The aim of this in vitro study was to evaluate the effect of different surface treatments on the resin–resin bond strength of a composite resin previously contaminated with blood.
MethodsSixty bar-shaped specimens were fabricated. Two 2-mm-thick layers of an A3.5 shade composite (TPH3) were inserted on a silicon matrix, photoactivated and subjected to different surface treatments (n=12): (1) no contamination, control; (2) blood contamination and air drying; (3) blood contamination, rinsing with water, and air drying; (4) blood contamination, rinsing with water, air drying, and application of the bonding agent of an adhesive system (Adper Scotchbond Multi-Purpose Adhesive); and (5) blood contamination, rinsing with water, air drying, phosphoric acid etching, and application of the bonding agent of an adhesive system. Then, two 2-mm-thick layers of an A1 shade composite (TPH3) were inserted and photoactivated. After storing in water for 24h, the samples were subjected to a microtensile bond strength test in a universal testing machine. Failure modes were evaluated in a stereomicroscope. Data were analyzed using one-way ANOVA and the Tukey test (p<0.05).
ResultsThere were statistically significant differences between the treatments. Blood contamination and air drying provided the lowest bond strength values; only blood contamination, rinsing with water, air drying, phosphoric acid etching, and application of the bonding agent of an adhesive system provided bond strength similar to the control.
ConclusionsThe use of a full adhesive protocol involving phosphoric acid etching and the application of the bonding agent of an adhesive system provided adequate resin–resin bond strength of the composite tested.
Este estudo in vitro objetivou avaliar o efeito de diferentes tratamentos de superfície na resistência adesiva de um compósito previamente contaminado com sangue.
MétodosSessenta amostras em forma de palito foram confeccionadas, dois incrementos de 2mm de espessura de um compósito de cor A3,5 (TPH3) foram inseridos numa matriz de silicone, fotoativados e submetidos a diferentes tratamentos superficiais (n=12): [1] nenhuma contaminação – controle; [2] contaminação com sangue (CS) e secagem com ar; [3] CS, lavagem com água e secagem com ar; [4] CS, lavagem com água, secagem com ar e aplicação de uma resina hidrófoba de um sistema adesivo (Adper Scothbond Multi-Purpose); [5] CS, lavagem com água, secagem com ar, condicionamento com ácido fosfórico e aplicação da resina hidrófoba de um sistema adesivo. Posteriormente, dois incrementos de 2mm de espessura de um compósito de cor A1(TPH3) foram inseridos e fotoativados. Após 24 horas de armazenamento em água, as amostras foram submetidas ao teste de resistência à microtração numa máquina de ensaios universal. O padrão de fratura foi avaliado em um estereomicroscópio. Os dados foram analisados utilizando-se ANOVA a um critério e teste de Turkey (p<0,05).
ResultadosHouve diferenças estatisticamente significativas entre os tratamentos. CS e secagem propiciaram os menores valores de resistência de união, enquanto apenas o tratamento CS, lavagem com água, secagem, condicionamento com ácido fosfórico e aplicação da resina hidrófoba de um sistema adesivo promoveram resistência de união similar ao controle.
ConclusãoEm situações de contaminação com sangue, o uso de um protocolo adesivo completo envolvendo o condicionamento com ácido fosfórico e a aplicação da resina hidrófoba de um sistema adesivo propiciou uma resistência adesiva entre incrementos de resina adequada.
Filling with composite resin is a technically sensitive procedure involving several operational steps that need to be well executed to obtain successful long-term results. One of these steps is appropriate isolation of the operative field to prevent contamination during the filling procedure.1 Contamination can occur at several stages of the procedure and in different substrates (enamel, dentin-prepared surfaces and/or the layers of composite resin), and various fluids, including blood, can reduce the union.2
The union between composite resin layers is possible due to the presence of residual monomers and free radicals in light-cured composite.3 However, when blood contamination occurs on a composite resin layer during insertion and light curing, before the final layer of the filling, the union between the resins layers can be compromised causing the treatment to fail. In fact, the blood can act as a contaminant in adhesive interfaces, which would decrease the bond strength between resin–resin increments.3
Studies have been carried out on blood contamination on tooth surfaces when using adhesives4–7 or adhesive self-etching, but it is not known if phosphoric acid improves resin–resin bond strength and there is a lack of information about the effect of blood contamination between layers of light-cured composites resin.3
This in vitro study aimed to evaluate the effects of blood contamination on resin–resin bond strength between layers of composite using a microtensile test and to determine the best surface treatment method to re-establish the strength of the union between layers. The null hypothesis that was tested on this study is that there is no statistically significant difference between the treatments.
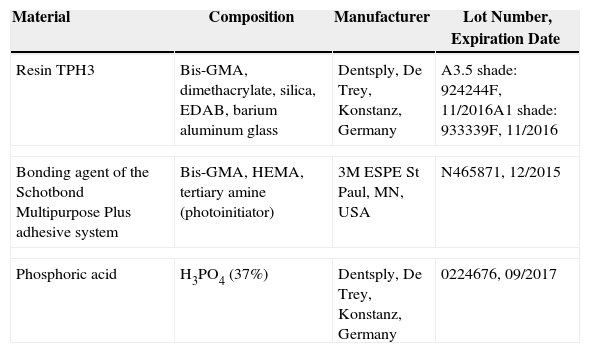
Materials and methodsThis study evaluated the resin–resin bond strength between composite resin layers according to the surface treatment used to clean the increment after blood contamination. The following cleaning protocols were tested: (a) air drying; (b) rinsing with water and air drying; (c) rinsing with water, air drying and application of a bonding agent; and (d) rinsing with water, air drying, phosphoric acid etching and application of a bonding agent. The materials that were used are described in Table 1.
Materials used in the study.
| Material | Composition | Manufacturer | Lot Number, Expiration Date |
|---|---|---|---|
| Resin TPH3 | Bis-GMA, dimethacrylate, silica, EDAB, barium aluminum glass | Dentsply, De Trey, Konstanz, Germany | A3.5 shade: 924244F, 11/2016A1 shade: 933339F, 11/2016 |
| Bonding agent of the Schotbond Multipurpose Plus adhesive system | Bis-GMA, HEMA, tertiary amine (photoinitiator) | 3M ESPE St Paul, MN, USA | N465871, 12/2015 |
| Phosphoric acid | H3PO4 (37%) | Dentsply, De Trey, Konstanz, Germany | 0224676, 09/2017 |
Sixty specimens of composite resin measuring 1.5×1.5×8.0mm3 were prepared. A cylindrical matrix (12×8mm2) with silicon to create a rectangular internal space (1.5×1.5×8.0mm3) was juxtaposed to a Teflon structure measuring 12×8mm2. The Teflon structure allows the depth of the central band to be set in millimeters. Every two complete turns of this band provided 2mm depth. The Teflon structure was rotated four times, each with two turns, resulting in specimens measuring 8mm in length.
Initially, the Teflon structure was rotated twice, providing a depth of 2mm, allowing the silicon matrix to adjust to the slot. The first composite resin layer (TPH3, shade A3.5; Dentsply, De Trey, Konstanz, Germany) was then added to a thickness of 2mm with the aid of a spatula, which was also used to remove possible excess and make a relatively flat surface. The layer was then light cured for 20s using a light-emitting diode (LED) device (Coltolux LED, Colténe, Suíça; 800mW/cm2). The Teflon structure was then rotated again with two turns to move the silicon matrix and the first layer down before the addition and light curing of the second layer of resin (shade A3.5, 2-mm thick) as described above.
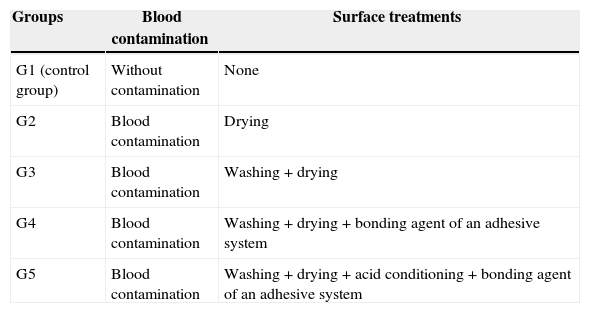
The specimens were divided randomly into five groups (12 specimens per group), according to the contamination and surface treatment (Table 2): group 1 (G1), control group, the specimens were not contaminated by blood; groups 2, 3, 4 and 5 (G2, G3, G4 and G5, respectively) were contaminated with human blood that was collected via a needle prick on the finger of the operator at the time of the experiment. One drop of blood was applied using a disposable brush (KG Sorense) for 15s.
Details of the groups based on superficial treatment of resin layers and blood contamination.
| Groups | Blood contamination | Surface treatments |
|---|---|---|
| G1 (control group) | Without contamination | None |
| G2 | Blood contamination | Drying |
| G3 | Blood contamination | Washing+drying |
| G4 | Blood contamination | Washing+drying+bonding agent of an adhesive system |
| G5 | Blood contamination | Washing+drying+acid conditioning+bonding agent of an adhesive system |
After the contamination, each group (G2, G3, G4 and G5) received a different superficial treatment as follows:
- •
G2. After blood contamination, the specimens were dried with an air jet for 20s applied with a triple syringe positioned 10cm from the layer, leaving a layer of dried blood on the surface of the resin.
- •
G3. After blood contamination, the specimens were washed with air/water jets from a triple syringe for 15s and dried for 20s with air jets from the triple syringe positioned 10cm from the surface.
- •
G4. After blood contamination, the specimens were washed with air/water jets from a triple syringe for 15s and dried for 20s with air jets from the triple syringe positioned 10cm from the surface. The bonding agent of Scotchbond Multi-Purpose Adhesive System (3M ESPE St Paul, MN, USA) was applied in two layers using a disposable brush. A soft air jet was applied for 2sec followed by light curing for 20s using a light-emitting diode (LED) device (Coltolux LED, Colténe, Suíça; 800mW/cm2).
- •
G5. After blood contamination, the specimens were washed with air/water jets from a triple syringe for 15s and dried for 20s with air jets from the triple syringe positioned 10cm from the resin. The surface was conditioned with phosphoric acid 37% (Denstply, De Trey, Konstanz, Germany) for 15s and was washed with air/water jets from a triple syringe for 20s and dried for 20s with the air jets from the triple syringe positioned 10cm from the resin. The bonding agent of Scotchbond Multi-Purpose Adhesive System (3M ESPE St Paul, MN, USA) was then applied in two layers using a disposable brush (KG Sorense). A soft air jet was applied for 2s followed by light curing for 20s using a light-emitting diode (LED) device (Coltolux LED, Colténe, Suíça; 800mW/cm2).
After the surface treatments, two more layers of resin (TPH3, shade A1, 2.0-mm thick) were added to all the composite resin blocks in the same manner as before the blood contamination. The blocks were light cured for 60s using a light-emitting diode (LED) device (Coltolux LED, Colténe, Suíça; 800mW/cm2). The finished specimens were immersed in containers with distilled water and stored for 24h at 37°C.8
At the end of the storage time, the specimens were fixed onto the grips of a microtensile device with cyanoacrylate-based glue (Super Bond Gel, Loctite Brazil, Ltda) and an acrylic resin monomer-based accelerator (Dêncor, Clássico Ltda, São Paulo, Brazil) following the long axis of the set (resin/resin), perpendicular to the base.
The microtensile test was performed using an Instron Universal Test Machine (Model 4411, Instron, Canton, USA) at a speed of 1.0mm/min until the specimen ruptured. The microtensile values were initially expressed in kilograms-force. After the tests, the values were converted into megapascals (MPa).
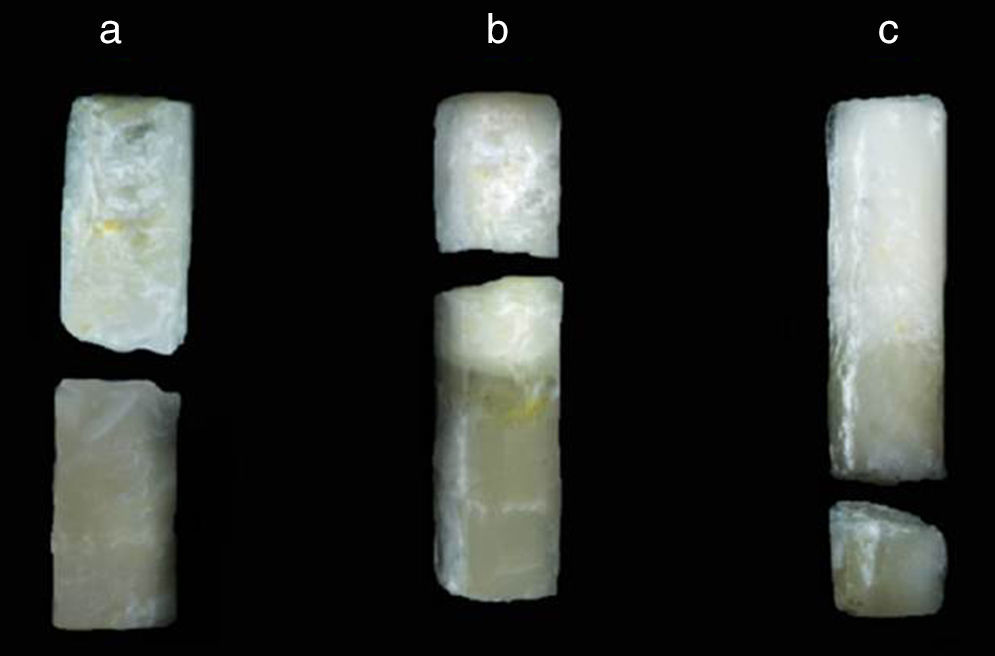
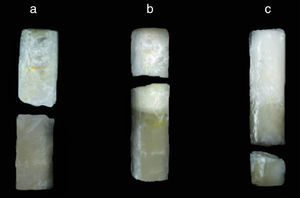
After the microtensile test, fractured specimens were examined with a stereomicroscope (Olympus SZ-CTV; Olympus, Tokyo, Japan) at 40× magnification to determine the mode of failure. The failure patterns were classified into two types: (1) failure on the resin A1/resin A3.5 interface (Fig. 1a); (2) cohesive failure on composite corresponding to color A1 (Fig. 1b) or A3.5 (Fig. 1c). Prematurely debonded specimens were registered with a bond strength of 0MPa.
Data distribution was analyzed using the Kolmogorov–Smirnov test and found to be normal. Further, data were analyzed using one-way ANOVA and the Tukey test (p<0.05). All data were analyzed using ASSISTAT Beta 7.5 (UFCG, Campina Grande, Brazil).
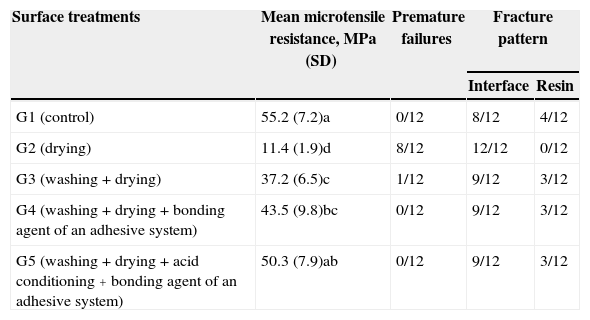
ResultsThere were statistical differences between the groups (p<0.05) (Table 3). The only treatment that presented results similar to the control group was G5 (washing+drying+phosphoric acid+bonding agent of an adhesive system). Surface treatment only with drying the surface contaminated with blood (G2) had the lowest values for cohesive strength.
Mean microtensile resistance in MPa (standard deviation), number of premature failures and failure modes according to the type of surface treatment.
| Surface treatments | Mean microtensile resistance, MPa (SD) | Premature failures | Fracture pattern | |
|---|---|---|---|---|
| Interface | Resin | |||
| G1 (control) | 55.2 (7.2)a | 0/12 | 8/12 | 4/12 |
| G2 (drying) | 11.4 (1.9)d | 8/12 | 12/12 | 0/12 |
| G3 (washing+drying) | 37.2 (6.5)c | 1/12 | 9/12 | 3/12 |
| G4 (washing+drying+bonding agent of an adhesive system) | 43.5 (9.8)bc | 0/12 | 9/12 | 3/12 |
| G5 (washing+drying+acid conditioning+bonding agent of an adhesive system) | 50.3 (7.9)ab | 0/12 | 9/12 | 3/12 |
Averages followed by different letters indicate statistically significant differences between treatments (p<0.05).
With regard to the fracture patterns, there was a predominance of failure at the interface independently of the superficial treatment. However, G2 (drying only) had the highest number of premature failures (Table 3).
DiscussionSince there were statistically significant differences between the treatments, the null hypothesis that – there is no statistically significant difference between the treatments – was rejected.
The union of resin layers, newly embedded on a cavity and light cured to new layers, is possible due to the presence of residual monomers and free radicals on the polymerized composite resin.9 However, if the resin surface is contaminated, these monomers and radicals may react with the contaminating agent making the union of resin increments impossible or inefficient.
This study evaluated the effect of blood contamination on the surface of light-cured resin layers, before the addition of new layers, simulating the filling procedure using polychromatic (shades A1 and A3.5) composite, by measuring microtensile strength.
Blood consists of plasma (66% by volume) as well as red cells, leukocytes and platelets (33%). There are methodologic differences in studies involving composite contamination with blood, so that fresh blood is considered the more appropriate for laboratory experiments6,9,10 than heparinized blood6 because the addition of anticoagulant may reduce the resin–resin strength.10 Therefore, the blood used as the contaminant in this study was collected at the time of the experiment.
The influence of blood contamination on the bond strength between composites can be attributed to its high level of protein and macromolecules such as fibrinogen and platelets that can form a film on the surface of substrates, weakening the bond.11 When only drying was performed alone (G2), it is likely that the air treatment may not have removed the blood completely from the contaminated resin surface and the presence of this contaminant between resin layers may have led to a significant decrease in cohesive strength.
These results are strengthened by the fracture pattern observed, with the prevalence of a large number of failures (8 of 12) before the microtensile test, demonstrating the vulnerability of bonding between resin and resin contaminated with blood when only drying was performed. This result was similar to the results of another study, which was also noted that only the blood drying procedure had a bad effect, resulting in a reduction of the adhesive strength between resin layers.8
Regarding the washing and drying processes (G3), an increase in the resin–resin bond strength was noted compared with only drying process (G2), although the resin–resin bond strength has not been similar to that presented by the control group. Eiriksson and others autors8 observed that washing and drying the contaminated surface restored the bond strength of Pertac II resin but not Z250, Renew or APX, showing that different results are obtained using the same decontaminant but different types of resins. It has been hypothesized that the co-polymerization of resin increments is impaired by washing and drying the contaminated substrate, since they remove the oxygen from the superficial resin layer.12 Another possible explanation refers to the fact that both the blood protein components and the water were not completely removed, causing a reduction in the superficial stress on the composite and, consequently, lower adhesion of polymerized composite to the next resin layer.12
Previous investigations showed the effects of blood contamination7–9,13–15 between composite resin and tooth surfaces (enamel and/or dentin). Many studies reported that the application of adhesive after washing and drying the contaminated surface increased significantly the adhesive strength between the resin composite layers and the tooth structure, increasing the longevity of the filling.7,15,16 It is believed that this occurs because the application of adhesive (reagent monomers) enables chemical bonding of the decontaminated monomers with the subsequent resin layers.8
The application of the bonding agent of an adhesive after washing and drying the contaminated surface (G4) resulted in increased resin–resin microtensile bond strength. However, even this process having proven resin–resin bond strength similar to other treatments [washing+drying (G3) and washing+drying+acid conditioning+bonding agent of an adhesive system (G5)], it was not able to provide resin–resin bond strength similar to the control group. On the other hand, only washing+drying+acid conditioning+bonding agent of an adhesive system treatment (G5) was capable to provide similar resin–resin microtensile bond strength to the control group. Although phosphoric acid does not significantly modify the morphologic pattern of composite resin surfaces,16 one possible explanation for the high resistance values is that the acid acts as an additional cleansing agent, and in addition to washing before and after conditioning, the contaminating agent is completely removed, enabling strong adhesion.
ConclusionsWithin the limitations of this study, it is concluded that contaminated surfaces must not be treated only with drying because this treatment showed the worst strength. The use of phosphoric acid and the application of the bonding agent of an adhesive system presented results similar to the control group, ensuring better resin–resin bond strength between composite resin layers contaminated with blood.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflict of interest to declare.
The authors thank Dentsply for providing the composite resin used in this study.