To define a set of indicators for mental health care, monitoring quality assurance in schizophrenia, depression and bipolar disorders in Spain.
Material and methodQualitative research. Consensus-based study involving 6 psychiatrists on the steering committee and a panel of 43 psychiatrists working in several health services in Spain. An initial proposal of 44 indicators for depression, 42 for schizophrenia and 58 for bipolar disorder was elaborated after reviewing the literature. This proposal was analysed by experts using the Delphi technique. The valuation of these indicators in successive rounds allowed those with less degree of consensus to be discarded. Feasibility, sensitivity and clinical relevance were considered. The study was carried out between July 2015 and March 2016.
ResultsSeventy indicators were defined by consensus: 17 for major depression, 16 for schizophrenia, 17 for bipolar disorder and 20 common to all three pathologies. These indicators included measures related to adequacy, patient safety, exacerbation, mechanical restraint, suicidal behaviour, psychoeducation, adherence, mortality and physical health.
ConclusionsThis set of indicators allows quality monitoring in the treatment of patients with schizophrenia, depression or bipolar disorder. Mental health care authorities and professionals can use this proposal for developing a balanced scorecard adjusted to their priorities and welfare objectives.
Identificar, para el conjunto de la red asistencial en salud mental en España, un conjunto de indicadores para monitorizar la calidad asistencial en esquizofrenia, depresión mayor y trastorno bipolar.
Material y métodoEstudio basado en el consenso de especialistas en psiquiatría (6 en comité de dirección y un panel de 43 psiquiatras de la sanidad pública). Tras revisar la literatura se elaboró una propuesta inicial de 44 indicadores para depresión mayor, 42 para esquizofrenia y 58 para trastorno bipolar que, mediante estudio Delphi, fue analizada por los expertos. La valoración de estos indicadores en sucesivas rondas permitió descartar aquellos con menor grado de consenso. Se consideraron factibilidad, sensibilidad y relevancia clínica. El estudio fue realizado entre los meses de julio de 2015 y marzo de 2016.
ResultadosSe definieron por consenso 70 indicadores: 17 indicadores específicos de depresión mayor, 16 de esquizofrenia, 17 de trastorno bipolar y 20 comunes a las tres patologías. Entre estos indicadores se incluyeron medidas relativas a adecuación de los ingresos, seguridad del paciente, reagudización, contención mecánica, conducta suicida, programas psicoeducativos, adherencia terapéutica, mortalidad y salud física.
ConclusionesEste conjunto de indicadores permite monitorizar la calidad en el tratamiento de pacientes con esquizofrenia, depresión o trastorno bipolar. Cada dispositivo asistencial puede, a partir de esta propuesta, elaborar un cuadro de mando integral ajustado a sus prioridades y objetivos asistenciales.
Care quality evaluation systems have become more widespread, making it possible to compare care facilities.1 These systems include a series of indicators that offer information on the working of care facilities, according to country, for professionals as well as patients, their family members and citizens.
The use of these information systems combined with the modification of clinical practice so that it fulfils the criteria set out in practical guides, has been considered to be a means of guaranteeing the quality of care in the field of mental health2–4 and promoting structured and organised multidisciplinary treatment.5
In the case of mental illnesses, until relatively recently very few indicators were used to monitor and improve care.6 Studies have gradually been published, above all in Anglo-Saxon countries, which focus on monitoring the quality of mental health care.7,8
Two basic approaches have been used. The first of these is the monitoring of indicators in national or regional quality assurance systems. For example, Canada9 and Denmark10 have opted to design a healthcare monitoring system that includes the treatment of patients with schizophrenia. The STABLE project has set standards for good care in bipolar disorder, while other studies have used indicators to evaluate the degree to which patients are psycho-socially integrated.11 The second approach is to audit hospitals using indicators. In Holland,12 for example, a set of 6 measures to apply during an audit have been identified.
The psychiatric literature describes how quality indicators have been used to implement benchmarking systems,13 analyzing treatment equality14–17 and evaluating variability in the intensity with which certain therapies are used.18,19 The suitability of hospitalisation has been analysed20 as have referrals from primary care,21 predicting the duration of admission,22,23 supporting the implementation of routes in care,2,24 determining the degree to which psychiatric and psychosocial treatment are integrated,25 the suitability of interventions at other levels of care26,27 evaluating the effect of financing systems,28 learning about patient experience29 or evaluating the impact of physical diseases on the quality of life and mortality among mental patients30,31 or the frequency of adverse events not associated with the mental illness of these patients.32–34
The aim of this study was to identify, for the whole mental health care network in Spain, a set of indicators that will make it possible to monitor care quality in schizophrenia, major depression and bipolar disorder.
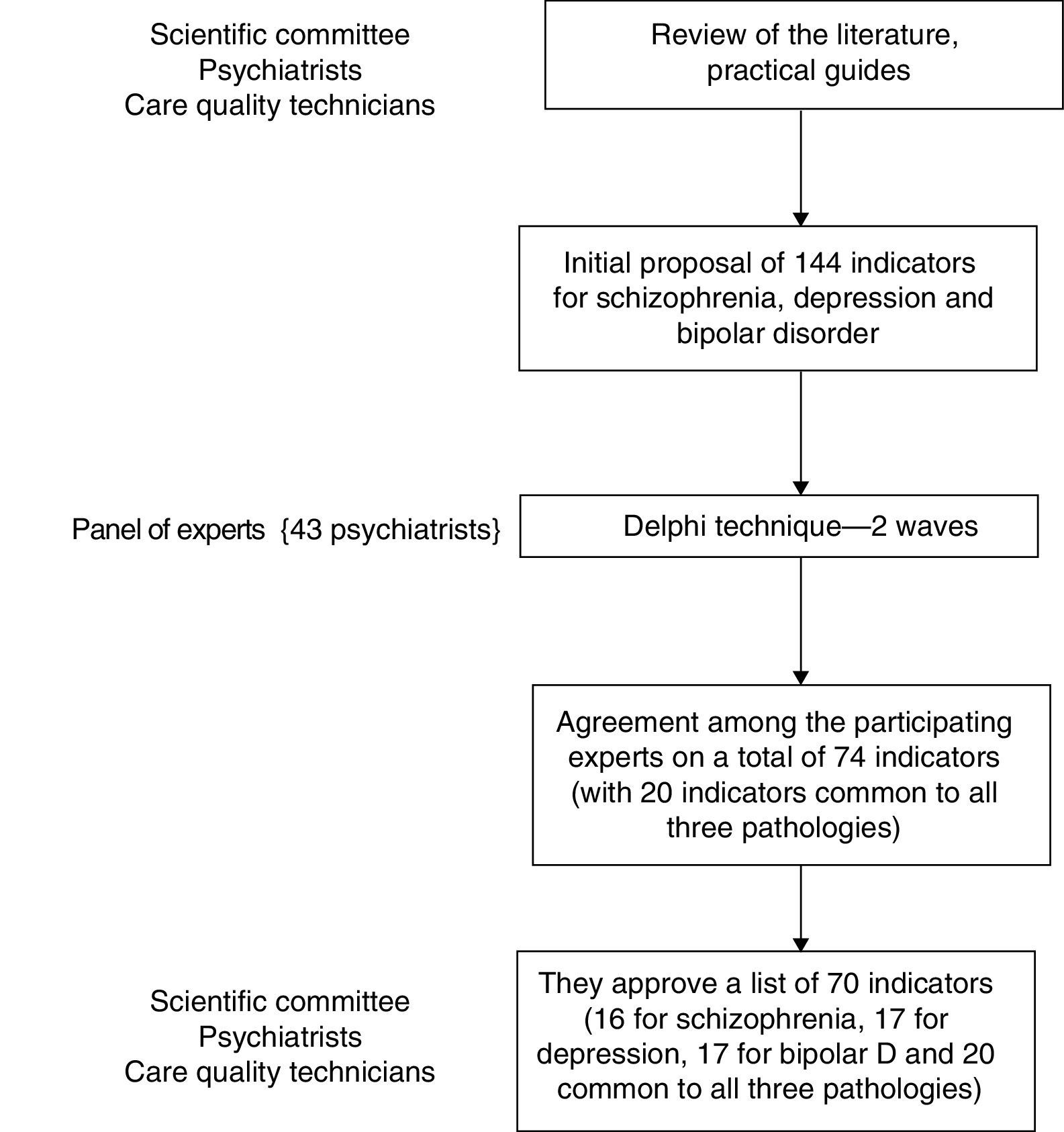
MethodThis work involved the preparation of quality indicators for schizophrenia, depression and bipolar disorder based on the consensus of a scientific committee and use of the Delphi technique among mental health specialists. The study was undertaken from July 2015 to March 2016 (Fig. 1). The scientific committee was composed of six psychiatrists with recognised prestige in the field of psychiatry who have wide experience in the pathologies analysed. It also contained three experts in care quality with more than 5 years’ experience in this field. Consultation using the Delphi technique involved a total of 43 psychiatrists in the Spanish public health system. These professionals formed three work groups, one for each of the pathologies analysed. The participation criteria for experts in this panel were at least 5 years’ experience and having played an outstanding role in clinical treatment practice and/or in research, in at least one of the three pathologies covered.
Indicator was defined in a particular way (normally numerical) for each criterion measured or evaluated; criterion was defined as the condition care had to fulfil to be considered good quality, and standard was the degree of compliance that could be demanded of a quality criterion.
As the starting point for the preparation of quality criteria, indicators and standards, the scientific committee selected and reviewed the clinical practice guides on the management of depression in adults (2014),35 bipolar disorder (2012)36 and schizophrenia and incipient psychotic disorder (2009).37 A series of studies published from 2012 to 2015 were also selected using the meta-search engines PubMed and Scopus to look for the following terms: quality indicators, quality assistance and depression, bipolar disorder and schizophrenia. The papers located in this way were reviewed, firstly by JJM and MG reading the title and abstract, independently, and secondly by reading the abstract and text of the selected references. Based on these documentary sources the scientific committee agreed a battery of potential indicators. For each one of these indicators the following aspects were determined: the quality of the evidence justifying its inclusion, reference standards based on the literature and the reliability of the sources of the information used to establish the indicator. The SIGN3 classification system was used to determine the levels of evidence and degrees of recommendation. This analysis gave rise to an initial list of indicators grouped according to pathology (major depression, schizophrenia and bipolar disorder) together with quality criteria (structure, process and result). Each set of indicators grouped according to pathology was analysed by the scientific committee, which was subdivided into workgroups with two psychiatrists per pathology. These revised their definition and organised the information on the quality of evidence, reference standards and sources of information. Subsequently, all of this information was shared in a face-to-face meeting of the whole scientific committee and the indictors that aroused the greatest doubts about their suitability were debated. Those which would have amounted to repetitions were also debated, to modify or merge them. The indicators were ranked one by one, considering their objectivity, the ease and reliability of the measurement in question in relation to the sources of information and quality of evidence. This list of indicators and their corresponding technical data sheets were reviewed once again by peers online, and then finally, in another meeting, the scientific committee evaluated the indicators once again, using a three-step scale to classify them as indispensible, moderately important or to be rejected. The resulting list of indicators was used to create questionnaire 0, which would be used during the application of the Delphi technique in the next phase of the study.
Study using the Delphi techniqueThe Delphi technique was applied using an online platform with a response scale of from 1 to 9, where 1 meant I disagree very much and 9 meant I agree very much. The indicators were presented grouped according to structure, process and result for each pathology, together with a battery of indicators that are common to all three pathologies. This phase of the research was also used to promote the diffusion of the initiative among mental health professionals in the public health system.
The Delphi technique has been used to reach agreement on measurements used to evaluate results in the field of health in many studies. It is a cost-effective technique, as it involves a large number of professionals with different experiences in a way that is simple, flexible and has appropriate control of possible distortions.38 Two successive rounds were held. Between both rounds each participant received a report on the intermediate results achieved by the panel, shown in graph format with frequency of response together with the anonymous remarks made by the group during the first round. This offered the opportunity to compare personal opinions with those of the other panellists. The consensus criterion for the participants was that agreement was considered to exist when at least one third of the participants’ scores were outside the region of the 3 points around the median. An indicator was considered to lack clinical relevance when the median was ≤3, and it was considered to be relevant when it had ≥7 points. The other indicators were considered doubtful. The top ranking indicators were selected for the next phase of the study. All of the doubtful indicators were presented in a second round to be reconsidered. The result was shared with the participants and evaluated in another meeting of the scientific committee.
The second round included a ranking and selection of the indicators considered to be essential in psychiatric clinical practice for the pathologies of major depression, schizophrenia and bipolar disorder. The justification for this modification was that, due to the fact that the questionnaire included items that were mainly drawn from evidence that was scientifically validated in the bibliography, the expected level of consensus was high in the majority of cases. However, it was necessary to identify the ones that were essential and which would make it possible to ensure identification of minimum quality standards in clinical practice. Compliance with the main aim of the project was therefore emphasised and ensured: to define by consensus a minimum number of indicators for the suitable management of major depression, schizophrenia and bipolar disorder, to be used in the Spanish healthcare system.
After each round the degree of dispersion of the final replies was statistically analysed to determine which questions had attained a sufficient degree of agreement among the experts, in terms of their agreement or disagreement with each indicator. The indicators that did not attain the specified level of agreement or which were not identified as priorities by the panel of experts, but which were considered to be recommendable by the scientific committee, are listed in the additional material (Appendix A).
Definition of criteria, indicators and standardsThe selected indicators were grouped by the scientific committee according to the similarity of the quality criteria they represented. A file was prepared for each indicator containing the following fields: denomination of the criterion, definition, calculation formula, justification, exclusions or clarifications, indicator type (structure, process or result), source/s of information, objective or acceptable level and bibliography of the reference standard, depending on the data supplied in the scientific literature. These files were revised and validated by two professionals with experience in care quality and, more specifically, in the design of quality indicators to implement benchmarking strategies. They were finally reviewed by the members of the scientific committee.
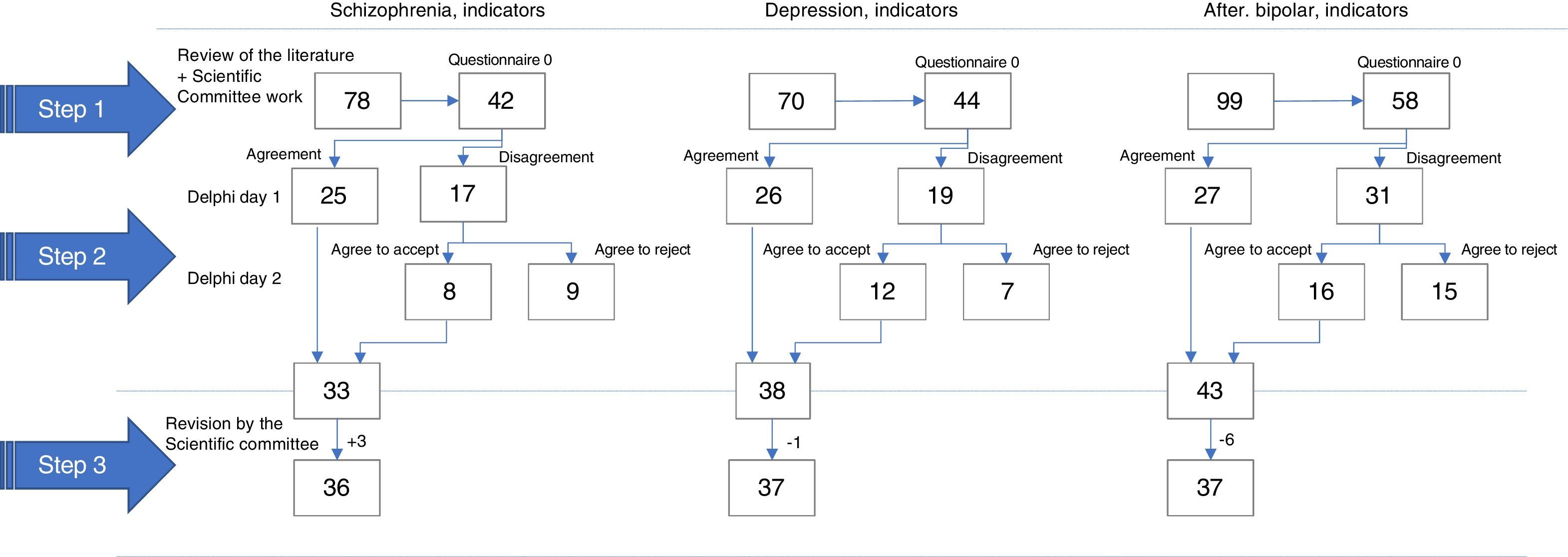
ResultsThe review of documents identified 14 scientific references supplied by the review of the bibliography, including originals of systematic reviews of highly effective treatments for the pathologies in question which contained measurements for the evaluation of the clinical result. The scientific committee identified an initial list of 247 potential indicators: 70 for major depression in adults, 78 indicators for schizophrenia and incipient psychotic disorder and 99 indicators for bipolar disorder. After reviewing similarities, pertinence and clarity, and taking into account the criteria of objectivity, ease of measurement and auditability, questionnaire 0 for the first round of the Delphi study had 44 possible indicators for major depression, 42 for schizophrenia and 58 for bipolar disorder.
All of the 43 panellists responded in the first and second rounds of the Delphi technique. There were 14 panellists expert in the study and treatment of major depression, 9 panellists expert in the study and treatment of schizophrenia and 20 panellists expert in the study and treatment of bipolar disorder. In the first round consensus was reached on 26 indicators for major depression, 25 for schizophrenia and 27 for bipolar disorder; 19 were considered doubtful for major depression, 17 for schizophrenia and 31 for bipolar disorder. In the second round and following review, consensus was reached for the suitability of 12 indicators for major depression, 8 for schizophrenia and 16 for bipolar disorder. 7 were rejected for major depression, 9 for schizophrenia and 15 for bipolar disorder. Lastly, the resulting set of indicators was subjected to judgement by the scientific committee. To unify the quality criteria examined this committee included 3 indicators in the case of the table of the list of indicators for schizophrenia and eliminated one in the case of depressive disorder and 6 from the list of bipolar disorder indicators. In this way a total 70 indicators were defined: 17 specific indicators for major depression, 16 specific indicators for schizophrenia, 17 specific indicators for bipolar disorder and 20 indicators that are common to all three pathologies (Fig. 2).
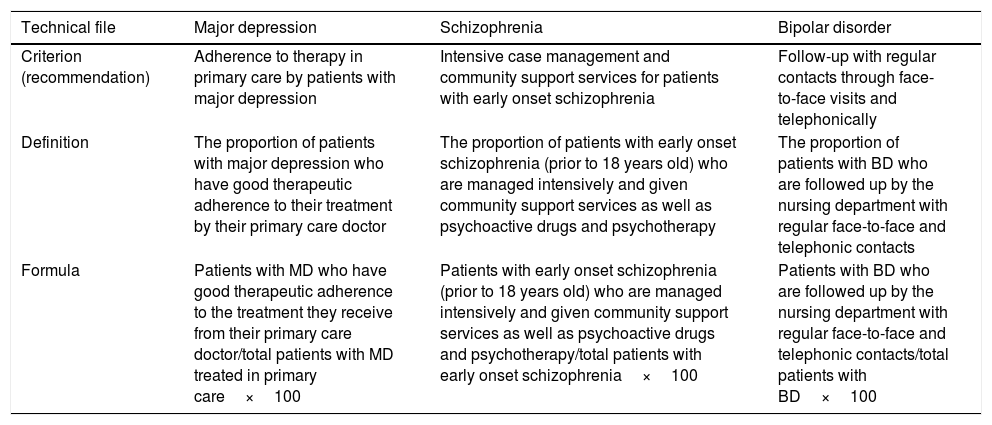
The indicators common to all three pathologies included measures relating to the suitability of admission, patient safety, relapse, mechanical restraint, suicidal behaviour, psycho-educational programs, adherence to therapy and mortality or physical health. Although the indicators of results in the whole set were given precedence, there were slightly more process indicators than there were result indicators. Table 1 describes three examples of descriptive files of the agreed indicators. For each one its operational definition was established, together with the calculation formula to prevent variability in the estimation of the indicator, whether it was an indicator of structure, process or result, the justification for recommending this indicator, and clarification on the correct interpretation of the indicator, the evidence that supports the propagation of the indicator, its definition and calculation formula together with the sources of information and references used. In all cases the calculation formula also establishes the recommendable periodicity of the measurement. Table 1 online shows all of the specific indicators identified for each pathology, grouped according to quality criteria and including their operational definition. For example, in the case of major depression, the following indicator was included in the process indicators for evaluation and diagnosis: the proportion of patients with major depression (MD), in the evaluation of which the following aspects were taken into account: the characteristics of the episode, psychosocial aspects, associated degree of dysfunction and/or disability, the aspects that had the greatest functional impact in the everyday life of the patient and the heterogeneity of the disorder and how the patient perceived himself and his symptoms. Table 2 online shows the indicators common to all three pathologies with their corresponding quality criterion details to facilitate comprehension, as well as their operational definition. For example, respecting the results indicators and the suitability criterion for admission to hospital, the indicator for the appropriateness of admission common to all three pathologies has been defined as: patients with MD-SCH-BD treated in the acute unit who fulfil the admission criteria. The files for each indicator with all of their information may be consulted as complementary information in the digital version of this paper.
Examples of the descriptive files of indicators.
| Technical file | Major depression | Schizophrenia | Bipolar disorder |
|---|---|---|---|
| Criterion (recommendation) | Adherence to therapy in primary care by patients with major depression | Intensive case management and community support services for patients with early onset schizophrenia | Follow-up with regular contacts through face-to-face visits and telephonically |
| Definition | The proportion of patients with major depression who have good therapeutic adherence to their treatment by their primary care doctor | The proportion of patients with early onset schizophrenia (prior to 18 years old) who are managed intensively and given community support services as well as psychoactive drugs and psychotherapy | The proportion of patients with BD who are followed up by the nursing department with regular face-to-face and telephonic contacts |
| Formula | Patients with MD who have good therapeutic adherence to the treatment they receive from their primary care doctor/total patients with MD treated in primary care×100 | Patients with early onset schizophrenia (prior to 18 years old) who are managed intensively and given community support services as well as psychoactive drugs and psychotherapy/total patients with early onset schizophrenia×100 | Patients with BD who are followed up by the nursing department with regular face-to-face and telephonic contacts/total patients with BD×100 |
| Type | Result | Process | Process |
|---|---|---|---|
| Justification/Exclusions/Clarifications | In primary care the rate of non-adherence to anti-depressive treatment is high (approximately 50%) from the first weeks after starting it. Some factors that explain this lack of adherence to pharmacological treatment are the presence of side effects and the absence of the desired effect, or the long time until response to treatments | Intensive management is recommended of cases, with community support services as well as the administration of psychoactive drugs and psychotherapy for patients with early onset schizophrenia (before 18 years old) | Follow-up must involve regular contacts in the nursing surgery and it is also advisable to support follow-up through telephonic consultation |
| Strength of the recommendation | D. Evidence level 3 or 4. Evidence extrapolated from level 2+ studies | D. Evidence level 3 or 4. Evidence extrapolated from level 2+ studies | C. Sufficient evidence derived from 2+ level studies, directly applicable to the target population and showing overall consistency in the results. Evidence extrapolated from 2++ level studies |
| Information sources | Clinical documentation | Clinical documentation | Clinical documentation |
| References | • Calderón C, Retolaza A, Payo J, Bacigalupe A, Zallo E, Mosquera I. Perspectivas de los pacientes diagnosticados de depresión y atendidos por médicos de familia y psiquiatras. Aten Primaria. 2012;44(10):595–602. • Grupo de Trabajo de la Guía de Práctica Clínica sobre la Depresión Mayor en la Infancia y en la Adolescencia. Guía de Práctica Clínica sobre la Depresión Mayor en la Infancia y en la Adolescencia. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad y Política Social. Axencia de Avaliación de Tecnoloxías Sanitarias de Galicia (avalia-t); 2009. Guías de Práctica Clínica en el SNS: avalia-t N° 2007/09. • Párraga-Martínez I, López-Torres Hidalgo J, del Campo del Campo JM, Villena Ferrer A, Morena Rayo S, Escobar Rabadán F. Seguimiento de la adherencia al tratamiento antidepresivo en pacientes que inician su consumo. Aten Prim. 2014;46:357–66. • Roca M, Armengol S, Salvador-Carulla L, Monzón S, Salvà J, Gili M. Adherence to medication in depressive patients. J Clin Psychopharmacol. 2011;31(4):541–3 | • Dixon LB, Goldman HH, Bennett ME, et al. Implementing coordinated specialty care for early psychosis: The raise connection program. Psychiatr Serv. 2015;66(7):691–8 • Grupo de Trabajo de la Guía de Práctica Clínica sobre la Esquizofrenia y el Trastorno Psicótico Incipiente. Fòrum de Salut Mental, coordinación. Guía de Práctica Clínica sobre la Esquizofrenia y el Trastorno Psicótico Incipiente. Madrid: Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad y Consumo. Agència d’Avaluació de Tecnologia i Recerca Mèdiques; 2009. Guía de Práctica Clínica: AATRM. N° 2006/05-2. • Insel TR. RAISE-ing Our Expectations for First-Episode Psychosis. Am J Psychiatry. 2016;173:311–2. • Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173:362–72. • Ojeda N, Peña J, Segarra R, et al. La predicción del diagnóstico de esquizofrenia: El rol de la neurocognición en el primer episodio de psicosis. Bilbao: Editorial Universidad | Grupo de Trabajo de la Guía de Práctica Clínica sobre Trastorno Bipolar. Guía de Práctica Clínica sobre Trastorno Bipolar. Madrid: Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Servicios Sociales e Igualdad. Universidad de Alcalá. Asociación Española de Neuropsiquiatría. 2012. UAH/AEN Núm. 2012/1 |
A set of indicators are presented that make it possible to monitor the quality of treatment of patients with schizophrenia, depression or bipolar disorder. This catalogue of indicators has been prepared while attempting to ensure that they are acceptable for professionals and healthcare management, that they are sensitive enough to detect changes when introducing good care practices, that they can be calculated using current information systems and that they are valid, i.e., that they are clinically relevant. The methodology used followed the guidelines used in other indicator-based monitoring systems.39,40
There are fewer indicator-based quality monitoring systems for mental illnesses than is the case for other pathologies.41 This lack makes it harder to evaluate the quality of psychiatric care. This proposal of indicators is designed to ensure that there is an environment in Spain that makes it possible to assure and improve the quality of psychiatric care for this patient profile by supplying process and results indicators that meet European recommendations.41 In this way mental health units will be able fulfil the quality improvement standards implemented in other countries.42–44
Unlike other approaches which centre on the overall working of mental health protection systems,45 this catalogue of indicators makes it possible to monitor quality in three disabling and highly prevalent pathologies in terms of acceptability, accessibility, pertinence, competence, continuity, efficacy, efficiency and safety.
Around 17 indicators are selected for each scenario. This proposal is similar in its approach and type of indicators included to those of other studies in the case of bipolar disorder,46 depression47 and schizophrenia.43,48–50 This set of indicators is designed for the implementation of a benchmarking system, although it may also be used to audit mental health departments or as the basis for developing a quality certification system.
Putting this proposal into practice is based on the voluntary participation of community and hospital mental health units. This list of indicators makes it possible to adapt to the priorities of each one of these units, defining its entire control panel on the basis of them.
LimitationsThe level of evidence of mental health quality indicators identified in the literature varies, and this is so for all of the studies. We have tried to overcome this potential limitation by using a panel of experts. As well as their clinical relevance, the feasibility of calculation and acceptability of indicators have been taken into account, so that although other equally valid indicators may exist, they have not been included in this list. This proposal is designed to be applied from the first moment by mental health departments, so that in the future other quality indicators may be included, or some may be replaced due to technical or therapeutic advances. This list does not include quality indicators associated with the Patient Reported Outcome Measures.51 The preparation of indicators in psychiatry is a complex matter. This is so firstly because it is hard to determine the efficacy of an intervention over the short term. Secondly, the scope of the concept of quality requires a large number of indicators to explore different dimensions. Thirdly, technologies change and new treatments emerge constantly and quickly. Fourthly, the multidisciplinary nature of clinical interventions makes it more complex. The panel of experts was composed of clinicians with a long and recognised professional history, assisted by professionals in the field of care quality with more than 15 years’ experience. Nevertheless, future studies will be able to include other types of professional, such as healthcare managers or private healthcare company managers. Patients may also be included to check the acceptability of the proposed indicators.
The quality of care is now a priority interest for clinicians, patients, managers, regulatory bodies and society in general. The main strength of this project is its pioneering nature in Spain, as a response to the desire to ensure and improve the quality of care in mental illnesses. This study promotes a suitable environment so that patients have a proven level of quality in all areas of the healthcare system.
To conclude, we present a set of result and process indicators drawn up by consensus, similar to other European works in recent years. It seeks to improve the quality of treatments received by patients with depression, bipolar disorder or schizophrenia. These indicators centre on aspects relating to accessibility, diagnostic accuracy, treatment and safety. Measurements of this type make it possible to establish targets for care and to compare units, hospitals and healthcare areas.
FinancingThis study was financed by a Jansen-Cilag Educational Grant.
Conflict of interestsMiquel Bernardo has been a consultant or has received fees or research funding from AB-Biotics, Adamed, Amgen, Boehringer, Eli Lilly, Ferrer, Forum Pharmaceuticals, Gedeon, Janssen-Cilag, Lundbeck, Pfizer, Roche, CIBERSAM, Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación, Ministerio Economía y Competitividad, Generalitat de Catalunya, Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2014SGR441), the 7th Framework Program of the European Union y Foundation Group for Research in Schizophrenia (EGRIS).
Consuelo de Dios has received fees for advisory, teaching or research activities from Janssen, Lundbeck, Otsuka, Pfizer and Servier. She has received grants from the Instituto de Investigación Carlos II and the Instituto de Investigación IDIPAZ.
Víctor Pérez has been a consultant or has received fees or research funding from AB-Biotics, AstraZeneca, Bristol-Myers-Squibb, CIBERSAM, FIS- ISCiii, Janssen Cilag, Lundbeck, Otsuka, Servier and Medtronic.
Emilio Ignacio has been a speaker and consultant with Janssen-Cilag. A consultant of Abbvie España, Allergan and Boehringer.
Manuel Serrano declares that during the year 2016 – 2017 he obtained financing for meetings, conferences and attending courses from Otsuka, Janssen, Lundbeck, financing for taking part in research from Janssen, fees as a speaker (conferences and courses from Otsuka, Janssen and Lundbeck) and as a consultant for a Janssen pharmaceutical company in new technologies.
Eduard Vieta has received financing for research projects and/or fees as a consultant or speaker from the following companies and institutions: AB-Biotics, Allergan, Angellini, AstraZeneca, Bristol-Myers Squibb, Elan, Eli Lilly, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, Glaxo-Smith-Kline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, Sanofi-Aventis, Servier, Shire, Solvay, Sunovion, Takeda, el Instituto de Salud Carlos III, el Séptimo Programa Marco (ENBREC), the Brain and Behaviour Foundation (NARSAD) and the Stanley Medical Research Institute.
José Joaquín Mira has been a consultant for Janssen Cilag and MSD España, with whom he is currently collaborating in several research projects. He is an Almirall speaker.
Mercedes Guilabert has been a consultant for Janssen Cilag and MSD España, with whom she currently works on several research projects.
Miquel Roca has received Research grants from the Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, European Union ERDF and fees for his participation in Boards (Janssen, Lundbeck) and in Continuous Medical Education (Janssen, Lundbeck, Pfizer).
The authors would like to thank the Unidad de Investigación Estratégica en Salud de Luzán 5 for methodological and technical support.
The CERCA Programme/Generalitat de Catalunya, Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2014SGR441).
Please cite this article as: Bernardo M, de Dios C, Pérez V, Ignacio E, Serrano M, Vieta E, et al. Indicadores de calidad en el tratamiento de pacientes con depresión, trastorno bipolar o esquizofrenia. Estudio de consenso. Rev Psiquiatr Salud Ment (Barc.). 2018;11:66–75.