Pure blowout fracture is an injury in which only one internal orbit wall is affected, without any compromise of the orbital rim or another region. The inferior and the medial walls are the most frequently affected areas. The patient usually presents diplopia, infraorbital nerve paresthesia and entrapment of soft tissue within the maxillary sinus, which leads to a possible limitation of the ocular movements and enophthalmos. Computer tomography scan is a helpful method for the diagnosis and qualification of this fracture. Whether the orbit reconstruction is indicated, natural and synthetic materials are available. We report a case of a 27 years old man, who was diagnosed with a pure blowout fracture after a physical aggression. The surgical treatment involved orbital floor reconstruction with a titanium mesh and under general anesthesia. The result was satisfactory and the patient does not show visual disturbances or paresthesia in six months follow-up.
Fractura Blowout pura ocorre quando apenas uma parede da o¿rbita é afectada, sem comprometer o aro orbital ou qualquer outra regia¿o. As paredes inferior e mesial sa¿o normalmente as áreas mais afectadas. O paciente geralmente apresenta diplopia, parestesia do nervo infra-orbital, aprisionamento de tecido mole dentro do seio maxilar, o que leva a uma possi¿vel limitac¿a¿o de movimentos oculares e enoftlamia. A tomografia computadorizada é um método u¿til para o diagno¿stico e qualificac¿a¿o desta fractura. Caso a reconstrução seja indicada, materiais sintéticos e naturais esta¿o disponi¿veis. O trabalho relata o caso de um homem, 27 anos de idade, em que foi diagnosticada uma fractura Blowout pura, apo¿s agressa¿o fi¿sica. O doente foi tratado sob anestesia geral por reconstruc¿a¿o do assoalho da o¿rbita com malha de tita¿nio. O resultado final foi satisfato¿rio e o paciente na¿o apresenta distu¿rbios visuais ou parestesia, num seguimento durante seis meses.
The term blowout fracture was first described in 19571 and it refers to a condition in which the displacement of an orbital wall occurs, but the orbital rim suffers no damage. Three different theories have been proposed to explain the mechanism of blowout fractures: globe-to-wall contact theory, hydraulic theory and bone conduction theory. Common symptoms of this fracture are diplopia, enophthalmos, dystopia, paresthesia of the infraorbital nerve, and soft tissue incarceration or entrapment, leading to restriction of ocular movements.2
The computed tomography is a radiological tool for evaluation of orbital fractures, which helps the surgeon to see if there is any incarceration or entrapment of soft tissue related to the orbit within the adjacent sinus. Repairing the orbital wall fractures is still a surgical problem, due to the drawbacks of the reconstruction materials and technical errors,3 such as misdiagnosis, timing of treatment as well as the accuracy during the repositioning of the soft tissue and the adaptation of the reconstruction material. In the treatment of blowout fractures, it is important to reconstruct and maintain the accurate anatomical structural support of the orbit, against herniation forces during the initial phase of healing to obtain a functional and an esthetic result. Joining and stabilizing small, thin and delicate bone fragments is usually impossible.4 Therefore, natural and synthetic materials, like autogenous bone and titanium mesh, are available to reconstruct the orbital walls when it is necessary. The choice is based on the surgeon's experience and the availability of the material. We describe a clinical case of orbital floor reconstruction, with a titanium mesh as a treatment option for pure blowout fracture.
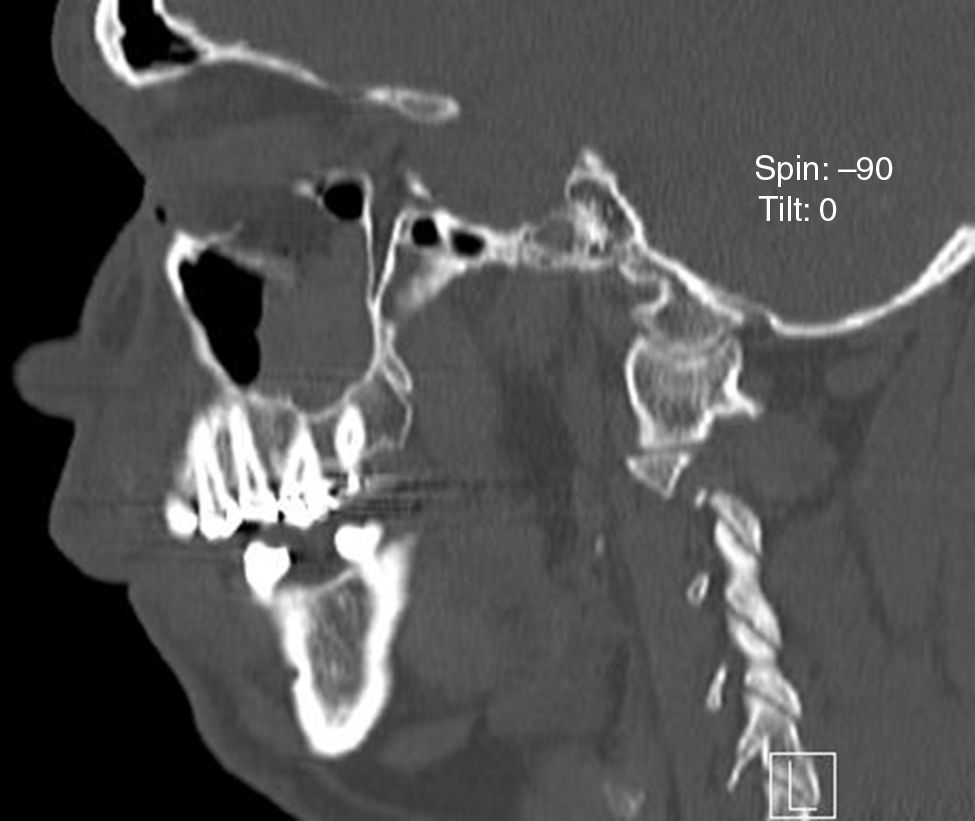
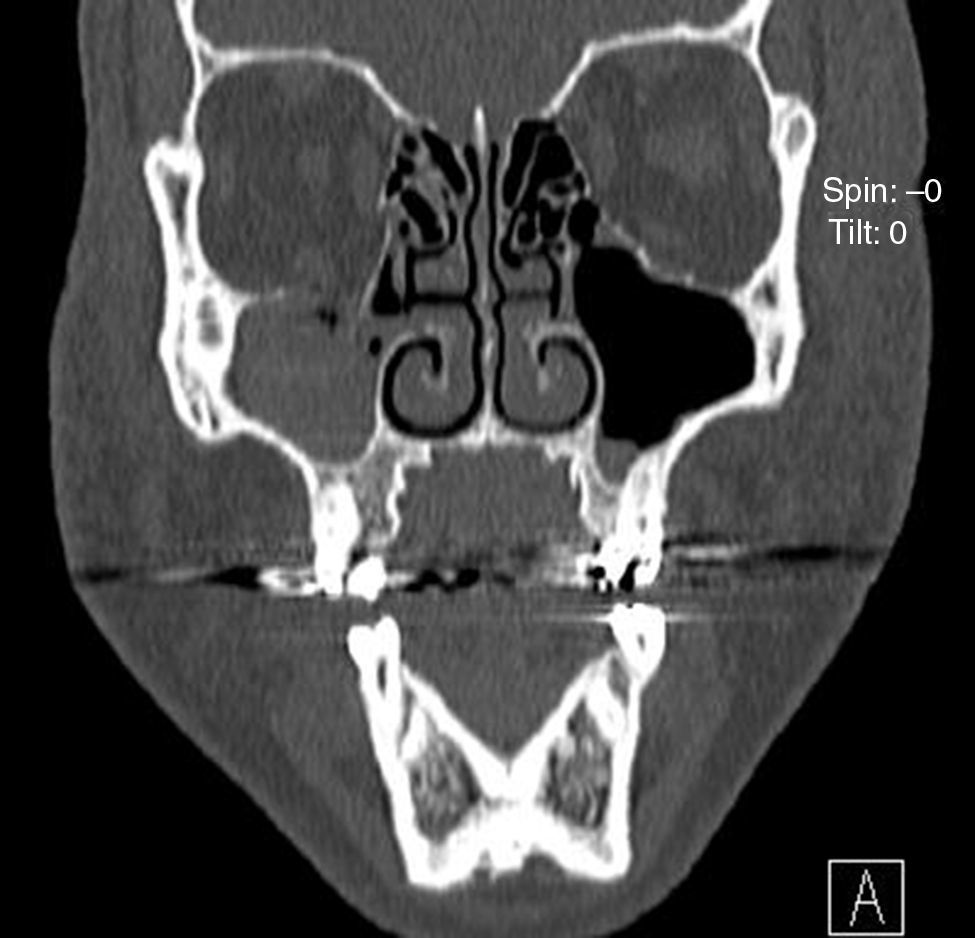
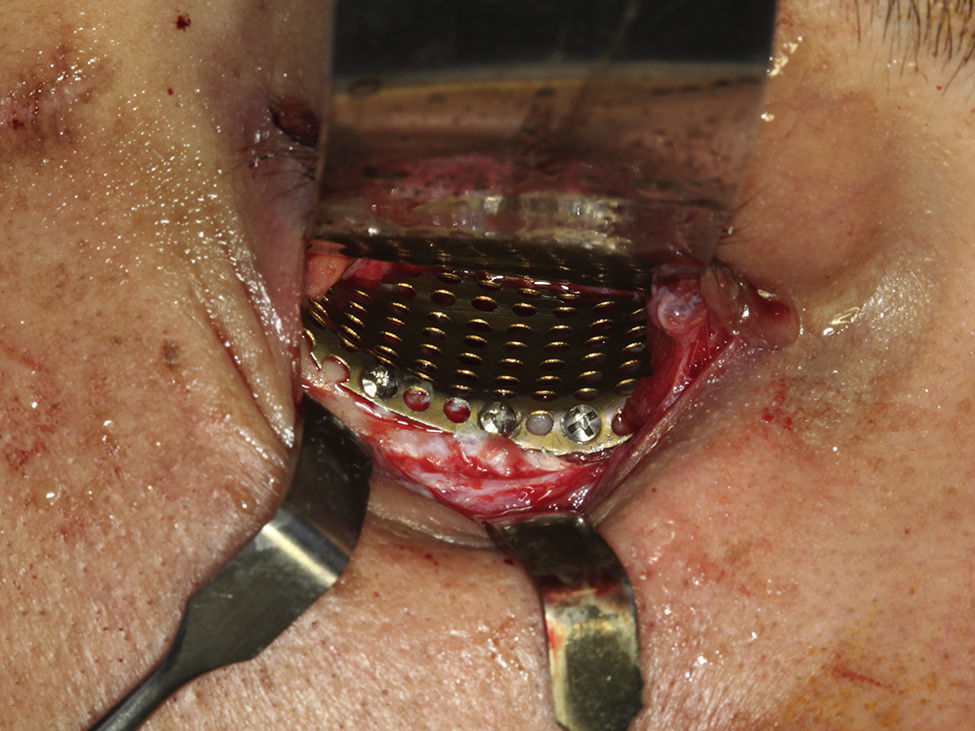
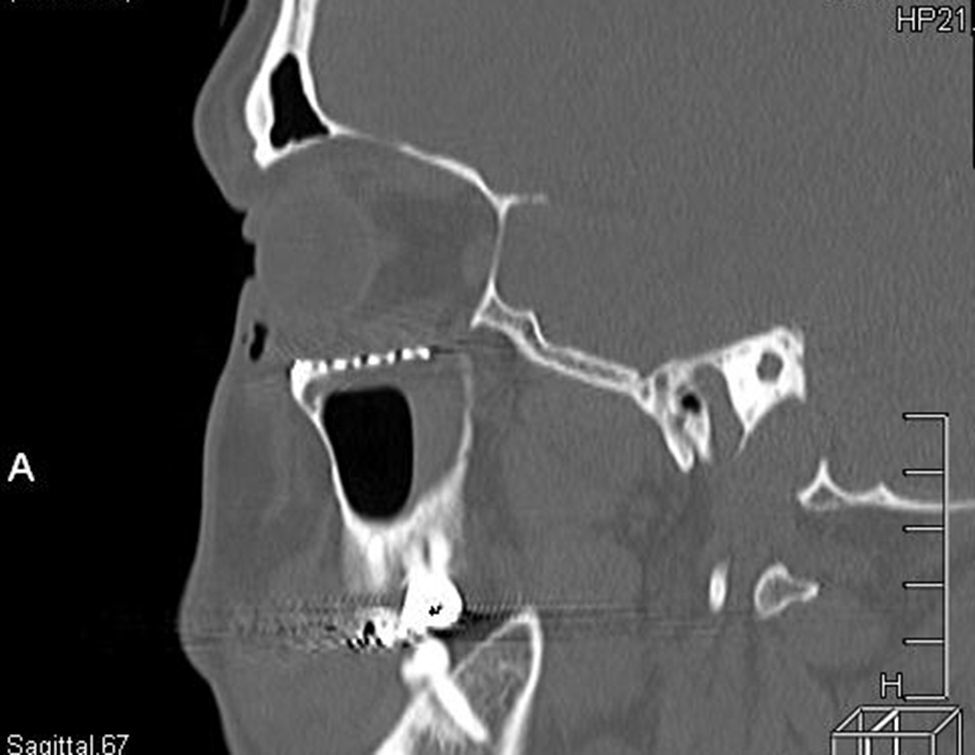
Case reportA 27 year old man was examined at the Oral and Maxillofacial Surgery Department of the University Hospital of Uberlândia after physical aggression. He was submitted to a clinical evaluation and showed orbital ecchymosis, paresthesia of the infraorbital nerve and diplopia during vertical and horizontal ocular movements. Nevertheless, no ocular movement restriction was found. A computed tomography scan was done and it revealed a blowout fracture of the floor of the right orbit and a herniation of the orbital soft tissue into the maxillary sinus (Figs. 1 and 2). A week after the trauma, the patient was submitted to a reconstruction of the orbital floor, under general anesthesia. A tarsorrhaphy suture was used, to protect the cornea during the operative procedure, followed by a subtarsal approach to access the orbital floor (Fig. 3). The herniated soft tissue was repositioned and the orbital floor defect covered with a trapezoidal titanium mesh with approximately 25mm on the orbit margin and 20mm on the posterior width (Neo-ortho, Curitiba, PR, Brazil), which was fixed on the orbital rim with 3 monocortical, 1.5mm profile (Neo-ortho, Curitiba, PR, Brazil), 2 screws of 5mm and 1 screw of 4mm (Fig. 4). A forced duction test was conducted with a negative result and the globe mobility was intact. A 6-0 non-resorbable suture (nylon, ETHICON®, Johnson & Johnson, USA) was used along the skin margin. There were no complications and the patient was discharged 1 day after surgery. A computed tomography scan was carried out after the surgery, showing a satisfactory repositioning of the soft tissue previously herniated and a good adaptation of the titanium mesh (Figs. 5 and 6). The patient remained under surveillance for six months, with no complaint of paresthesia, no signs of visual disturbances or diplopia.
The mechanisms, which lead to blowout fractures, have been the aim of many researches. However, no consensus has been achieved until now. A study published in 19435 supported the globe-to-wall contact theory, reporting 24 cases of internal fracture of the orbit, and explained that the posteriorly displaced eyeball transmitted the force of a blow directly to the orbital wall. In 1957, it was proposed the hydraulic theory,6 according to which blowout fractures are caused by the increase of intraorbital pressure. Finally, the bone conduction theory, first proposed in 1972,7 suggested that the trauma to the infraorbital rim may transmit force directly to the thinner orbital floor, causing disruption of the bone without fracture of the rim.
In 1999, a group of researchers8 showed that both, the “hydraulic” and the “buckling” mechanisms can be validated and concluded that the fracture patterns differed between impact on the orbital rim, versus directly on the globe. The “hydraulic” mechanism produced larger fractures with the involvement of the floor and medial wall, where the herniation of orbital contents was frequent. The “buckling mechanism” produced smaller fractures involving the medial wall, without significant orbital content herniation. Accordingly, this case report would be related to the “hydraulic” theory, as the orbital floor was extensively damaged and the herniation of the soft tissue was present.
The indications for surgical exploration of the fractured orbital floor include: enophthalmos, limitation of extraocular muscle function, large orbital floor defect with herniation of the soft tissue into the maxillary sinus and deformity along the infraorbital margin with paresthesia of the infraorbital nerve causing numbness.9 If the reconstruction of the orbital floor is not performed or if it is postponed, the herniated or entrapped soft tissue can initiate the healing process and a contracture of these tissues can occur leading to ocular movement restriction and visual disturbances. Not only did our patient present herniation of the soft tissue, but also paresthesia of the infraorbital nerve and diplopia during horizontal and vertical ocular movements, therefore he was submitted to a surgical treatment.
The computed tomography scan is a helpful instrument for the diagnosis of the pure blowout fracture. During 28 months, at the University Hospital of Geneva, a study10 described and evaluated the reliability and the accuracy of a specific computed tomography-based assessment, in predicting treatment decisions for pure orbital floor blowout fractures. This study showed that the severity of the inferior rectus muscle displacement, observed on the computed tomography scanning, is the most important independent predictive radiologic factor in decision making of the treatment for pure blowout fracture.
Numerous materials, natural and synthetic substances, are available for reconstructing damaged orbital walls, to restore orbital volume. The ideal material is the one that has biomechanical properties and which better replicates the tissue it replaces. Rigid materials are best suited for reconstruction of large defects, to prevent sagging and displacement into the maxillary antrum.11
Autogenous bone grafts, such as calvarium and iliac crest, are useful to repair facial bone defects, because of their strength, biocompatibility and osteogenic, osteoconductive, and osteoinductive potential. They share disadvantages like donor site morbidity, variable resorption rate, limited quantity and difficulty in molding in the appropriate shape. Moreover they are resistant to infection, give good structural support and are not rejected.3 The cortical bone from the calvarium satisfies the requirement of rigidity besides, its curvature is useful for floor reconstruction although its rigidity makes contouring nearly impossible.11
In what concerns resorbable systems, a resorbable mesh plate used for orbital floor reconstruction has many advantages. It is easy to sculpt to fit in the defect and the operative time is significantly decreased. The low profile of the implant prevents postoperative proptosis and globe dystopia. Radiolucency of the system allows postoperative imaging without metallic artifact. Besides, the main superiority of the use of a resorbable mesh system in orbital floor fracture, is the maintenance of orbital contents against herniation forces, during the initial phase of healing and complete resorption from the region, after it is no longer needed.4
According to a manuscript published in 2003,12 the ability of titanium mesh to conform to the contours of the orbit makes it a better material for reconstructing not only isolated floor fractures but also those defects that involve both the floor and medial wall and this is partially based on the finding that many of the bone grafts used are too thick: decreasing orbital volume compared with the uninjured side and also elevating the floor in the anterior orbit creates an adverse effect elevating the globe.
Finally, the titanium mesh has good biocompatibility and is easily adjustable. It is easy to trim and shape exactly to the orbital contour. Moreover, with this mesh structure, connective tissue can grow around and through the implant, preventing its migration and it can be reliably fixed with screws in areas such as the infraorbital border.13 About the rigidity presented by titanium mesh and cranial bone grafts, both seemed to bridge the defects without sagging or changes in shape, differing from the titanium “screen” that was considered too thin and did not present enough rigidity for large defects.12 As we have titanium mesh at our disposal in our hospital and to avoid the morbidity of a donor site, we used this material to reconstruct the orbital floor. This is in accordance with a retrospective study developed at Parkland Memorial Hospital12 that concluded that orbits reconstructed with titanium mesh, show better overall reconstructions than those reconstructed with bone grafts.
The goals of the orbital fracture treatment are not only to free incarcerated soft tissue, but also to restore the anatomy and volume of the internal orbit and to prevent damages like permanent paresthesia and enophthalmos. The clinical evaluation, in association with the appropriate radiologic examination, should guide the maxillofacial surgeon through the case resolution and whenever a surgical treatment is necessary, the approach and the material used for reconstruction should be one which leads to a minor morbidity and greater stability for the patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.