Many studies have demonstrated that the risk of suicide in prison is higher than in the general population. This study has two aims. First, to explore the risk of suicide in men sentenced in Andalusian prisons. And second, to study the sociodemographic, criminal and, especially, psychopathological factors associated with this risk.
MethodsAn assessment was made of 472 sentenced inmates in two Andalusian prisons, and included a sociodemographic interview, the IPDE personality disorders questionnaire, the SCID-I diagnostic interview (DSMIV), and the Plutchick suicide risk questionnaire. The interviewers were experienced clinical psychologists with training in prison environments. Adjusted ORs were calculated using a logistic regression.
ResultsA risk of committing suicide was detected in 33.5% of the sample. The diagnoses (lifetime prevalence) of affective disorder (adjusted OR 3329), substance dependence disorders (adjusted OR 2733), personality disorders (adjusted OR 3115) and anxiety disorder (adjusted OR 1650), as well as a family psychiatric history (adjusted OR 1650), were the predictors that remained as risk factors after the regression analysis. No socio-demographic risk factor was significant in the regression analysis.
ConclusionsThe psychopathological variables are essential and the most powerful factors to explain suicide risk in prisons. A correct and systematic diagnosis, and an appropriate treatment by mental health professionals during the imprisonment are essential to prevent the risk of suicide.
Numerosas investigaciones muestran que el riesgo de suicidio en los centros penitenciarios es superior al de la población general. Los objetivos del trabajo son primero explorar el riesgo de suicidio de internos condenados masculinos en centros penitenciarios andaluces; y segundo, estudiar los factores sociodemográficos, penales y, especialmente, psicopatológicos, asociados a este riesgo.
MétodosFueron evaluados 472 internos con condena de 2 centros penitenciarios andaluces aplicándose una entrevista sociodemográfica, el cuestionario de trastornos de personalidad IPDE, la entrevista diagnóstica SCID-I (DSMIV) y el cuestionario de riesgo suicida Plutchick. Los evaluadores fueron psicólogos clínicos entrenados con experiencia en el medio penitenciario. Se calcularon los OR crudos y ajustados por medio de la ejecución de una regresión logística.
ResultadosEl 33,5% de la muestra se encuentra en situación de riesgo de cometer suicidio. Los diagnósticos (prevalencia vida) de trastorno afectivo (OR ajustado 3.329), por dependencia (OR ajustado 2.733), un trastorno de personalidad (OR ajustado 3.115) y trastorno de ansiedad (OR ajustado 1.650) junto con los antecedentes psiquiátricos familiares (OR ajustado 1.650) fueron las variables predictivas que resistieron como factores de riesgo el análisis de regresión. Ninguna variable sociodemográfica con OR crudos significativos resistió el análisis de regresión.
ConclusionesLas variables psicopatológicas son esenciales y las más potentes para explicar el riesgo suicida en el medio penitenciario. Un correcto y exhaustivo diagnóstico, seguido del adecuado tratamiento por profesionales de salud mental durante los internamientos penitenciarios son esenciales para prevenir el riesgo de suicidio.
The suicide rate in prisons is significantly higher than the rate in the general population both in Spain and in the world.1–4 In Spain, the suicide rate in prisons was 0.46 per 1000 in 2006, higher than the rate of the normal population in that year, which was 0.11 for men and 0.03 for women.5 Nevertheless, we should indicate that since the implementation of the Framework Programme for Suicide Prevention in prisons (regulated by directive 14/2005), the suicide rate has dropped over the last decade. Specifically, based on the data from correctional centres, the suicide rate has fallen from 0.54 to 0.41 suicides per 1000 in 2000–2009.6
Due to the relevance of the question, some national and international studies have attempted to establish what the factors associated to the risk of committing suicide in penitentiary surrounds are. For example, Blaauw, Kerhof, Lindsay and Hayes,2 by analysing 95 suicide cases in Dutch jails, determined that a combination of 2 demographic variables (age over 40 years and lack of a home), 2 legal variables (previous imprisonment and violent crime) and 2 variables related to psychological disorders (history of psychiatric treatment and of drug abuse) could predict 82% of the suicide victims in the Dutch prison population with a specificity of 0.82.2 These authors also warned of the difficulties in linking suicidal behaviour (ideation, attempts and successful suicides) with different psychiatric disorders because of how hard it is to identify and diagnose inmates correctly in prison surroundings. Suffering from a psychiatric disorder is very important risk factor clearly related to suicide risk.6–8
The most common psychiatric disorders in the prison population at risk for suicide are psychotropic substance dependence, affective disorders and psychotic disorders.9 With respect to psychotic disorders, some authors warn us about the importance of considering positive symptoms and not only the simple diagnosis.10
Negredo, Melis and Herrero6 recently studied suicidal behaviour in 29 inmates in the psychiatric prison hospital in Foncalent, with 11 female inmates from the same centre and 6 male controls. These authors point out in their conclusions that, in addition to depressive type psychopathology and the disorders linked to substance abuse, the features of the uninhibited, antisocial and aggressive personality are important to bear in mind. This fact leads us to consider personality disorders (axis II of the DSM) in the study of suicidal behaviour in the prison population.6
Apart from psychopathological factors, other sociodemographic and legal variables have been pointed out to explain suicidal behaviour. For example, some factors that present a higher risk of suicidal behaviour (ideation, attempts and suicide) are being male, being preventative, not having a partner or suffering from social isolation,11 having received a previous sentence,12 committing violent crimes,5 serving a sentence in the source country and being more than 40 years old.6 As far as age, there are studies that indicate that being young is a risk factor.13 In addition, recent studies have found that being married behaves like a risk factor, although a small one.14 This contradicts the consideration of not having a partner as a risk factor. In the other variables considered risk factors, there is little or no argument as to their influence on suicidal behaviour in prisons.
The objectives of this study were double: firstly, to determine the suicide risk of sentenced men in prisons in Andalucía; and secondly, to study the association of this risk to a set of sociodemographic, legal and psychiatric variables.
MethodParticipantsWe randomly selected 500 male sentenced inmates in prisons in Andalucía, based on the data facilitated by the administration of 2 prisons. There were 250 inmates from Albolote prison (Granada) and 250 from Morón prison (Sevilla). Morón and Albolote are the prisons with the highest number of inmates in Andalucía. Specifically, when the inmates were selected, Morón prison held 1712 inmates and Albolote, 1754. Due to the large population in these prisons, extensive mobility of prison population and lack of different admission profiles in the jails in Andalucía we believe that these prisons are representative of the prisons in Andalucía. Inclusion criteria for the inmates were having sufficient command of Castilian Spanish (ability to understand the interviewers’ questions and respond appropriately), not having any neurological illness and having more than 6 months left to serve on their sentence. Out of the 500 inmates initially contacted, 472 were assess in the end; there were 247 inmates in Morón prison (52.33%) and 225 in Albolote (47.67%). The number of inmates that refused to participate and sign the informed consent was 18 (3.6%) and there were 3 data lost. Almost all the inmates that refused to sign the consent form belonged to organised groups of a political or religious nature. The rest of the inmates were not included in the sample because they did not fulfil the criteria for inclusion. The inmates initially selected that could not be found in these 2 prisons because of, for example, having changed prisons or having been released were substituted using individuals in a reserve list that was also randomised by modules.
The final sample was representative for a prison population of 15,000 inmates in Andalucía, with 2% precision, 95% confidence interval (CI) and a value of the parameter to be measured of 0.5. All the inmates participating gave their written informed consent. At that time, they were assigned a code so that the study could be carried out without identifying the participants at any time. The selection and execution of the study was approved by the management at the prisons and correctional centres. A commission of the Fundación Andaluza Pública for the integration of the mentally ill (FAISEM in Spanish) and the management of the prisons supervised the progression of the project with the aim of complying with all ethical requirements.
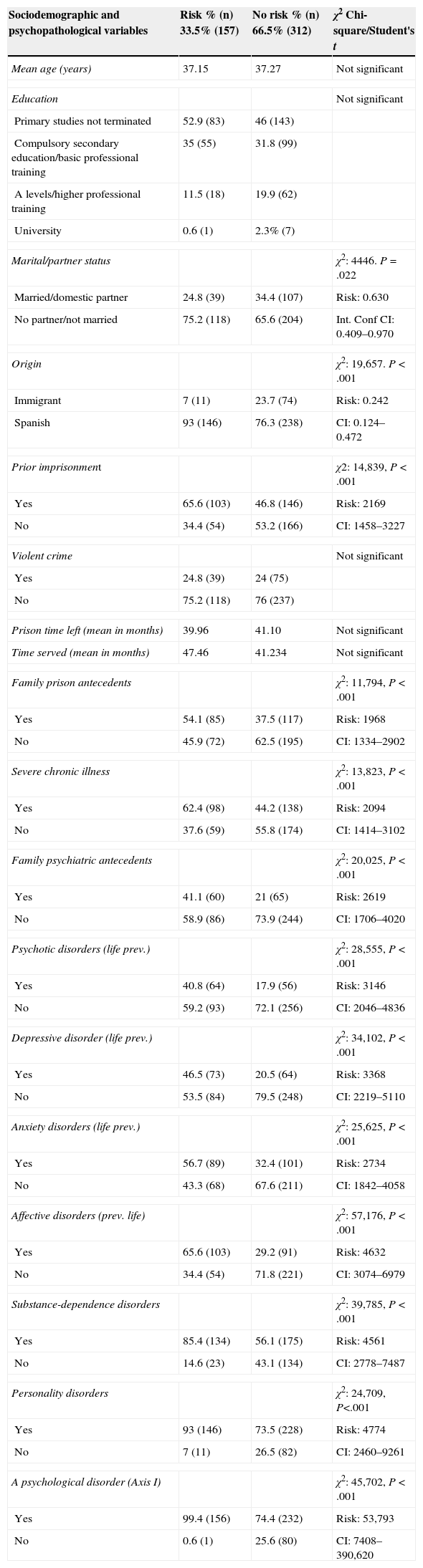
Table 1 describes our study sample. It can be seen that the mean age is slightly below 40 years old, that the inmates have a very low educational level, the majority have not got partners, 18% are immigrants, practically half the inmates have been imprisoned before and that there is a very elevated life prevalence of psychological disorders.
Description of the sample and associated suicide risk (crude odd ratios [ORs]).
| Sociodemographic and psychopathological variables | Risk % (n) 33.5% (157) | No risk % (n) 66.5% (312) | χ2 Chi-square/Student's t |
|---|---|---|---|
| Mean age (years) | 37.15 | 37.27 | Not significant |
| Education | Not significant | ||
| Primary studies not terminated | 52.9 (83) | 46 (143) | |
| Compulsory secondary education/basic professional training | 35 (55) | 31.8 (99) | |
| A levels/higher professional training | 11.5 (18) | 19.9 (62) | |
| University | 0.6 (1) | 2.3% (7) | |
| Marital/partner status | χ2: 4446. P=.022 | ||
| Married/domestic partner | 24.8 (39) | 34.4 (107) | Risk: 0.630 |
| No partner/not married | 75.2 (118) | 65.6 (204) | Int. Conf CI: 0.409–0.970 |
| Origin | χ2: 19,657. P<.001 | ||
| Immigrant | 7 (11) | 23.7 (74) | Risk: 0.242 |
| Spanish | 93 (146) | 76.3 (238) | CI: 0.124–0.472 |
| Prior imprisonment | χ2: 14,839, P<.001 | ||
| Yes | 65.6 (103) | 46.8 (146) | Risk: 2169 |
| No | 34.4 (54) | 53.2 (166) | CI: 1458–3227 |
| Violent crime | Not significant | ||
| Yes | 24.8 (39) | 24 (75) | |
| No | 75.2 (118) | 76 (237) | |
| Prison time left (mean in months) | 39.96 | 41.10 | Not significant |
| Time served (mean in months) | 47.46 | 41.234 | Not significant |
| Family prison antecedents | χ2: 11,794, P<.001 | ||
| Yes | 54.1 (85) | 37.5 (117) | Risk: 1968 |
| No | 45.9 (72) | 62.5 (195) | CI: 1334–2902 |
| Severe chronic illness | χ2: 13,823, P<.001 | ||
| Yes | 62.4 (98) | 44.2 (138) | Risk: 2094 |
| No | 37.6 (59) | 55.8 (174) | CI: 1414–3102 |
| Family psychiatric antecedents | χ2: 20,025, P<.001 | ||
| Yes | 41.1 (60) | 21 (65) | Risk: 2619 |
| No | 58.9 (86) | 73.9 (244) | CI: 1706–4020 |
| Psychotic disorders (life prev.) | χ2: 28,555, P<.001 | ||
| Yes | 40.8 (64) | 17.9 (56) | Risk: 3146 |
| No | 59.2 (93) | 72.1 (256) | CI: 2046–4836 |
| Depressive disorder (life prev.) | χ2: 34,102, P<.001 | ||
| Yes | 46.5 (73) | 20.5 (64) | Risk: 3368 |
| No | 53.5 (84) | 79.5 (248) | CI: 2219–5110 |
| Anxiety disorders (life prev.) | χ2: 25,625, P<.001 | ||
| Yes | 56.7 (89) | 32.4 (101) | Risk: 2734 |
| No | 43.3 (68) | 67.6 (211) | CI: 1842–4058 |
| Affective disorders (prev. life) | χ2: 57,176, P<.001 | ||
| Yes | 65.6 (103) | 29.2 (91) | Risk: 4632 |
| No | 34.4 (54) | 71.8 (221) | CI: 3074–6979 |
| Substance-dependence disorders | χ2: 39,785, P<.001 | ||
| Yes | 85.4 (134) | 56.1 (175) | Risk: 4561 |
| No | 14.6 (23) | 43.1 (134) | CI: 2778–7487 |
| Personality disorders | χ2: 24,709, P<.001 | ||
| Yes | 93 (146) | 73.5 (228) | Risk: 4774 |
| No | 7 (11) | 26.5 (82) | CI: 2460–9261 |
| A psychological disorder (Axis I) | χ2: 45,702, P<.001 | ||
| Yes | 99.4 (156) | 74.4 (232) | Risk: 53,793 |
| No | 0.6 (1) | 25.6 (80) | CI: 7408–390,620 |
A team of 8 clinical psychologists with experience in prison settings, divided into groups of 4 in each prison, diagnosed the selected inmates using a battery of instruments. The interviewers were previously trained in the use of the assessment instruments, especially in the application of the Structured Clinical Interview for the DSM axis I disorders (SCID-I) diagnostic interview. The training in the use of this interview took place by the use of clinical cases provided by the project coordinator, until acceptable reliability among the interviewers was attained. At the end of the training period, the 8 interviewers reached at least 80% agreement in the diagnosis of the clinical cases. Once a month, seminars were held with each team to analyse and supervise the inmate diagnoses in which there were doubts. If necessary, a group diagnosis was established at these meetings with at least 75% agreement among the 4 interviewers and the coordinator. The design, the contact with the prisons and the diagnoses were all carried out between 2011 and 2012. In this period, 2 psychologists trained in the instruments used introduced the assessment results in the data table and refined possible errors; finally, the analyses were carried out.
Instruments and analysisThe sociodemographic, penal and family clinical history data were obtained by sociodemographic interviews. When necessary, the data obtained in the interviews was confirmed using the information available to the prisons. The clinical version of the well-known SCID for the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) was used to diagnose axis I disorders.
The questionnaire associated with the International Personality Disorder Examination (IPDE) was applied to explore personality disorders. The IPDE questionnaire consists of 59 items that measure the 59 criteria of the total of the 9 personality disorders.15 Some authors have found, with opiate-addicted populations and a cut-off of 2/3, sensitivity of 88–100% and specificity of 37–98% among the personality disorders. In our case, we used the more conservative cut-off point of 4 or more unexpected answers.16
Suicide risk was assessed using the Spanish version of Plutchik's suicide risk scale.17 Its objective is to differentiate between normal individuals and those that are at risk of committing suicide, using the answers to 15 “Yes-No” questions. The cut-off point at which to consider risk is 6 points. This cut-off achieves sensitivity of 74% and specificity of 95% to distinguish between controls and patients. In the Spanish validation, Cronbach's alpha was 0.90 and the reliability after 72h was a test–retest of 0.89.18 The Cronbach's alpha of our sample was 0.8. Although this scale can be self-administered, the interviewers explored the inmates’ answers to make sure that the questions were understood and to get more details on some positive answers (for example, to the item that explores suicide attempts.
Apart from the instruments described, whose results we have used in this study, the battery of instruments selected included 2 questionnaires used in social health services (the last year of sentences and 1 year before prison confinement), Moors organisational climate in prisons questionnaire and a questionnaire on general health, as well as the Toni II intelligence test.
We first applied the Chi-square test and found the crude odds ratios (OR) of exceeding the cut-off in the suicide risk scale for the dichotomous categorical variables (0.1) with a confidence interval (CI) of 95%. For the quantitative variables, we applied only Student's t-test of mean contrasts. In agreement with the literature on the subject, we studied the following sociodemographic and penal factors: age, educational level, marital/partner status (married–unmarried partner–no partner), geographical origin (Spaniard or immigrant), previous imprisonment, sentenced for violent crime, sentence time remaining, time served, family penal antecedents and history of chronic organic illness. We considered only the severe, long-term or chronic illnesses (such as cancer, HIV, AIDS, hepatitis, cardiovascular disorders, asthma, pulmonary emphysema, etc. As for the psychopathological variables, we considered the existence or lack of diagnoses (life prevalence): family psychiatric antecedents, psychotic disorders, depressive disorder, anxiety disorders, affective disorders, substance dependence disorders, personality disorders and some psychological disorders (axis I).
The comorbidity was high. Consequently, to study the joint behaviour and find the adjusted ORs, in the end we applied a binary logistic regression («Enter» method), considering predictive variables only those that were significant in our first analysis. To do so, we used the statistical package SPSS20.
ResultsA third of the sample was found in a situation of risk based on the instrument chosen and the cut-off point of 6. The answers to items 13 and 15 respectively explore suicidal ideation and history of suicide attempts. Analysing these items, 34.2% of the inmates have thought about committing suicide at some time, while 22.5% of the inmates interviewed have attempted suicide at least once in their lives. As can be seen in Table 1, the data show that having some psychiatric disorder is an extreme risk factor of exceeding the cut-off of 6 and the inmate is thus likely to commit suicide. However, it should be noted that the wide confidence interval of this factor makes it impossible to have a rigorous interpretation or include this variable in the regression analysis. Looking at the groups of specific disorders, we can find that affective disorders (which include depressive and bipolar disorders, substance dependence disorders and personality disorders) are especially significant; all of these disorders present ORs above 4. Having suffered a psychotic disorder presents a crude OR of 3.146. Family psychiatric antecedents also function as a considerable risk factor. Both the existence of family penal antecedents and previous imprisonments double the risk of exceeding the cut-off point of 6. Other penal-related factors are not significant. It is interesting to point out that having a chronic organic illness presents an OR of 2, converting this into an important risk factor. The only protective factors found are being an immigrant and having a partner.
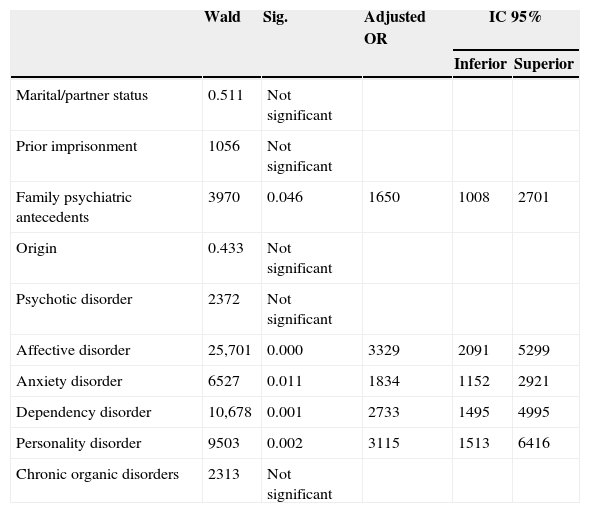
Table 2 displays the results of the logistic regression on introducing the significant predictive variables in the previous analysis. The only exceptions are the variable for axis I disorders, given that they are confused with the rest of the specific diagnoses, and the depressive disorder variable, because this diagnosis is included in the affective disorder variable.
Result of the logistic regression analysis (adjusted odds ratios [OR]).
| Wald | Sig. | Adjusted OR | IC 95% | ||
|---|---|---|---|---|---|
| Inferior | Superior | ||||
| Marital/partner status | 0.511 | Not significant | |||
| Prior imprisonment | 1056 | Not significant | |||
| Family psychiatric antecedents | 3970 | 0.046 | 1650 | 1008 | 2701 |
| Origin | 0.433 | Not significant | |||
| Psychotic disorder | 2372 | Not significant | |||
| Affective disorder | 25,701 | 0.000 | 3329 | 2091 | 5299 |
| Anxiety disorder | 6527 | 0.011 | 1834 | 1152 | 2921 |
| Dependency disorder | 10,678 | 0.001 | 2733 | 1495 | 4995 |
| Personality disorder | 9503 | 0.002 | 3115 | 1513 | 6416 |
| Chronic organic disorders | 2313 | Not significant | |||
It can be seen that all the sociodemographic or penal variables lose their significance when they are analysed together with the rest of the variables. Even the variable psychotic disorders stops being significant. The other psychopathological disorder variable still behave like risk factors, especially the variables affective disorder and personality disorder variables show adjusted OR values of more than 3 points. In the same way, having suffered a disorder from substance dependence doubles the risk of exceeding the cut-off of 6. Finally, the factor family psychiatric disorders resists regression analysis and maintains its significance with a small but significant adjusted OR. The ICs of the significant variables in the regression analysis are small. The percent of cases predicted correctly by the resulting equation was 75%, with 54% sensitivity and 86% specificity. Nagelkerke's R2, which indicates the goodness of adjustment of the system, yields a value of 0.343 (a considerable percent of explained variable). The lack of significance in the Hosmer–Lesmeshow test indicates, likewise, a good adjustment for the model.
DiscussionIn this section, we analyse the data from the first study on suicide risk in a prison population in Andalucía of these methodological characteristics. Firstly, we can say that both the percentage of suicidal ideation and of suicide attempts exceed by 7.5 and 15 times the prevalence in Spain for these found by the European Study on the Epidemiology of Mental Disorders.19 Specifically, in that report the prevalence of suicidal ideation and was 4.4% and 1.5%, respectively. In agreement with our results, a third of the sample is found in a situation of risk by having exceeded the cut-off criterion. Although we are analysing suicide risk and not mortality by suicide, our results are compatible with the existence of a mortality rate per suicide that multiplies by 8 that of the general population found by Bedoya et al.1 in Catalonian prisons in 2009. Our data greatly exceed the 3% of inmates that had attempted suicide the year prior to their imprisonment and the 2.7% for the last year in prison in Spain according to a study by the Directorate General of Prisons.20 In this study, the results were obtained by having the prison physicians fill in each inmate's data based on their clinical histories in 2006. Although we obtained the life prevalence of suicide attempts (which we feel is necessary to evaluate the risk appropriately), the difference from earlier results is considerable. In addition, we estimate that our study produces a methodological improvement, given that we interviewed and diagnosed the inmates personally.
Our crude ORs verify the importance of some legal and sociodemographic variables, such as the existence of a history of prior imprisonment and having sentimental relationships.11,12 However, other variables highlighted in other studies (for example, age or the existence of violent crimes) have not yielded significant results for us.6,13 With respect to this last factor, it should be pointed out that we have included among violent crimes not only homicides, assassinations and sexual assault, but also their attempts, robbery with force and injuries. Different categorizations, bearing in mind that there are also different legal systems among the countries, may be making the comparison of results more difficult.6 Just as with having a partner, being an immigrant functions as a factor of protection. Although we have not included immigrants with a deficient use of Spanish in our study, we cannot rule out the possible underestimation of suicide risk in the immigrant population due to language problems and to cultural differences. In addition, it is necessary to consider that, by excluding the immigrants that do not speak Spanish (precisely the ones that probably find themselves most isolated) from our samples, we are excluding the most vulnerable inmates that are perhaps in the greatest situation of risk. At any rate, other studies have found results similar to ours,10,21,22 even by a systematic review.14 Consequently, we have to go more deeply and search for alternative explanations for the possible methodological errors. In fact, related to this data, our team has attempted to explain results obtained in another study that shows that being an immigrant is also a protective factor against having some type of psychosis in the jails in Andalucía.23 Having some type of organic disorder (which doubles the risk) has to be considered as well, because this factor is normally not even included in study designs, although some studies have taken it into consideration.10 We should not let other, more specific variables in the prison setting make this factor invisible, given that having incapacitating somatic illness constitutes a clear risk factor in the general population.6,8
The regression analysis demonstrates the power that psychopathological variables have to explain suicide risk. The legal and sociodemographic variables do not stand up to a joint analysis. Only family psychiatric antecedents preserve significance. This does not mean that the crude ORs of the variables that disappear should be ignored; it indicates instead that there is some confusion among the set of variables and that the psychopathological variables are the strongest in explaining suicide risk. Among these variables, the life prevalence of some type of affective and personality disorders especially preserve a very high risk. Neither should dependence disorders (especially relevant in prison settings) and anxiety disorders be dismissed. The nucleus of the risk of suicide is found among these diagnoses. Having a diagnosis of psychotic disorder stops being a risk factor in the regression analysis. Over the last few years, experts have attempted to establish the psychopathological profile of patients diagnosed with schizophrenia at risk of committing suicide. Some authors suggest that the positive symptoms,10 especially in the acute phases, are clear factors of suicide risk; however, other authors have found the affective symptoms, desperation and depression are what best explain the risk of suicide in patients with schizophrenia.24,25 In this sense, the existence of elevated comorbidity among the diagnoses has probably caused the effect of this variable (psychotic disorders) to mix with psychopathological disorders, which are more powerful, mentioned earlier.
Our results are compatible with results from international studies that have analysed successful suicides; these studies emphasise the importance of psychiatric diagnoses as risk factors4,14,21,22,26 and offer ORs similar to ours. All of this should be considered with the requisite caution due to the methological difference between these (for example, in procedures to evaluate the diagnoses and the way to group them). It is precisely in this aspect that we believe lies one of the positive aspects of our study: a rigorous in situ clinical diagnosis of a wide sample of prison inmates in Andalucía. Without wanting to go into detail about results and analyses that are beyond the scope of our objective, our data yield a very high life prevalence for some axis I psychiatric disorders and personality disorders, 82% and 79% of the sample, respectively.
We now turn to the limitations of our study. Plutchik's suicide risk questionnaire is self-administered and, although the interviewers have had individual access to the inmates and have been able to go more deeply into and verify their answers, we cannot rule out that (for example) the prevalence of suicide attempts and thus the prevalence of risk have been overestimated by including what were no more than self-aggressions as suicide attempts. Without a doubt, a personal and systematic interview that explores the history of suicide attempts and suicidal ideation, as well as later follow-up of an inmate cohort, would improve our study. Some studies have debated the usefulness of the IPDE questionnaire in the prison population, recommending in any case a cut-off point of 4, as we do.27 In our study, we analyse the risk of committing suicide and not successful suicide, which prevents direct comparison with other studies.
In conclusion, the strength of the psychopathological variables and their prevalence in the prison poblation28 indicates the need for correct, detailed diagnosis in prisons to prevent suicides. The diagnoses and prior clinical information are undoubtedly useful, but they are insufficient. Likewise, it is essential for professional mental health teams to treat psychopathological disorders during imprisonments.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
FundingThe data analysed in this study stem from the project on prevalence of mental disorders in prisons in Andalucía (PRECA-II), which was funded by the Public Andalucía Foundation for the Social Integration of the Mentally Ill and was approved by the regional Ministry for Equality and Social Wellbeing of the governing council of Andalucía in agreement with the Ministry of the Interior of the Spanish government (BOE-A-2006, 10957).
Conflict of interestThe authors have no conflicts of interest to declare.
The authors of the study thank the interviewers in Sevilla and Granada for their work. We likewise thank the directors, technical team and civil servants at Morón and Albolote prisons for their collaboration and willingness to perform the research. Without all of them, this research would have been impossible. We also thank our colleagues at the Hospital San Juan de Dios in Barcelona who initiated the PRECA-I project for their collaboration and support in the early research periods.
Please cite this article as: Saavedra J, López M. Riesgo de suicidio de hombres internos con condena en centros penitenciarios. Rev Psiquiatr Salud Ment (Barc.). 2015;8:224–231.