To analyse the differences in the quality of life of patients with psychosis according to the course of the illness.
MethodClinical records and SCID-I interviews were used to establish the course of the illness and to categorise it according to 3 criteria: (a) relapses, (b) residual symptoms, and (c) clinical diagnosis. Subjective quality of life was assessed with the Seville Questionnaire.
ResultsSixty one patients (56% women) participated, reporting a mostly adequate quality of life. An illness course characterised by the presence of residual symptoms, rather than by the occurrence of any relapse or the progression of a first-episode psychosis into schizophrenia, showed a negative effect on the perceived quality of life of patients.
ConclusionsThe clinical services provided to patients with psychosis should focus not only on symptoms remission and relapse prevention, but also achieving a recovery with a satisfactory quality of life. Having identified residual symptoms as a crucial factor negatively affecting quality of life, clinicians must carefully assess them and treat them, in order to achieve the best possible recovery.
Analizar las diferencias en la calidad de vida de pacientes con psicosis comparados de acuerdo con el curso de la enfermedad.
MétodoSe usaron las historias clínicas y la SCID-I para establecer el curso de la enfermedad, que se clasificó conforme a 3 criterios: a) recaídas, b) síntomas residuales y c) diagnóstico clínico primario. La calidad de vida subjetiva se evaluó con el cuestionario Sevilla.
ResultadosParticiparon 61 pacientes (el 56% mujeres) que, en general, refirieron un nivel de calidad de vida adecuado. El curso de la enfermedad, caracterizado por la presencia de síntomas residuales, más que por la experiencia de recaídas o la evolución de un primer episodio de psicosis a esquizofrenia, reveló un efecto negativo sobre la calidad de vida percibida por los pacientes.
ConclusionesLos servicios clínicos ofrecidos a los pacientes con psicosis han de enfocarse no solo en la remisión de los síntomas y prevención de las recaídas sino también en la obtención del restablecimiento con una calidad de vida satisfactoria. Puesto que se han identificado los síntomas residuales como un factor esencial que afecta de modo negativo a la calidad de vida, los médicos han de valorarlos cuidadosamente a fin de lograr el mayor grado posible de restablecimiento del paciente.
The experts have now reached a consensus that the psychoses of the schizophrenia spectrum no longer mean an inexorable progression towards deterioration and the first psychosis episode can follow varying courses–from the complete reestablishment of the patient to becoming a chronic case.1 In addition, the tests suggest that, if they occur, deterioration and/or recurrences are more likely in the first 3–5 years after psychosis onset (the “critical period”); later on, the illness seems to become stable.2,3 Consequently, the progression of psychosis can become stable in the initial years and not all cases evolve to a persistent or devastating psychosis. As far as the diagnosis goes, after approximately 6 months’ evolution, the psychosis can be classified as schizophrenia or other type of non-affective psychosis.4 Other criteria used to evaluate its progression are the presence of residual symptoms5 and the incidence of later recurrences.5,6
In mental health treatment, given the current perspectives, the objective is not only to obtain remission (disappearance or attenuation of the presence and the severity of the basic symptoms of the disorder). It also covers patient reestablishment, which includes remission, appropriate psychosocial functional outcomes and a satisfactory quality of life.7 Research, public health policies and medical programmes have adopted the concept of health-linked quality of life to evaluate the effects of chronic illnesses (for example, schizophrenia) on daily patient functioning, their satisfaction with life and how they relate to several health indexes (including, among others, demographic, social, economic, accessibility and coverage).
Insofar as the diagnostic course, although research indicates that patients with schizophrenia experience a significantly more unfavourable quality of life,8 they do not seem more affected in comparison with patients having other types of psychosis.9 A recurrent course10 and residual psychopathology11 has also been linked to a decrease in quality of life. This is a variable as important as it is complex, and research has provided evidence of how it can be affected by various sociodemographic, clinical, social and therapeutic factors.8,9 Various factors and scales have been proposed to assess it.8 Quality of life undoubtedly runs the risk of being negatively impacted when the patient has a psychotic episode. However, given that the course of the illness varies a lot, we have to investigate differences in quality of life for patients with psychosis when comparing them based on the course of their illness, which constitutes the objective of the present study. Knowing the individual effect of diagnostic, recurrent or symptomatic progression of the psychosis on quality of life would make it easier to identify the patients requiring greater support and resources to achieve satisfactory reestablishment.
MethodsThis study was carried out in a public psychiatric hospital in Mexico after obtaining formal authorisation and ethical approval from the hospital's research ethics committee. We reviewed the clinical histories in the search of patients that fulfilled the following inclusion criteria: (a) incidence of an initial psychotic episode 5–11 years earlier (so all the patients would have overcome the critical period); (b) age at onset: 16–45 years old; (c) current primary diagnosis of schizophrenia or other psychotic disorder based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders [DSM-IV-TR])4; and (d) inhabitants of the city of Mérida, where the hospital is located. The criteria for exclusion were: (a) psychosis of an affective, organic or toxic type,4 (b) a clear intellectual disorder and (c) insufficient contact information. Of the 103 patients that we contacted, 5 could not participate because of the notable severity of the symptoms. Of the remaining patients, 61 (62.2%) agreed to be interviewed, signing an informed consent form, without economic compensation.
When the patients were evaluated, we used the clinical histories and the structured clinical interview for DSM disorders (SCID-I)12 to establish the course of the illness and to classify it according to the following 3 criteria: (a) recurrences, (b) residual symptoms and (c) primary clinical diagnosis. Residual symptoms are the signs of the disorder manifested by: (i) only negative symptoms or (ii) 2 or more characteristic symptoms (delusions, hallucinations, unorganised and incoherent language, clearly unorganised or catatonic behaviour, and negative symptoms present in an attenuated manner (subthreshold) (e.g., strange thoughts or beliefs or highly unusual perceptive experiences).4 A recurrence (a later psychotic episode) is defined as “the incidence of any major modification belonging to the psychological clinical picture, which causes the patient to be referred to a psychiatric centre, to increase the dosage of the antipsychotic medication, or to be admitted to hospital”.6 A recurrence could have occurred as a change from (1) a state of complete reestablishment (absence of psychotic symptoms) to the reappearance of psychotic symptoms, or (2) a state of partial reestablishment (stable state of persistent symptoms) up to a clear worsening of the psychotic symptoms.5
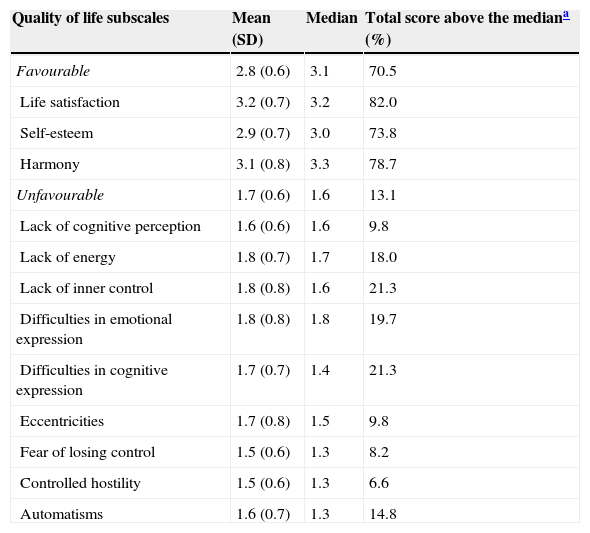
Subjective quality of life was evaluated using the Sevilla questionnaire,13 a self-assessed 59-item Likert scale questionnaire, formulated for patients with schizophrenia. This questionnaire consists of a scale for favourable aspects and another for unfavourable aspects, with 3 and 9 subscales, respectively (Table 1).
Descriptive statistics for quality of life (n=61).
| Quality of life subscales | Mean (SD) | Median | Total score above the mediana (%) |
|---|---|---|---|
| Favourable | 2.8 (0.6) | 3.1 | 70.5 |
| Life satisfaction | 3.2 (0.7) | 3.2 | 82.0 |
| Self-esteem | 2.9 (0.7) | 3.0 | 73.8 |
| Harmony | 3.1 (0.8) | 3.3 | 78.7 |
| Unfavourable | 1.7 (0.6) | 1.6 | 13.1 |
| Lack of cognitive perception | 1.6 (0.6) | 1.6 | 9.8 |
| Lack of energy | 1.8 (0.7) | 1.7 | 18.0 |
| Lack of inner control | 1.8 (0.8) | 1.6 | 21.3 |
| Difficulties in emotional expression | 1.8 (0.8) | 1.8 | 19.7 |
| Difficulties in cognitive expression | 1.7 (0.7) | 1.4 | 21.3 |
| Eccentricities | 1.7 (0.8) | 1.5 | 9.8 |
| Fear of losing control | 1.5 (0.6) | 1.3 | 8.2 |
| Controlled hostility | 1.5 (0.6) | 1.3 | 6.6 |
| Automatisms | 1.6 (0.7) | 1.3 | 14.8 |
Firstly, the quality of life reported by the entire sample was analysed, obtaining the mean, standard deviation (SD) and medians for the scores achieved on the total scale and on the subscales. The percentage of participants whose scores (total and by subscale) were greater than the mean (that is, 2.5 in an interval of 1–4). The patients were immediately assigned to 1 of 2 groups based on whether they had experienced a recurrence or not; the mean quality of life scored achieved were then compared using a T-test for independent samples. The level of significance was set as P=.05. The same procedure was followed to classify the patients that presented residual symptoms (or not) at the time of the assessment and lastly, to classify the patients based on the diagnosis of schizophrenia or another type of psychosis. All statistical analyses were processed using the computer package SPSS version 19.
ResultsAt the time of evaluation, no patients were hospitalised. However, 50.8% of them had been hospitalised at least once, and 34.4% had been hospitalised when they the first psychosis episode occurred. The mean course of the illness was 6.7 years (SD=1.9; limits 3.8–11.2). Current mean age was 35.9 years (SD=10) and the mean age at the onset of psychosis was 29.1 years (SD=9.8). Most participants (49.2%) were single; 42.6% were married or had a partner; and 8.2% were divorced/separated. The majority of them still lived with their parents (54.1%) and their level of education was ≤9 years (55.7%). As for occupation, 34.4% reported that they were responsible for the household tasks, 44.3% were self-employed and 21.3% lacked any official occupation. Females represented 56% of the sample; no statistically significant differences by sex were identified for the 3 variables mentioned earlier.
Table 1 presents the descriptive statistics corresponding to quality of life. No statistically significant differences in sex were found for any of the subscales. The participants generally reported an appropriate quality of life: for all the favourable dimension means, the participants obtained scores of more than 3 and for all the means of the unfavourable dimension they obtained scores of less than 2. These positive results are confirmed when median scores and the percentage of patients with scores higher and lower than the mean score (2.5) in the favourable and unfavourable dimensions, respectively.
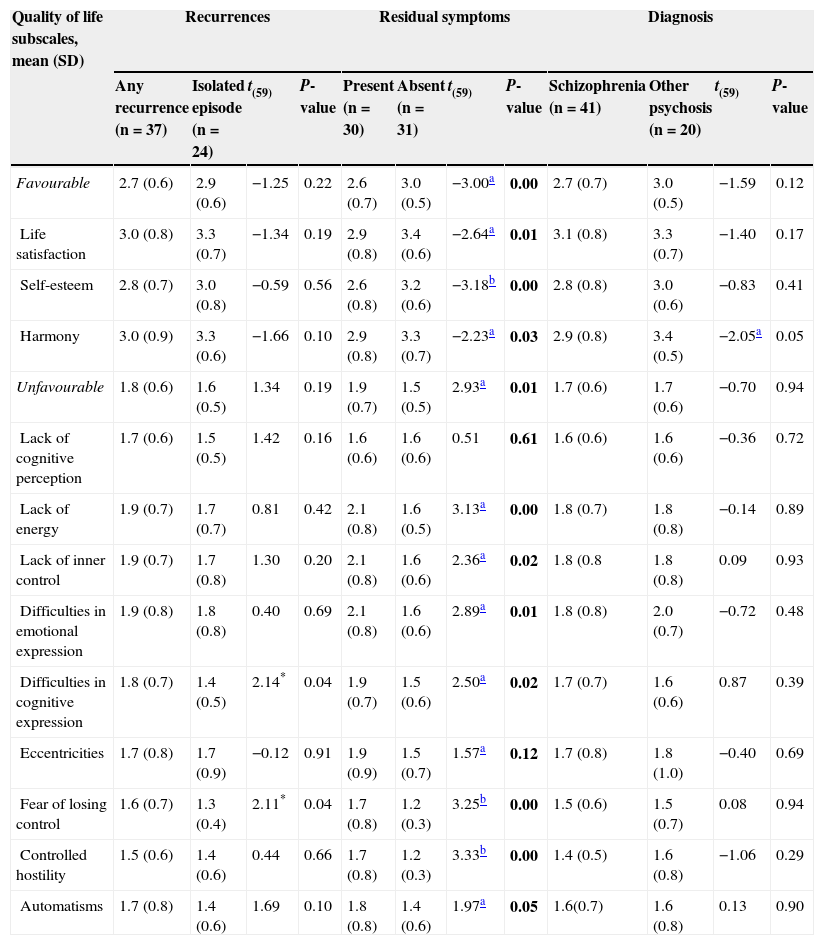
Table 2 presents the case distribution based on the 3 criteria and the differences in the course of the illness when the quality of life scores are compared between groups. As for the distributions of the course of the illness, 39.3% experienced recurrences, while 60.7% only experienced a single episode of psychosis. At the time of the evaluation, 50.8% of the participants were free from residual symptoms; 67.2% presented schizophrenia (14 paranoid, 2 unorganised and 25 residual) and the remaining 32.8% presented other types of psychosis (8 schizoaffective, 7 delusional, 2 schizophreniform, 2 short and 1 not otherwise specified).
Differences in quality of life by the course of the illness (n=61).
| Quality of life subscales, mean (SD) | Recurrences | Residual symptoms | Diagnosis | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any recurrence (n=37) | Isolated episode (n=24) | t(59) | P-value | Present (n=30) | Absent (n=31) | t(59) | P-value | Schizophrenia (n=41) | Other psychosis (n=20) | t(59) | P-value | |
| Favourable | 2.7 (0.6) | 2.9 (0.6) | −1.25 | 0.22 | 2.6 (0.7) | 3.0 (0.5) | −3.00a | 0.00 | 2.7 (0.7) | 3.0 (0.5) | −1.59 | 0.12 |
| Life satisfaction | 3.0 (0.8) | 3.3 (0.7) | −1.34 | 0.19 | 2.9 (0.8) | 3.4 (0.6) | −2.64a | 0.01 | 3.1 (0.8) | 3.3 (0.7) | −1.40 | 0.17 |
| Self-esteem | 2.8 (0.7) | 3.0 (0.8) | −0.59 | 0.56 | 2.6 (0.8) | 3.2 (0.6) | −3.18b | 0.00 | 2.8 (0.8) | 3.0 (0.6) | −0.83 | 0.41 |
| Harmony | 3.0 (0.9) | 3.3 (0.6) | −1.66 | 0.10 | 2.9 (0.8) | 3.3 (0.7) | −2.23a | 0.03 | 2.9 (0.8) | 3.4 (0.5) | −2.05a | 0.05 |
| Unfavourable | 1.8 (0.6) | 1.6 (0.5) | 1.34 | 0.19 | 1.9 (0.7) | 1.5 (0.5) | 2.93a | 0.01 | 1.7 (0.6) | 1.7 (0.6) | −0.70 | 0.94 |
| Lack of cognitive perception | 1.7 (0.6) | 1.5 (0.5) | 1.42 | 0.16 | 1.6 (0.6) | 1.6 (0.6) | 0.51 | 0.61 | 1.6 (0.6) | 1.6 (0.6) | −0.36 | 0.72 |
| Lack of energy | 1.9 (0.7) | 1.7 (0.7) | 0.81 | 0.42 | 2.1 (0.8) | 1.6 (0.5) | 3.13a | 0.00 | 1.8 (0.7) | 1.8 (0.8) | −0.14 | 0.89 |
| Lack of inner control | 1.9 (0.7) | 1.7 (0.8) | 1.30 | 0.20 | 2.1 (0.8) | 1.6 (0.6) | 2.36a | 0.02 | 1.8 (0.8 | 1.8 (0.8) | 0.09 | 0.93 |
| Difficulties in emotional expression | 1.9 (0.8) | 1.8 (0.8) | 0.40 | 0.69 | 2.1 (0.8) | 1.6 (0.6) | 2.89a | 0.01 | 1.8 (0.8) | 2.0 (0.7) | −0.72 | 0.48 |
| Difficulties in cognitive expression | 1.8 (0.7) | 1.4 (0.5) | 2.14* | 0.04 | 1.9 (0.7) | 1.5 (0.6) | 2.50a | 0.02 | 1.7 (0.7) | 1.6 (0.6) | 0.87 | 0.39 |
| Eccentricities | 1.7 (0.8) | 1.7 (0.9) | −0.12 | 0.91 | 1.9 (0.9) | 1.5 (0.7) | 1.57a | 0.12 | 1.7 (0.8) | 1.8 (1.0) | −0.40 | 0.69 |
| Fear of losing control | 1.6 (0.7) | 1.3 (0.4) | 2.11* | 0.04 | 1.7 (0.8) | 1.2 (0.3) | 3.25b | 0.00 | 1.5 (0.6) | 1.5 (0.7) | 0.08 | 0.94 |
| Controlled hostility | 1.5 (0.6) | 1.4 (0.6) | 0.44 | 0.66 | 1.7 (0.8) | 1.2 (0.3) | 3.33b | 0.00 | 1.4 (0.5) | 1.6 (0.8) | −1.06 | 0.29 |
| Automatisms | 1.7 (0.8) | 1.4 (0.6) | 1.69 | 0.10 | 1.8 (0.8) | 1.4 (0.6) | 1.97a | 0.05 | 1.6(0.7) | 1.6 (0.8) | 0.13 | 0.90 |
Statistically significant results (P≤0.05) in bold type.
Considering the overall scores, it can be seen (Table 2) that the residual symptom criteria were the only ones that showed statistically significant differences between groups and on both scales, favourable and unfavourable. In addition, the patients without residual symptoms obtained a more favourable score in 11 (10 of them statistically significant) of the 12 quality of life subscales. In contrast, the criteria for recurrences and diagnosis detected only 2 and 1 significant differences, respectively. In short, the criteria for residual symptoms, more than the diagnosis or recurrences, revealed firm differences that were significant mainly in the majority of the quality of life dimensions. This indicated that the patients with residual symptoms had a poorer quality of life, in comparison with those free from these symptoms.
DiscussionIndependently of the course of the illness, and coinciding with previous studies carried out with samples of individuals if Spanish–American origin,14 the participants barely reported affects on quality of life. This evidence not only supports a more optimistic view of psychosis when the individual reaches reestablishment, it shows that a satisfactory quality of life is possible. It also formulates the question as to why the patients living in developed countries report a poorer quality of life compared with the others. It has been proposed that the social and cultural contexts, with a less competitive environment and more moderates life requirements (such as those found in Spanish–American countries) could constitute key influences in this phenomenon.14
Residual psychopathology has been linked to a poorer quality of life.11 In addition, these results suggest that illness progression characterised by residual symptoms, more than the incidence of a recurrence or the evolution of a first episode of psychosis in schizophrenia, negatively affects the patients’ perceived quality of life. Residual symptoms, whether related to possible adverse effects of the treatment or not, can influence subjective wellbeing indirectly through their intromission in the disorder, affecting the individual's social functioning and perceptions about general health and limiting the role played by the individual due to emotional problems.15 This not only reduces the outcomes of positive reinforcement stemming from highly valued activities, it also reduces the sensation of personal control; this in turn limits the capacity to obtain positive outcomes and/or avoid negative ones.16
Due to the design of this study, the information on therapeutic prescription and treatment adherence was not appropriately analysed. Consequently, we cannot provide precise, more detailed interpretations of the factors that are the basis for the residual symptoms. An evaluation in greater depth of the psychopathology and functionality would also open the possibility of making additional, more precise interpretations. Quality of life is an outcome that is both important and complex. It is influenced by a series of environmental and psychological factors. Future research needs to consider more rigorous and objective registration, and that of other pertinent data from the beginning (or even earlier) during the following years. Apart from these limitations, this study provides some interesting findings on a possible association between the course of the illness (recurrences, residual symptoms and diagnosis) and quality of life. However, it has to be recognised that a prospective design would make a more precise and extensive register of the information possible. This is especially true if you consider that psychosis is a disorder that is likely to vary over time and, for this reason, the way that the patient perceives his/her quality of life can also vary. In addition, a larger sample, evaluated in repeated visits over time (that is, at different points of evolution) would allow a more in-depth analysis by diagnosis and clinical profile, which would improve the possibility of generalising our results.
In the clinical services that have patients with psychosis, attention should not be given only to symptom remission and prevention of recurrences, the objective should be providing patient reestablishment associated with a satisfactory quality of life. As residual symptoms have been identified as a decisive factor that affects quality of life negatively, physicians need to evaluate these symptoms carefully and treat them to obtain reestablishment to the highest level possible.
Ehical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe author declares that there is no conflict of interest.
The authors wish to express their gratitude to the National Council of Science and Technology (CONACyT in Spanish), Mexico, for granting a doctoral fellowship (187498), and to the Hospital Psiquiátrico Yucatán for their support, as well as all the participants included in the study.
Please cite this article as: Gómez-de-Regil L. Curso de la enfermedad y calidad de vida en pacientes mexicanos con psicosis. Rev Psiquiatr Salud Ment (Barc.). 2015;8:218–223.