Over the past 25 years, several studies have shown the efficacy of a number of psychological interventions for severe personality disorders. However, the generalizability of these positive results from long traditional research settings to more ordinary ones has been questioned, requiring a need for replication in pragmatic studies.
MethodsThis pragmatic study compares hospitalizations and Emergency Room visits before and during a 6-month therapeutic programme for severe personality disorders, and at 36 months after starting it. The therapeutic programme, which integrates several specific interventions within a coherent framework, was carried out in an ordinary clinical setting. Fifty-one patients, evaluated according DSM-IV criteria by using the Spanish version of the Structured Clinical Interview for Personality Disorders (SCID-II), were included.
ResultsThe clinical characteristics showed a group of severely disturbed patients, of which 78.4% met criteria for borderline personality disorder. The percentage of patients hospitalized and visiting the Emergency Room, as well as the number of days of hospitalisation and Emergency Room visits was significantly reduced during the treatment, and this improvement was maintained throughout.
ConclusionsAn integrated treatment for severe personality disorders could be effective in preventing reliance on readmissions, or prolonged hospital stays, when it is implemented by clinicians in ordinary clinical settings.
En los últimos 25 años varios estudios han mostrado la eficacia de diversas intervenciones psicológicas para los trastornos graves de la personalidad. Sin embargo, la generalización de estos resultados positivos desde entornos con larga tradición investigadora a condiciones de práctica habitual ha sido cuestionada, reclamándose la replicación en estudios pragmáticos.
MétodosEste estudio pragmático compara las hospitalizaciones y las visitas a Urgencias antes y durante un programa terapéutico de 6 meses para trastornos graves de la personalidad y 36 meses después del inicio. El programa terapéutico, que integra varias intervenciones específicas en un encuadre coherente, se realizó en un entorno de práctica habitual. Se incluyeron 51 pacientes evaluados de acuerdo con criterios DSM-IV por medio de la versión española de la Entrevista Clínica Estructurada para Trastornos de la Personalidad (SCID-II).
ResultadosLas características clínicas evidenciaron un grupo de pacientes muy graves, de los que el 78,4% cumplía criterios de trastorno límite de la personalidad. El porcentaje de pacientes hospitalizados y que visitaron Urgencias, así como el número de días de hospitalización y de visitas a Urgencias, se redujo significativamente durante el tratamiento, y esta mejoría se mantuvo en el tiempo.
ConclusionesUn tratamiento integrado para trastornos graves de la personalidad puede ser efectivo para reducir las readmisiones o las estancias hospitalarias prolongadas cuando es implementado por clínicos en condiciones de práctica habitual.
People who suffer from personality disorders (PD) in general, and borderline personality disorder (BPD) in particular, frequently show a serious psychopathology along with poor psychosocial functioning and quality of life.1–3 For many years, the uncertain effectiveness of treatments available for PDs even made some physicians question the feasibility of treating these patients in the public health services.4,5 In the last 25 years, several prospective studies have shown the usefulness of different psychotherapeutic interventions in PD6,7 in outpatient treatment,4,8–20 day hospital (DH) programmes1,21–26 or inpatient programmes.27,28
Despite all these advances, there are still many questions in relation to PD treatment. Some authors24 wonder if the efficacy achieved in therapeutic programmes at university hospitals with a high level of clinical expertise and research is applicable to sites that usually treat PD and carry out studies under the conditions of routine practise.5,7,24 Furthermore, since PD represent a very heterogeneous group of patients24 and none of the treatments is supported by solid evidence,7 several expert reviews29,30 have recommended integrated treatment for PD combining effective interventions taken from different therapeutic models and applying them in a structured manner according to a protocol. However, the evidence available for this approach is limited.1,14
Another essential issue is treatment duration.20,24,31 Most therapies being researched last for at least for one year, which ultimately leads to long waiting lists. Some authors2,31 state that most PD do not require such long therapies, which should be reserved for more serious patients. Finally, given the fact that many PDs show a chronic course, it is worth wondering if the benefits obtained in the different therapies persist over the years. Information related to the topic is scarce, since only a few studies have follow-up periods for more than two years, either in outpatient treatments,4,14,20,32 inpatient programmes33 or DH programmes.21,34
In our field, PD account for more than one-third of short-term readmissions35 (within 90 days after discharge) and the quality of health care continuance was low.36 With a view to improving health care provided to these patients, an integrated therapeutic programme was launched which, despite taking advantage of the DH resources, offered specific treatment within a customised health care environment.
The objectives of this study are the following: (a) to assess programme effectiveness to reduce repeated and/or extended hospitalisations and recurrent Emergency Room visits; and (b) to determine if this benefit is maintained in the mid-long term during the three-year follow-up.
Material and methodsStudy and designThis is a pre–post, intrasubject, pragmatic study of patients admitted to an integrated therapeutic programme for PD with serious psychiatric symptomatology and low psychosocial functioning (severe personality disorders, SPD). It was conducted at a DH belonging to the mental health network that provides services to a population of about 299,000 inhabitants within the Barcelonès-Nord health care area in the metropolitan area of Barcelona. The private practise of the area is scarce and milited to the outpatient setting; according to the guidelines of the health authorities, medical-psychiatric health care is sectorised and patients should be referred to hospitals responsible for this health care area. Therefore, almost all subjects with mental health disorders are treated at these sectorial hospitals. A biannual assessment was used, including upon admission to the programme (T-0) and after 6 months (T-1), 12 months (T-2), 18 months (T-3), 24 months (T-4), 30 months (T-5) and 36 months (T-6). The study was approved by the local Ethics Committee, and all patients signed an Informed Consent Form.
Participants and procedureThe patient sample was selected out of all consecutive referrals to the SPD programme from September 2001 to December 2006 (n=66). The inclusion criteria for the programme were the following: (a) DSM-IV criteria37 for BPD; (b) if the BPD criteria were not met, then the DSM-IV criteria37 for another PD were used along with self-inflicted lesions, suicidal behaviour or impulsive behaviour in at least two fields (expenses, sex, substance abuse, careless driving, food binges) of the fourth criteria of BPD according to the DSM-IV37; (c) a score of 50 or less in the Global Assessment of Functioning (GAF) Scale of the DSM-IV37; and (d) treatment could be initiated without having to take a leave from studies or work. The exclusion criteria implied meeting the DSM-IV37 criteria for: (a) schizophrenia; (b) bipolar disorder I; (c) mental retardation; and (d) substance abuse disorder, in this case, only if there were behavioural disorders which interfered with treatment. All patients were assessed by a referral therapist, who had been consecutively appointed, by means of a clinical interview in accordance with the DSM-IV criteria.37 The assessment protocol included a sociodemographic survey, the GAF Scale of the DSM-IV37 and the Spanish version of the semi-structured interview for making Axis II38 (SCID-II). Two patients were excluded because they met the schizophrenia criteria, and another patient met bipolar disorder I criteria. In 12 out of the 63 remaining cases, in the 7 patients who had been admitted in 2001 and half of those who had been admitted in 2002, it was not possible to administer the SCID-II due to problems related to the launch of the programme. Thus, our final sample included 51 patients diagnosed with PD. Sixteen patients (31.4%) abandoned the programme (12 patients, 23.5%, during the first 4 months); all of these patients were included in the analysis. During the treatment period, one patient died as a result of self-inflicted lesions, and 17 months after having finished treatment one patient committed suicide; in both cases, the last observations were carried forward.
Intervention: the integrated therapeutic programme for severe personality disordersThe SPD programme is a multiple-component, integrated treatment that adopts the four general therapeutic strategies suggested by Livesley39 as organisational general framework and combines effective techniques from different therapeutic models. The programme offers a 6-month treatment for male and female subjects aged 18–55 years. All patients show a PD, most of them a BPD, with low general functioning and serious behavioural disorders, especially suicidal behaviour and self-inflicted lesions. Before and after discharge, patients receive standard psychiatric treatment. After a complete description of the programme, all patients and the referral therapist, on behalf of the team, sign a therapeutic agreement that entails some minimal commitments for both parties. The programme, which takes place from Monday to Friday, comprises several weekly group interventions: (a) skill training group (2.5h), based on dialectic behaviour therapy40 (DBT); (b) relationship therapy (1.5h), supported by mentalisation-based treatment41 (MBT); (c) stress management group (2h); and (d) psychoeducational group (1.5h). Moreover, it includes: (e) individual therapy once a week, support psychodynamic psychotherapy42 or DBT,42 depending on the therapist's approach. In addition, as frequently as needed by each patient, there are also: (f) medication review; (g) nursing consultation; and (h) telephone consultation (from Monday to Friday, from 9:00 a.m. to 4:00 p.m.). Group psychotherapy is conducted in co-therapy by nursing staff and/or psychotherapists. Individual psychotherapy is conducted by a team of 4 psychotherapists with more than 10 years of training and vast psychotherapeutic experience at public hospitals. Once a week, the whole team holds a supervisory meeting (1.5h).
Outcome variables and information sourcesThe main outcome variable was the need for hospitalisation, assessed as a dichotomous variable (either present or absent) and as a recount variable (number of admissions) in each period. Other outcome variables were hospitalisation duration (number of days) and psychiatric emergency, also assessed as a dichotomous variable (either present or absent) and as a recount variable (number of emergencies). Assessments were made before admission to the programme or during baseline assessment (T0, including the 6 months prior to treatment start), after 6 months of treatment (T1) and every 6 months until completing the 36-month follow-up (T2, including months 7–12 from treatment start; T3, months 13–18; T4, months 19–24; T5, months 25–30; T6, months 31–36). During treatment, patients were asked about the use of services. In addition, an individual search was made with the hospital database in order to obtain information about hospitalisations and Emergency Room visits before treatment, during treatment and throughout the follow-up period. Data were verified against the notes included in the medical record and hospital health care professionals who treated patients during follow-up were questioned.
Statistical analysisThe statistical analysis was performed by means of the statistical programme SPSS® version 21.0. Account and continuous variables were described by means of the mean and standard deviation (SD), and categorical variables, by means of the absolute frequency and percentage. All outcome variables were analysed by an intention-to-treat analysis. For the analysis of the change throughout the follow-up, the procedure of generalised estimating equations was used, which goes beyond the generalised linear model for the analysis of repeated measures. The generalised estimating equations take into account that the same patients are measured repeatedly and use all the available data, notwithstanding the number of repeated measures.43 For the analysis, an exchangeable correlation structure was employed, which assumes that the correlation between consecutive measures is the same, regardless of the time between measures. For each outcome variable, a generalised estimating equations analysis was performed, where the dependent variable was the corresponding outcome measure (either dichotomous, recount or continuous), while the six dummy variables which were created to indicate time were used as an independent variable. Baseline assessment was used as a reference category. The regression coefficient (B), together with the standard error and the 95% confidence interval of each dummy variable, was used to estimate the effect of treatment between baseline assessment (T0) and follow-up (T1–T6). In order to quantify the difference between the means of continuous outcome variables, the effect size was calculated as the difference between the baseline mean and the last mean (T6), divided by the baseline SD.44 Values of p<0.05 were considered significant.
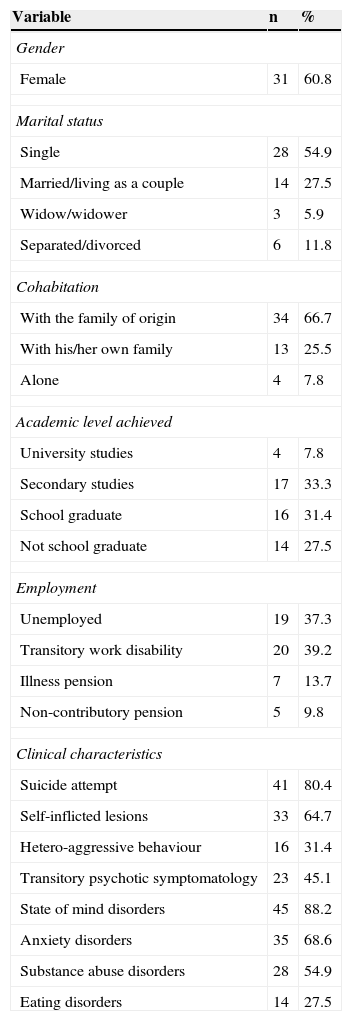
ResultsSample descriptionDuring baseline assessment, patients had a mean age of 33.4 years (SD=9.2), 31 (60.8%) were female subjects, the level of education achieved was low (59% did not have any secondary studies), and 100% did not work or study (Table 1). As regards the PD diagnosis based on Axis II, 40 (78.4%) patients met the BPD criteria, 3 (5.9%) met the unspecified PD criteria, 2 (3.9%) met the PD due to dependence criteria, 2 (3.9%) met the paranoid personality disorder criteria, 2 (3.9%) met the schizotypal personality disorder criteria, one (2.0%) met the narcissistic personality disorder criteria and another (2.0%) met the PD due to avoidance criteria. In addition, it was a sample with a serious symptomatology, as reflected by the clinical characteristics shown in Table 1, and low general functioning: mean score according to the GAF Scale of 39.3 (SD=4.4).
Clinical and sociodemographic variables.
| Variable | n | % |
|---|---|---|
| Gender | ||
| Female | 31 | 60.8 |
| Marital status | ||
| Single | 28 | 54.9 |
| Married/living as a couple | 14 | 27.5 |
| Widow/widower | 3 | 5.9 |
| Separated/divorced | 6 | 11.8 |
| Cohabitation | ||
| With the family of origin | 34 | 66.7 |
| With his/her own family | 13 | 25.5 |
| Alone | 4 | 7.8 |
| Academic level achieved | ||
| University studies | 4 | 7.8 |
| Secondary studies | 17 | 33.3 |
| School graduate | 16 | 31.4 |
| Not school graduate | 14 | 27.5 |
| Employment | ||
| Unemployed | 19 | 37.3 |
| Transitory work disability | 20 | 39.2 |
| Illness pension | 7 | 13.7 |
| Non-contributory pension | 5 | 9.8 |
| Clinical characteristics | ||
| Suicide attempt | 41 | 80.4 |
| Self-inflicted lesions | 33 | 64.7 |
| Hetero-aggressive behaviour | 16 | 31.4 |
| Transitory psychotic symptomatology | 23 | 45.1 |
| State of mind disorders | 45 | 88.2 |
| Anxiety disorders | 35 | 68.6 |
| Substance abuse disorders | 28 | 54.9 |
| Eating disorders | 14 | 27.5 |
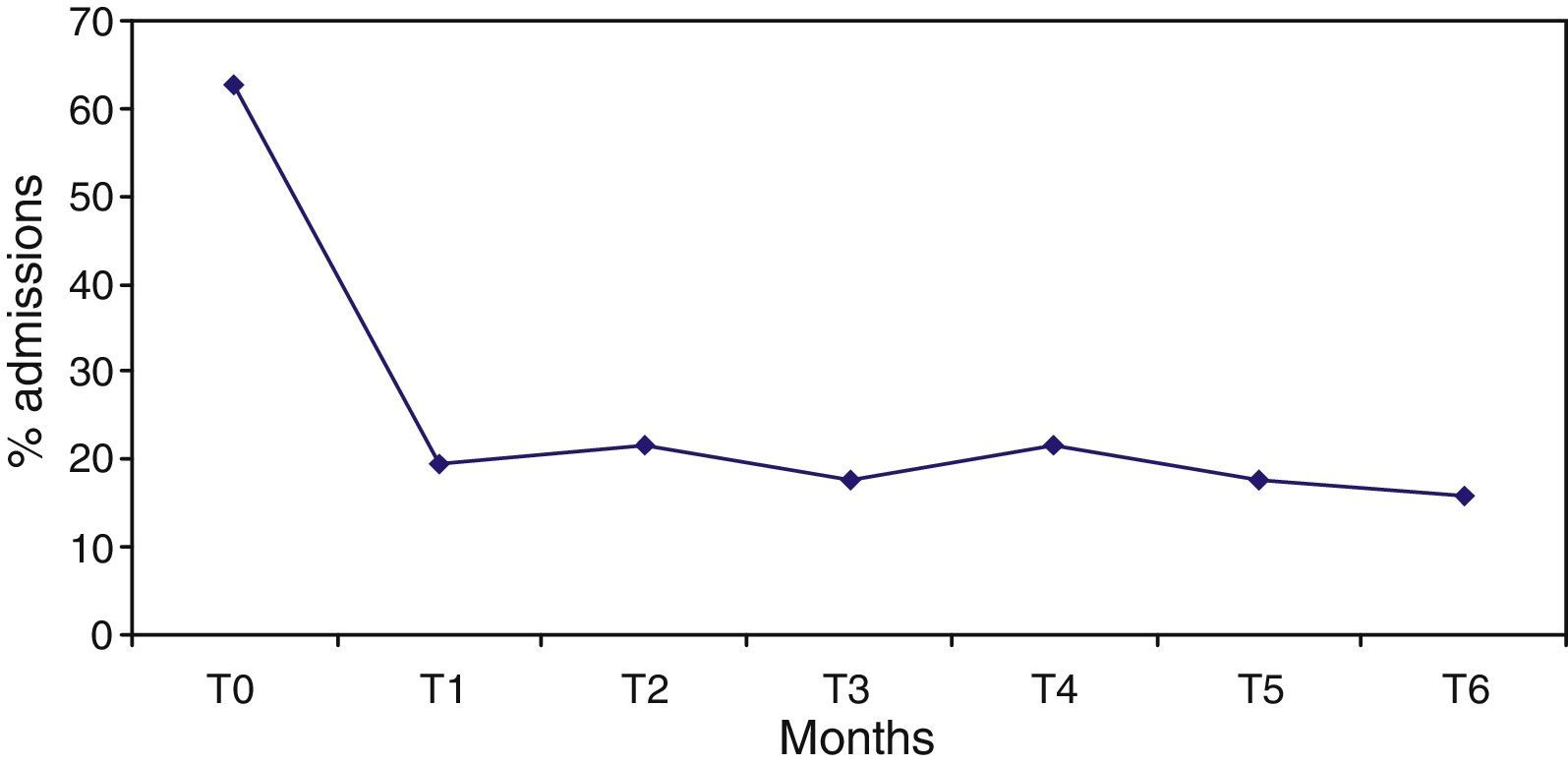
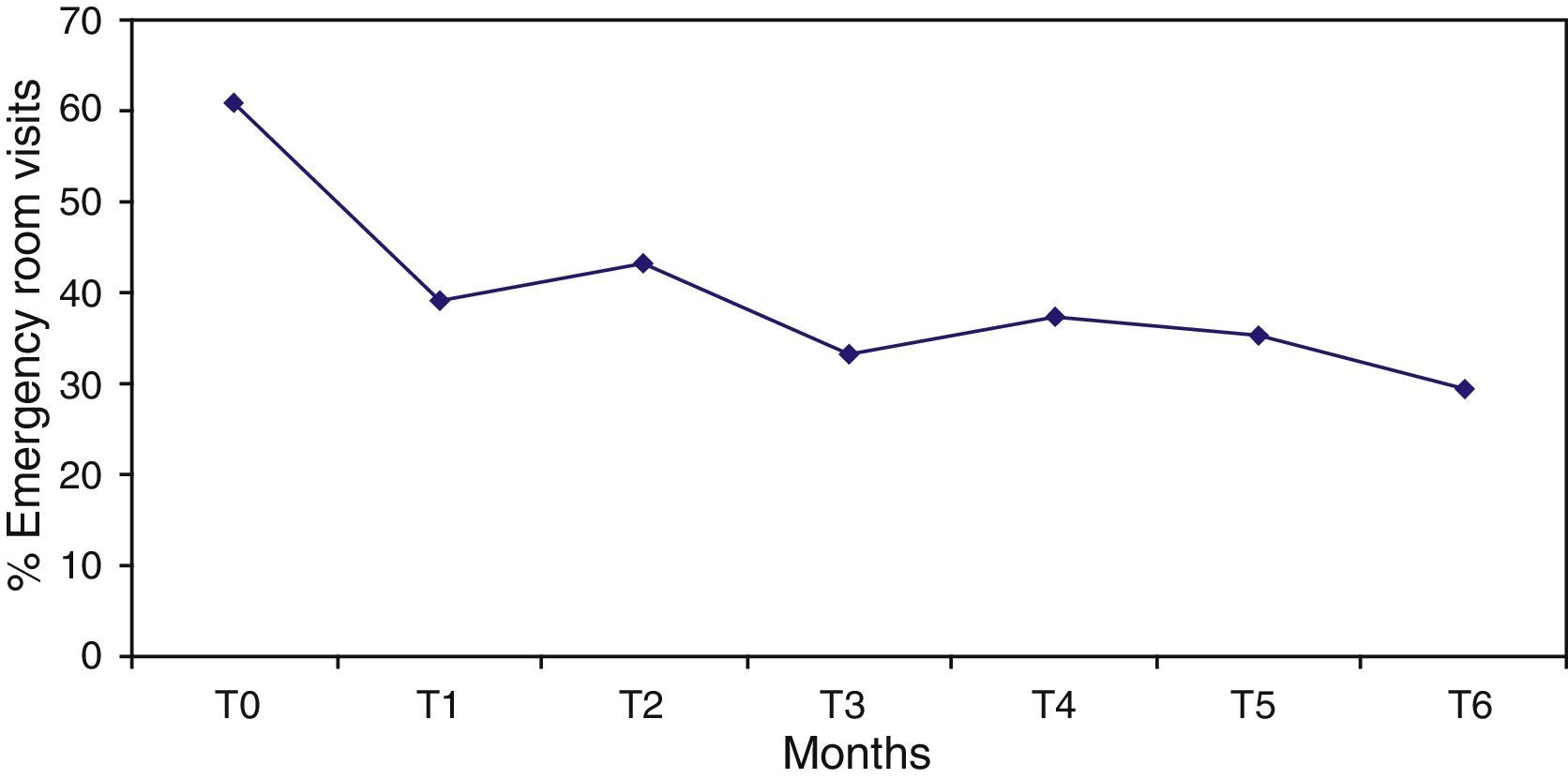
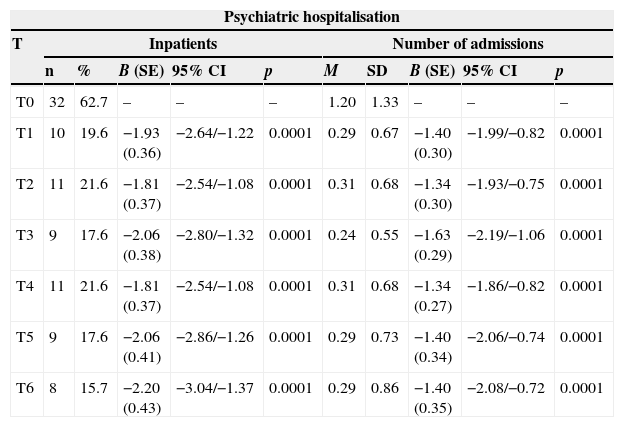
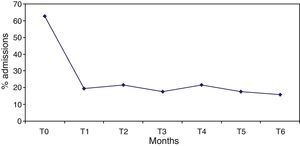
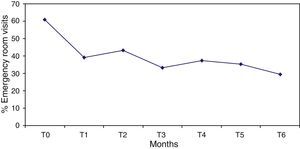
The percentage of hospitalised patients (Table 2) significantly decreased from 62.7%, in the 6 months prior to the programme start (T0), to 19.6% after 6 months of treatment (T1), and this reduction (Fig. 1) remained significantly stable (p<0.0001) in the 6 months prior to each assessment (T2–T6). Likewise, the mean number of admissions was reduced after treatment and remained stable during follow-up. Not only were patients admitted in a lower proportion and on less occasions, but also this improvement was also reflected in a decrease in hospital stay from 25.9 days in T0 (SD=29.5) to 3.5 days in T6 (SD=9.8), with an effect size of 0.8. Regarding psychiatric emergency, both the percentage of patients who visited it and the number of emergencies improved significantly, but the reduction was lower and more irregular throughout the follow-up period. Thus, in some time points (T3, T5 and T6) the improvement was very significant, and in others (T2), only slight (Table 2 and Fig. 2).
Outcome variables.
| Psychiatric hospitalisation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T | Inpatients | Number of admissions | ||||||||
| n | % | B (SE) | 95% CI | p | M | SD | B (SE) | 95% CI | p | |
| T0 | 32 | 62.7 | – | – | – | 1.20 | 1.33 | – | – | – |
| T1 | 10 | 19.6 | −1.93 (0.36) | −2.64/−1.22 | 0.0001 | 0.29 | 0.67 | −1.40 (0.30) | −1.99/−0.82 | 0.0001 |
| T2 | 11 | 21.6 | −1.81 (0.37) | −2.54/−1.08 | 0.0001 | 0.31 | 0.68 | −1.34 (0.30) | −1.93/−0.75 | 0.0001 |
| T3 | 9 | 17.6 | −2.06 (0.38) | −2.80/−1.32 | 0.0001 | 0.24 | 0.55 | −1.63 (0.29) | −2.19/−1.06 | 0.0001 |
| T4 | 11 | 21.6 | −1.81 (0.37) | −2.54/−1.08 | 0.0001 | 0.31 | 0.68 | −1.34 (0.27) | −1.86/−0.82 | 0.0001 |
| T5 | 9 | 17.6 | −2.06 (0.41) | −2.86/−1.26 | 0.0001 | 0.29 | 0.73 | −1.40 (0.34) | −2.06/−0.74 | 0.0001 |
| T6 | 8 | 15.7 | −2.20 (0.43) | −3.04/−1.37 | 0.0001 | 0.29 | 0.86 | −1.40 (0.35) | −2.08/−0.72 | 0.0001 |
| Days of hospitalisation | |||||
|---|---|---|---|---|---|
| T | M | SD | B (SE) | 95% CI | p |
| T0 | 25.9 | 29.5 | |||
| T1 | 4.8 | 12.7 | −21.16 (3.96) | −28.92/−13.39 | 0.0001 |
| T2 | 6.4 | 15.7 | −19.55 (3.84) | −27.08/−12.02 | 0.0001 |
| T3 | 8.8 | 23.5 | −17.18 (4.43) | −25.86/−8.50 | 0.0001 |
| T4 | 4.1 | 9.9 | −21.86 (3.83) | −29.37/−14.35 | 0.0001 |
| T5 | 5.1 | 14.8 | −20.82 (3.25) | −27.20/−14.45 | 0.0001 |
| T6 | 3.5 | 9.8 | −22.41 (3.54) | −29.35/−15.48 | 0.0001 |
| Psychiatric Emergency Room visit | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T | Patients | Number of Emergency Room visits | ||||||||
| n | % | B (SE) | 95% CI | p | M | SD | B (SE) | 95% CI | p | |
| T0 | 31 | 60.8 | – | – | – | 1.73 | 2.05 | – | – | – |
| T1 | 20 | 39.2 | −0.88 (0.41) | −1.68/−0.08 | 0.032 | 0.71 | 1.27 | −0.89 (0.26) | −1.41/−0.38 | 0.001 |
| T2 | 22 | 43.1 | −0.72 (0.34) | −1.34/−0.05 | 0.035 | 0.92 | 1.43 | −0.63 (0.26) | −1.14/−0.12 | 0.016 |
| T3 | 17 | 33.3 | −1.13 (0.38) | −1.88/−0.38 | 0.003 | 0.67 | 1.14 | −0.95 (0.26) | −1.46/−0.45 | 0.0001 |
| T4 | 19 | 37.3 | −0.96 (0.36) | −1.67/−0.25 | 0.008 | 1.00 | 1.85 | −0.55 (0.26) | −1.04/−0.05 | 0.032 |
| T5 | 18 | 35.3 | −1.04 (0.33) | −1.70/−0.39 | 0.002 | 0.59 | 0.94 | −1.08 (0.25) | −1.56/−0.59 | 0.0001 |
| T6 | 15 | 29.4 | −1.31 (0.34) | −1.98/−0.65 | 0.0001 | 0.63 | 1.28 | −1.01 (0.28) | −1.56/−0.46 | 0.0001 |
B: regression coefficient; SD: standard deviation; SE: standard error; 95% CI: 95% confidence interval; M: mean; p: probability value p; T0: it includes the six months before treatment start; T1: it includes the six months of treatment; T2: months 7–12 from treatment start; T3: months 13–18; T4: months 19–24; T5: months 25–30; T6: months 31–36.
Results indicate that in a sample of patients mainly diagnosed with BPD, of low sociocultural level, clinically very serious and with poor functioning, a multicomponent treatment which integrates effective techniques taken from different therapeutic models within a coherent and structured framework significantly reduces psychiatric readmissions and repeated Emergency Room visits, and these benefits continue over time.
The prevalence of self-aggressive and hetero-aggressive behaviour and substance abuse, prior to treatment start, was one of the highest among studies which do research into several psychotherapies, both in PDs in general, and in the BPD in particular.1,8–26 The prevalence of transient psychotic symptoms was also remarkable. This piece of information, despite being a DSM criterion, is facilitated by only a few studies,1,23 when, as emphasised by many authors,23,24 the combination of impulsivity and paranoid symptoms complicates the already difficult treatment of these patients. The baseline percentage of psychiatric admissions has also been associated with the severity of PDs admitted for treatment, as verified in two studies conducted in London with the MBT. In the first one,23 implemented in DH with a clinically more serious sample, almost 90% of patients were admitted during the year before therapy, while in the second,12 conducted in an outpatient setting, this percentage did not reach 29% during the previous 6 months. In addition, clinical seriousness of the sample was reflected by a very low global functioning level. Karterud et al.,24 consider that PDs with a higher functioning should receive outpatient treatment, while those with a score lower than 50 according to the GAF Scale could benefit from DH. However, if the GAF Scale score is lower than 40, the type of treatment offered in DH should be both qualitatively and quantitatively different, in line with that suggested by Bateman and Fonagy.23
During the stay in the programme, psychiatric admissions and the least desirable of the unscheduled visits, the Emergency Room visit, were considerably reduced. From the health care point of view, it is a very effective result, since, having no additional costs, it made it possible to modify the well-known tendency of PDs in general and BPDs in particular to short and recurring readmissions and/or extended hospitalisations. However, although some authors consider that the frequency of hospitalisation episodes constitutes a reasonable approximation to the serious suicidal behaviour, and the frequency of Emergency Room visits constitutes an approximation to severe self-inflicted lesions,12,34 the reduction in hospitalisations and Emergency Room visits does not guarantee a global clinical improvement. Considering all this, these are two pragmatic variables with a high health care value. It is worth mentioning that during the six months after discharge, together with a significant reduction in treatment hours, there was an increase in admissions and, above all, Emergency Room visits. Results also point to the fact that the beneficial effects may last over time, even with patients whose condition is serious and when outcome measures which do not depend on subjective judgements are used. Obviously, the continuance of the recovery cannot be attributed only to the programme for BPD, but it is likely that the usual psychiatric treatment, after completion thereof, would be more effective than before.
In the last few years, some authors5,7,24,45 have stated the need for conducting pragmatic studies to assess if the effectiveness reached in controlled studies may be replicated under usual practise conditions, since the information available is scarce.5,31 In this study, data were collected as part of the usual health care routine, which would reinforce the external validity thereof. However, a multicomponent programme, which requires interventions typical of a DBT, MBT, stress management, psychoeducation, support dynamic psychotherapy, pharmacological control, Nursing consultation and telephone consultation, entails a complex treatment which is difficult to replicate in the usual health care environment. However, if you think carefully, these interventions, except for groups based on DBT and MBT, are usually performed in different DHs, including individual psychotherapy. On the other hand, the DBT skill training manual explains that the DBT skill group may be combined with individual DBT or with another individual therapy model, and that this group may be led by Psychiatry residents, social workers and nurses.40 MBT group therapy does not require any extraordinary instruction either, and in London, it is performed by Nursing.23 The relational group of this programme introduced several MBT techniques, despite the fact that the main aspect was, as emphasised by Bateman and Fonagy,41 to change the therapeutic attitude towards a mentalisation attitude. Possibly, the greatest difficulty to implement such a programme is to generate a critical attitude which facilitates a structured protocol-based implementation of effective therapeutic strategies, and to maintain team commitment, supervision and cohesion.
As far as treatment duration is concerned, results indicate that a shorter than usual programme, even with serious PDs, may be enough to help a high percentage of patients, as stated by several authors,2,24,31 who advocate for optimising therapy effectiveness. It is important that treatments for PDs be effective, but also feasible and accessible. Otherwise, as they are more effective on more acute symptoms than on general functioning,14,31,32,34 we may face the paradox that when the patient makes a consultation, in general when he/she shows more impulsive symptoms, he/she is included in a long waiting list, just when the therapy might be more effective. Meanwhile, the percentage of patients who abandoned treatment cannot be compared to that of longer interventions, but after four months, it was similar to that described by other quarterly DH PD programmes.1,24
Finally, results show that an integrated therapeutic approach may be effective. The need for integrating several psychotherapeutic models is also a real situation which may be found on a daily basis in the mental health network sites, since it will not always be possible to make up a whole team in the same therapeutic model, or it may be even possible that not all health care providers are willing to do so. Moreover, some authors39 consider that a programme integrated by several interventions, if applied within a coherent and structured framework, may reduce resistance to change, anticipatory fear and, as a consequence, induce a lower linking anxiety.
The study has several limitations. The main one is the absence of a control group, and, therefore, results may only show the natural history of PDs. In this sense, BPD naturalistic follow-up studies46 show a spontaneous remission of impulsive symptoms, which could be more associated with admission and psychiatric emergency, in two to four years. However, in the only randomised controlled study with a long-term follow-up conducted in London in DH,34,47 with a BPD sampling with a similar seriousness to that studied herein, the progress of psychiatric admissions in patients who followed usual treatment, far from gradually improving, worsened, and was also very irregular. Thus, the percentage of hospitalisations of patients under usual treatment,47 whose impulsivity should also be improving from 24 months onwards, was 36.8% upon reaching such period, 36.8% after 30 months and 73.7% after 36 months of having started treatment. Something similar happened with mean hospital stay, which was of approximately 12 days after 6 months of treatment, 4 days after 12 months, 21 days after 18 months, 6 days after 24 months, 13 days after 30 months and 16 days after 36 months. Another limitation lies in the fact that it was not possible to feasibly record the progress of suicide attempts and self-inflicted lesions. It was not possible to use assessment scales either, except for those administered as part of health care routine, despite the fact that these tools are not usually employed in everyday practise. On the other hand, the study has several strengths which derive from its pragmatic design, the use of outcome measures which do not depend on subjective judgement, and the 36-month follow-up.
It may be concluded that, under usual practise conditions, treatment of BPDs may be effective and efficient when implemented according to therapeutic strategies which adapt evidence-based interventions,39 and benefits continue over time.
Ethical responsibilitiesPeople and animal protection. The authors declare that no experiments have been conducted in humans or animals for this research.
Data confidentialityThe authors declare that they have followed protocols in their working sites in relation to patients’ personal data disclosure.
Right to privacy and informed consentThe authors declare that this article does not contain patient-related data.
Conflict of interestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Lana F, Sánchez-Gil C, Ferrer L, López-Patón N, Litvan L, Marcos S, et al. Efectividad de un programa terapéutico integrado para trastornos graves de la personalidad. Seguimiento pragmático de 36 meses. Rev Psiquiatr Salud Ment (Barc.). 2015;8:3–10.