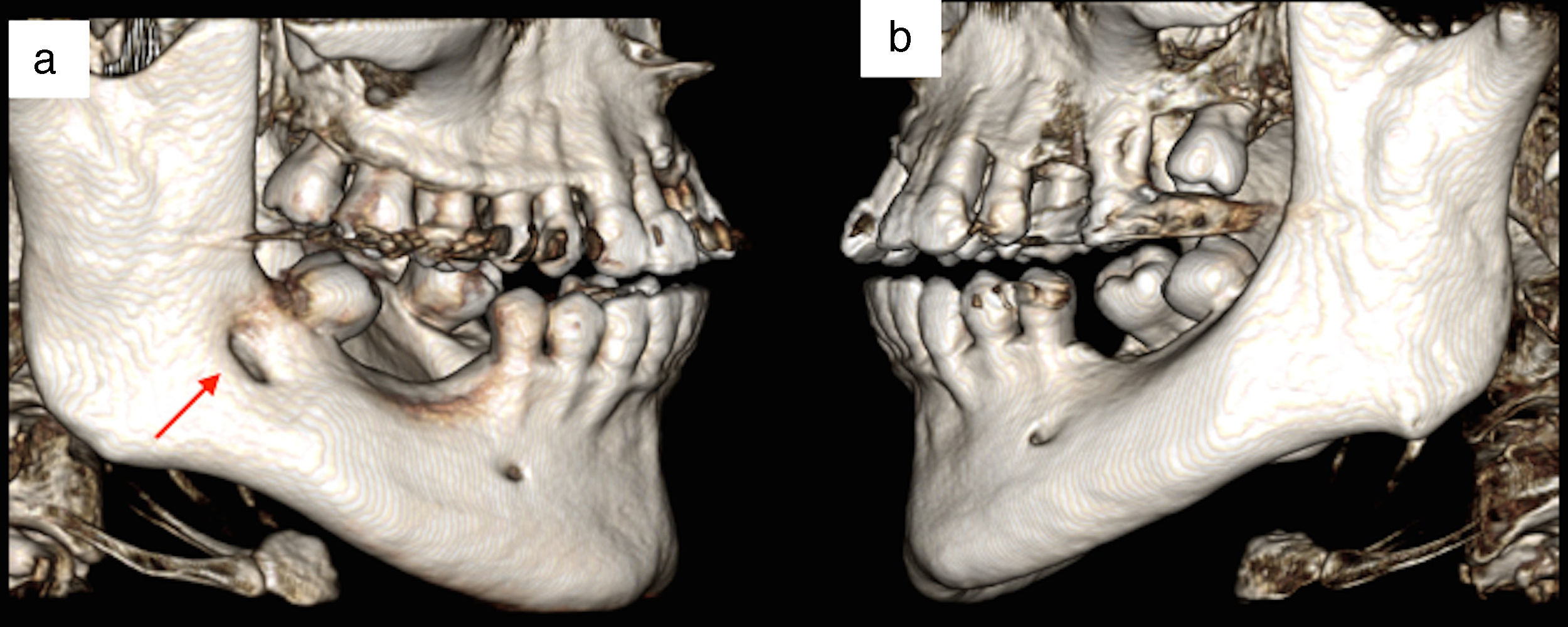
Tridimensional reconstruction was produced with InVivo (Dental Anatomage, Version 5.1.10) in order to illustrate and improve the observation of the MC and adjacent structures (Fig. 2).
DiscussionIn order to reduce complications related to IAN injury, an evaluation of pre-radiographs and tomographic exams must be considered to locate anatomical structures and their variation in the surgical area.1,6 Clinically, this kind of variation is important because many invasive procedures are performed in this area, such as implant placement, orthognatic surgery, dental extractions, and osteotomies. Knowledge of MC variation prevents injuries to the inferior alveolar neuromuscular bundle, which could cause traumatic neuroma, paresthesia, or bleeding.7,8 Therefore, if IAN fenestration is not identified may be a real concern during oral surgeries and postoperative period.
It was proved that it is easier to estimate MC position according to cortex with computed tomography (CT) than panoramic radiography, especially because conventional radiographs do not inform about thickness or location of anatomical structures in the buccolingual direction.2,6 Otherwise, 3D images allow evaluation of surface, shape, measurements, and magnification of anatomical structures,6,8 but the study of CM measures and dimensions is not well standardized, and there are a lot of methodologies for obtaining measurements.9 The main concerns regarding CBCT, CT, and other 3D exam modalities are amount of radiation and high cost.2 Anatomical variation associated with MC may cause complication during surgeries, but the use of new technologies, as CBCT, allow to planning and unmask this uncommon structures.
The mandibular canal is described as a well-defined radiolucent zone limited by radiopaque borders. The radiopaque borders’ definition depends on cortication and variables such as age, mandibular region, and surgical procedures.2,10 No relationship was found between cortication of the MC in panoramic radiographs and proximity to the mandibular buccolingual cortex.6
For Ylikontiola, MC is positioned close to the lingual cortex because it was observed that mean thickness between the MC and lingual cortex in the posterior area was 0.6mm and between the MC and the buccal cortex was 2.5mm. In a cadaveric study, it was observed that MC is near the buccal cortex in thin mandible rami, but vascular and nerve bundles may be close to the buccal cortex in cases of broad and thick rami.6 According to Balaji et al., the thickness of the mandibular buccal cortex is minor in the second molar level, under the influence of the masseter muscle.2 No significant difference was found in the distance of the MC and buccal cortical margin of the mandible between patients with or without prognatism.9 The mean distance of the MC and buccal cortex has also been described as increasing in the posterior to anterior direction.1 These findings are in agreement that in the posterior region the thickness of the area between the MC and the buccal cortex is minor in the mandibular posterior area. However, also it was found that MC course in posterior mandibular area close to lingual surface and traveled to anterior area bound to buccal surface.10
To highlight how uncommon buccal fenestration of the CM is, a study that examined 250 CBCT exams in order to report mandibular anatomical variations did not find any fenestration.11 Other study, tried to determine if age/sex could be related with IAN trajectory or with the presence of foraminas but it was prove that both occurs with no age/sex influence.12
In a case report of Tolentino et al.,5 a 49-year-old woman presented with one fenestration located in the canine region on the left side and another on the right side near the third molar region. The extension of fenestration was 6mm in the posterior area and 4mm in the anterior region. Both were possible to observe in the axial view and in a volume rendering. Any complication was related with these anatomical variations.5 Similar to our finds, was reported two clinical cases with fenestration in posterior area, both in a CBCT exam evaluation to dental implant placement.8 One case was found in a 58-year-old woman, located in left mandibular body, while the other was in a 68-year-old man billaterally also in mandibular body.8
One case of buccal fenestration was associated with a pathological process in a 20-year-old female patient with unilateral hemifacial microssomia of the left side. In orthopantomographic and 3D images, the MC and mental foramen were absent. During an intraoral surgical procedure, a neurovascular bundle was observed in the posterior lateral aspect of the mandible on the affected side.7
Like Tolentino et al. and Oliveira et al., we cannot affirm whether the IAN was exposed or was covered by the periosteum. Moreover, should be considered that a thin bony layer cannot be observed in CBCT exams, but still existing clinically. Tolentino et al.5 found fenestration bilaterally, and Oliveira et al. found two cases, one unilateral and the other bilateral.8 Most cases were found in female, middle-aged patients. Only one was associated with a pathological process, and all of them were anatomical findings.5,7,8
ConclusionBuccal cortex thickness is minor in the posterior region of the mandible, but cases of MC fenestration are extremely rare. MC buccolingual position and its measurements are better evaluated by CBCT and CT exams, demonstrating the responsibility of dentists to locate it and avoid possible IAN injuries during surgical procedures. In addition, more observational studies or even case reports are necessary to affirm the inclination of CM fenestration in the female gender.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.