Intraoral administration of local anesthetics is one of the most common dental procedures. Although this procedure is well known for its safety, complications can still occur. A 17-year-old female patient developed transient diplopia and ipsilateral lateral rectus muscle paralysis following administration of local anesthesia for right maxillary third molar extraction. The patient was informed and proper instructions were given regarding the complications. Complete resolution occurred within 2h. In this article, we review the clinical examination and management of this uncommon occurrence.
A administração intraoral de anestésicos locais é um dos procedimentos dentários mais comuns. Embora este procedimento seja bem conhecido pela sua segurança, complicações podem ocorrer. Paciente do sexo feminino, de 17 anos de idade, desenvolveu diplopia temporária e paralisia músculo reto-lateral ipsilateral após a administração de anestesia local para a extração do terceiro molar superior direito. A paciente foi informada e orientações adequadas foram passadas a respeito da complicação. A resolução completa ocorreu dentro de 2h. Neste artigo vamos rever o exame clínico e o tratamento desta ocorrência incomum.
Although local anesthesia is routinely used in daily dental practice, occasionally patients may present with complications associated with its administration. These complications may have local effects (trismus, hematoma, edema, facial nerve paralysis, burning upon injection, postanesthetic intraoral lesions, infections, soft tissue injury, sloughing of tissues, needle breakage, anesthesia failure, and ophthalmologic complications)1 or systemic effects (headache, syncope, allergy, and undesirable cardiovascular effects).2
Typical ophthalmologic complications after intraoral local anesthesia include accommodation disturbance, amaurosis (loss of sight), diplopia (double vision), enophthalmos (recession of the eyeball), miosis (contraction of the pupil), mydriasis (dilation of the pupil), ophthalmoplegia (paralysis of all muscles responsible for eye movements), and ptosis (drooping of the upper eyelid). Generally, these ophthalmologic complications have an immediate to short onset and disappear as the anesthesia subsides. These symptoms are most often attributed to the anesthetic solution reaching the orbit or nearby structures.3 Among the documented ophthalmologic complications, diplopia (39.8%) occurred most frequently, while ptosis (16.7%), mydriasis (14.8%), and amaurosis (13.0%) were less common. Other ophthalmologic complications such as accommodation disturbance, enophthalmos, miosis, and ophthalmoplegia were reported only in very few cases.4
Based on the extent of the surgical procedure, a specific technique for injection of anesthetic is chosen. When the procedure involves a small area, infiltration anesthesia may provide the necessary effect. On the other hand, a nerve block will provide enough anesthesia for a procedure involving two or three teeth, which is the case for third molar extractions.5 Regional block anesthesia is recommended for pain control during quadrant treatment and surgical procedures.5 The maxillary nerve block may also be used for extraction of superior third molars.
Complications associated with this type of anesthesia include damage to blood vessels and hematoma formation caused by perforation of the maxillary artery or penetration of the needle too far distally, reaching the pterygoid plexus; volume displacement of the orbital structures, producing periorbital swelling and proptosis; classic retrobulbar block, producing mydriasis, corneal anesthesia, and ophthalmoplegia; and regional block of the sixth cranial nerve, producing diplopia.5 When the abducens nerve (the sixth cranial nerve VI: CNVI) is damaged, the patient loses their ability to orientate the eye laterally and they are not able to abduct the eye on the affected side. This negative effect is due to the fact that the CNVI supplies somatic motor and proprioceptive fibers to the lateral rectus muscle which is responsible for lateral movement (abduction) of the eye.6 If this muscle is paralyzed by regional anesthesia, the patient may experience convergent strabismus (esotropia) and diplopia. The ocular muscles can also be indirectly affected during anesthesia of the maxillary nerve via the greater palatine canal, the infratemporal fossa, or the infraorbital sulcus.6,7 This article describes a case of temporary paralysis of the sixth cranial nerve secondary to dental anesthesia.
Case reportA 17-year-old melanoderm female patient attended the Department of Oral and Maxillofacial Surgery, Araraquara Dental School, São Paulo State University-UNESP, Brazil for extraction of impacted third molars.
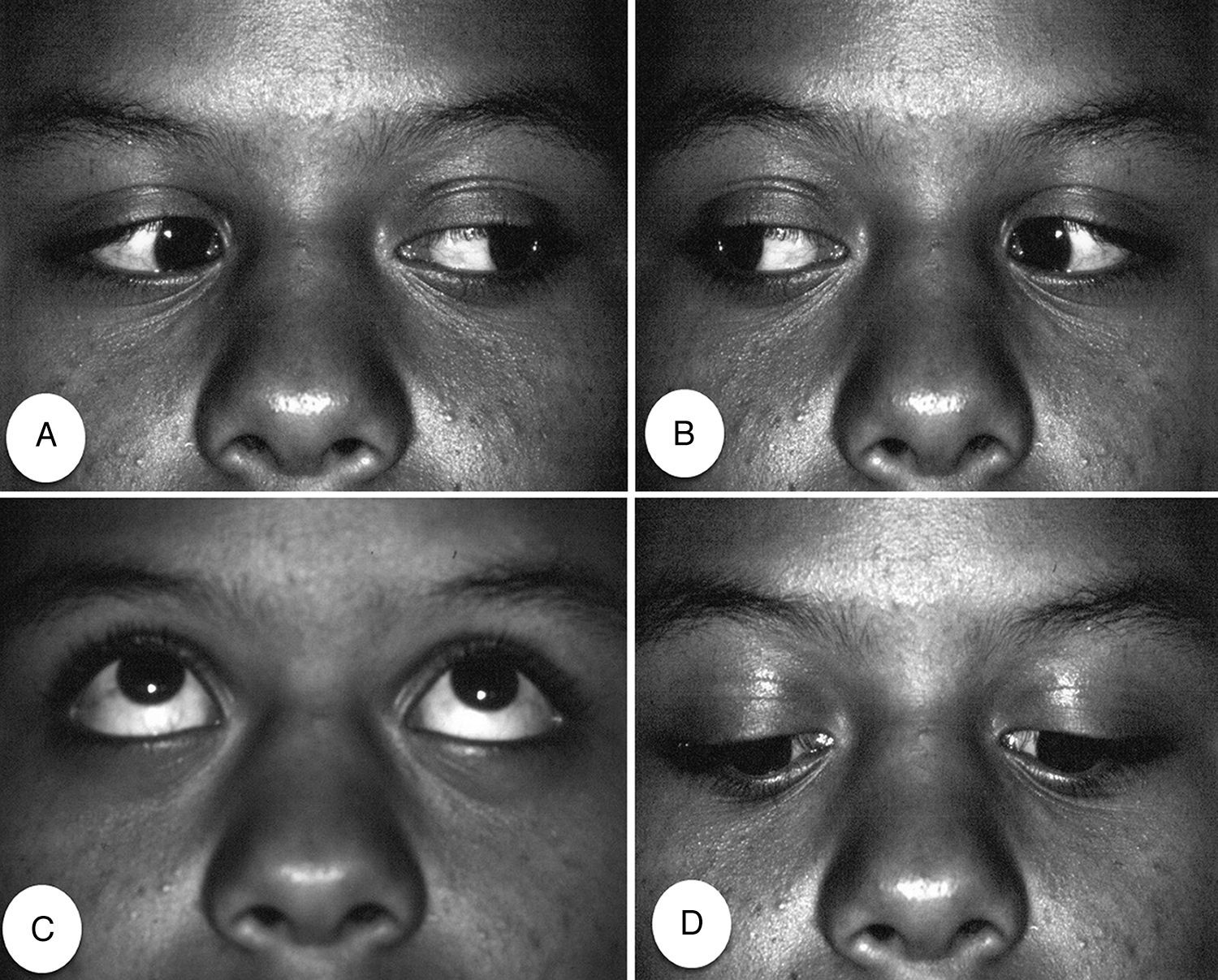
Anesthesia of the inferior alveolar, buccal, posterior superior alveolar, greater palatine, and lingual nerve was performed before extraction of elements 18 and 48. For anesthesia, 5.4mL of 2% mepivacaine solution with 1:100,000 adrenalin was used. The patient reported binocular diplopia 2min after injection of 1.8mL of anesthesia in the right mucobuccal fold in the direction of the pterygopalatine fossa. Clinical examination revealed right side paralysis of the sixth cranial nerve, apparent from absence of abduction movement of the right eye (Fig. 1).
The patient was informed about the complication, a cover was placed over the right eye, and proper instructions were given regarding the third molar extractions performed. The patient was recalled after 5 days.
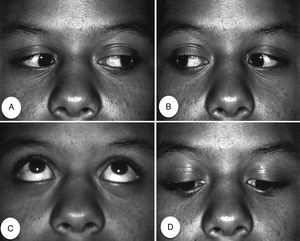
At the recall appointment, no visual or motility alteration of the involved eye was observed. The patient reported that eye movements returned to normal approximately 2h after injection of the anesthetic. Binocular diplopia and restriction of abduction of the right eye ceased, coinciding with the end of the local anesthetic effects (Fig. 2).
DiscussionOphthalmologic complications are mostly associated with intraoral local anesthesia of the inferior alveolar nerve (45.8%) or the posterior superior alveolar nerve (40.3%), i.e., injections administered in possible risk-zones.4 Prior to extracting maxillary third molars, the anesthetic solution is usually injected behind the maxillary tuberosity, close to the posterior superior alveolar nerve which emerges from the maxillary nerve before entering the maxilla through the pterygozygomatic and infratemporal fossa.5
The CNVI emerges from the brainstem between the pons and bulbar pyramid. It courses behind the anterior inferior cerebellar artery and enters the cavernous sinus, leaving the skull through the medial end of the superior orbital fissure as it enters the orbit, running on and penetrating the medial surface of the lateral rectus which abducts the eye.7
There are several hypotheses explaining paralysis of the CNVI. One such hypothesis is the denominated venous diffusion concept.1,4,8 According to this, the anesthetic solution from the pterygozygomatic and infratemporal fossa enters the pterygoid venous plexus and reaches the cavernous sinus via the emissary veins through the ovoid, lacerum, or sphenoid foraminae, affecting the CNVI and causing neuroparalysis of the lateral rectus muscle.
Since the lateral rectus muscle is only innervated by the CNVI, any kind of interruption in its function results in diplopia as the patient loses their ability to abduct the eye. Other possible hypotheses include the possibility of the anesthetic solution penetrating the orbital fossa via the maxillary sinus wall.9 The anesthetic solution may also diffuse into the ocular muscles through the inferior orbital fissure and reach the CNVI, resulting in diplopia.6 Ocular complications may also occur by simple diffusion of the anesthetic from the pterygomaxillary fossa into the orbit through defects in the bone or via the vascular, lymphatic, and venous pathways.7,10
Another possible explanation could be arterial diffusion wherein the anesthetic solution enters through the superior posterior alveolar artery that runs along a specific anomalous anatomical course, and reaches the oculomotor muscles. The solution may also enter through the superior portion of the internal maxillary artery to the middle meningeal artery, which has an anastomotic link with the lacrymal branch of the ophthalmic artery, to reach the eye muscles.9,11 In this last situation, other symptoms such as dizziness and sensitivity of the eyelids may also occur.
The most reasonable explanation for our case would be the spread of the anesthetic solution from the pterygopalatine fossa into the infratemporal fossa as it was administered with a long needle in the upper right vestibule in the direction of the pterygopalatine fossa. From the infratemporal fossa, the anesthetic solution diffused via the inferior orbital fissure into the orbit, reaching the extrinsic eye muscles and affecting the CNVI, causing partial ophthalmoplegia and resulting in binocular diplopia.1,4,7,8
In the case of ocular complications the vital signs, level of consciousness, eye movement, vision, facial muscle movement, and blanching must be evaluated to obtain a definitive diagnosis. The patient should be kept fully informed about any symptoms that may occur. In most cases, such symptoms are temporary and disappear within a short period, at which point the planned treatment can be continued.
Involvement of the CNVI may occur in any dental procedure involving anesthesia of the posterior region of the maxilla.1,3,4,7,9–11 Aspiration at the time of administration of local anesthesia is very important and minimizes the risk of ocular complications. If such complications do occur, the resulting diplopia is binocular. However, if the affected eye is covered, diplopia is not perceived by the patient. This is extremely important in order to allow the patient to be comfortable, functional, and to avoid accidents which may be caused by the double vision until the anesthetic effect subsides.
ConclusionTemporary paralysis of the CNVI is a possible complication of local anesthesia of the posterior maxilla. Care must be taken to deposit the anesthetic solution at the right location and depth using a needle of appropriate size. If this complication occurs, the patient should be reassured that the condition is temporary. Covering the affected eye is important to control diplopia until the situation resolves.
Ethical disclosuresProtection of people and animalsThe authors state that the procedures followed were in accordance with regulations established by the heads of the Clinical and Research Ethics Commission and according to the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors state that they followed the protocols of their work center on the publication of patient data.
Right to privacy and written consentThe authors declare having received written consent from patients and/or subjects mentioned in the article. The corresponding author must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.