The comorbidity of bipolar disorder and eating disorders has not been studied in depth. In addition, clinical implications involved in the appearance of both disorders are very important.
Material and methodsA systematic literature review of MEDLINE published up to September 2013 was performed, analyzing all the articles that studied the comorbidity of both conditions (bipolar disorder and eating disorders) and others’ research that studied the efficacy of pharmacological treatment and psychotherapy to improve these illnesses.
ResultsIn this review we found a high comorbidity of bipolar disorder and eating disorders, especially of bulimia nervosa and binge eating disorder. Studies show that lithium and topiramate are 2 of the more effective pharmacological agents in the treatment of both disorders.
ConclusionThere are a lot of studies that show evidence of comorbidity of bipolar disorder and eating disorders. However, further research is needed on assessment and treatment when these conditions co-exist, as well as study into the biopsychological aspects to determine the comorbid aetiology.
La comorbilidad entre el trastorno bipolar y los trastornos de la conducta alimentaria no está todavía bien estudiada. La aparición de ambos trastornos conlleva una serie de implicaciones clínicas muy importantes.
Material y métodosSe realizó una revisión sistemática de la literatura mediante una búsqueda bibliográfica en MEDLINE actualizada a septiembre de 2013 analizando todos los artículos que estudiaban la comorbilidad entre ambas condiciones (trastorno bipolar y trastornos de la conducta alimentaria), así como los trabajos que han estudiado la eficacia de tratamientos farmacológicos y de psicoterapia para mejorar ambos trastornos.
ResultadosEn esta revisión hemos encontrado una alta comorbilidad entre el trastorno bipolar y los trastornos de la conducta alimentaria, sobre todo la bulimia nerviosa y el trastorno por atracón. Los estudios muestran que el litio y el topiramato son algunos de los agentes farmacológicos con más efecto en el tratamiento de ambos trastornos.
ConclusiónA pesar de que hay una variedad de estudios, es necesaria más investigación tanto para el tratamiento cuando ambos trastornos coexisten como para la evaluación, además del estudio de la relación biopsicológica para determinar su etiología comórbida.
Before beginning to speak about comorbidity, it is important to know the disorders references in this review. On the one hand, we focus on eating disorders (EDs), which are divided into 3 types: anorexia nervosa (AN), defined as a rejection of maintaining a normal weight for the height and age (normally less than 85% of the expected weight) and intense fear of gaining weight; bulimia nervosa (BN), whose main symptom is the presence of binge eating episodes followed by compensatory behaviours to prevent weight gain; and lastly, binge eating disorder (BED), in which binge eating also occurs, but without compensatory behaviour, which usually leads to obesity. On the other hand, we talk about bipolar disorder (BD), which refers to a mood disorder in which the individuals alternate between periods of manic and depressive episodes, with euthymic states between episodes. The disorder is divided into type i (manic and mixed episodes) and type ii (episodes hypomanic and depressive episodes).1
Comorbidity refers to the presence of 2 or more unrelated medical problems in the same patient. Recognising the comorbidity between 2 disorders can help to explain the appearance of both in the same patient and provide professionals with information for assessment and decisions about interventions. This is the case with BD and EDs, whose comorbidity is increasingly studied for several reasons: (1) if EDs are more common in the bipolar population, assessing EDs in patients with BD is needed, especially when proposing treatment; (2) treating a disorder can worsen the progression of the other; it is necessary to evaluate the effects that the intervention on one has on the other and whether there is an effective drug or psychological treatment for both, when they occur separately and when the co-exist; and (3) generally, when 2 disorders are comorbid, there can be other associated comorbidities for each one separately, which is increased by their occurring jointly; in the case of these 2 disorders, many studies2–6 show that high rates of anxiety, alcohol abuse and drug addiction disorders coexist with the BD and EDs separately.
The objectives of the systematic review were 2: firstly, showing the evidence available about comorbidity between EDs and BD and its clinical implications, and secondly, examining the efficacy of the drug and psychological treatments that have been used when both illnesses co-exist.
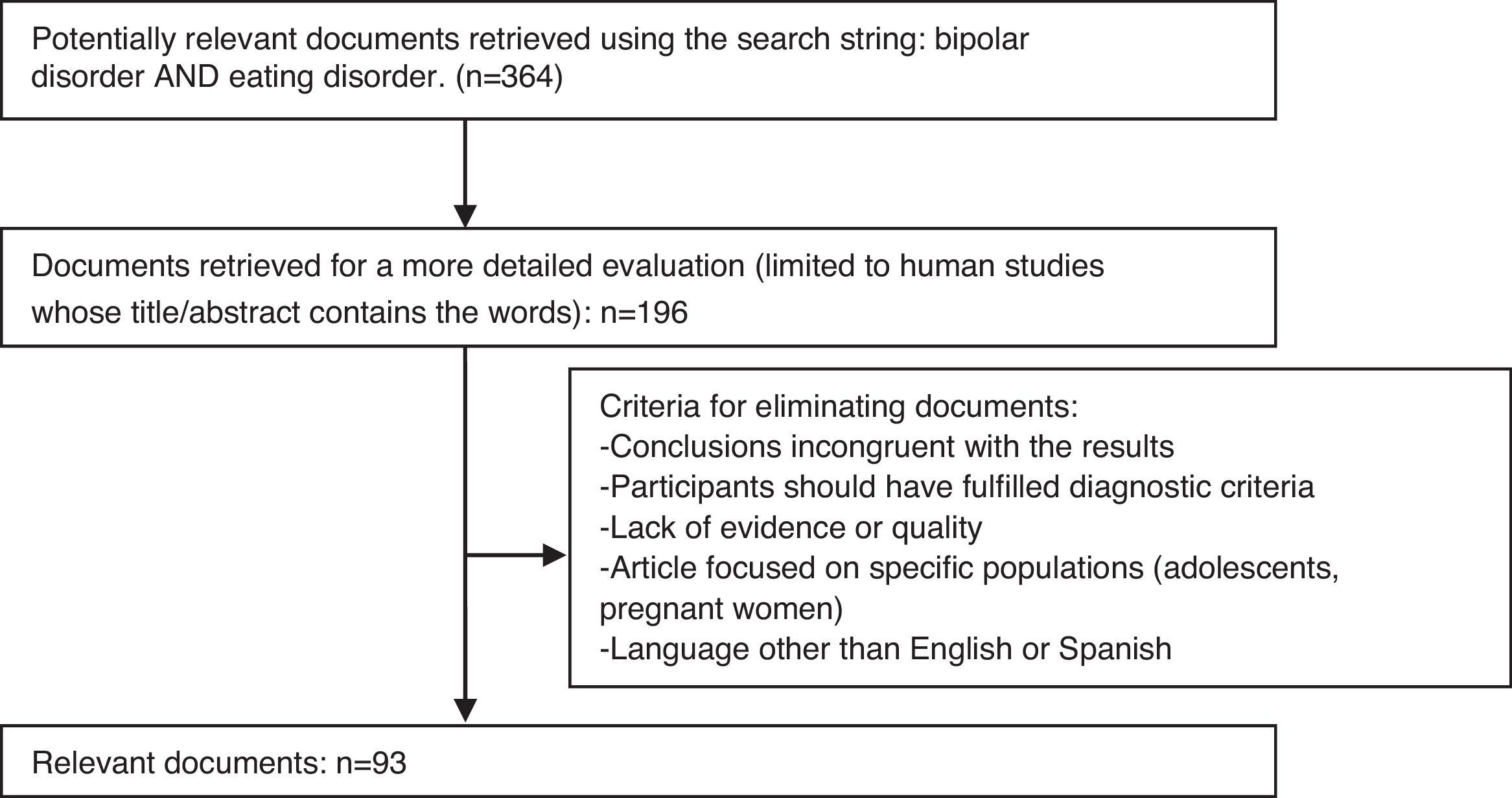
MethodWe have reviewed the articles published in MEDLINE/PubMed through September 2013, selecting the most recent ones (given that there is already a thorough one from 20054) to examine the comorbidity between the 2 disorders.
After we searched the main MEDLINE bibliography (Fig. 1) and analysed the documents, we performed a more detailed search based on the documents selected, using the words indicated below.
- 1.
To examine the evidence of usefulness of the treatments used in both disorders: bipolar disorder treatment, eating disorder treatment, olanzapine, antipsychotic, lamotrigine, antidepressive, lithium, sibutramine, topiramate, zonisamide, atomoxetine AND eating disorder.
- 2.
To analyse comorbidity with other EDs: obesity AND bipolar disorder, binge eating disorder; binge eating disorder; eating disorder («review»); bipolar disorder («review»); Bipolar Eating Disorder Scale.
The criteria for inclusion of the articles were as follows: the study was written in English or Castilian Spanish, it fulfilled diagnostic criteria for the 2 disorders studied (ED and BD), it was adequately powered, and it described the study sample adequately. The criteria for exclusion were: the sample included patients with other illnesses, the study was underpowered, the study conclusions were incongruent with study results, the study included only specific populations (such as adolescents or pregnant females), and the study objectives were incorrectly defined at the beginning.
Comorbidity of eating disorders and bipolar disorderThe comorbid presence of axis idisorders in patients with BD is generally high. McElroy et al.3 found high comorbidity between BD and axis I disorders in their study patients, with substance abuse and anxiety being the most common disorders,3,6 followed by EDs (6% over the lifespan and 1% currently).3 Comorbidity between BD and type i disorders was associated with greater severity.7
Based on McElroy et al.’s work,4 when a detailed in-depth examination is performed and the subthreshold disorders (conditions in the «spectrum» of the disorder) of both groups (BD and ED) are taken into consideration, a series of analogies arise insofar as phenomenology, course, family history, biology and treatment response.
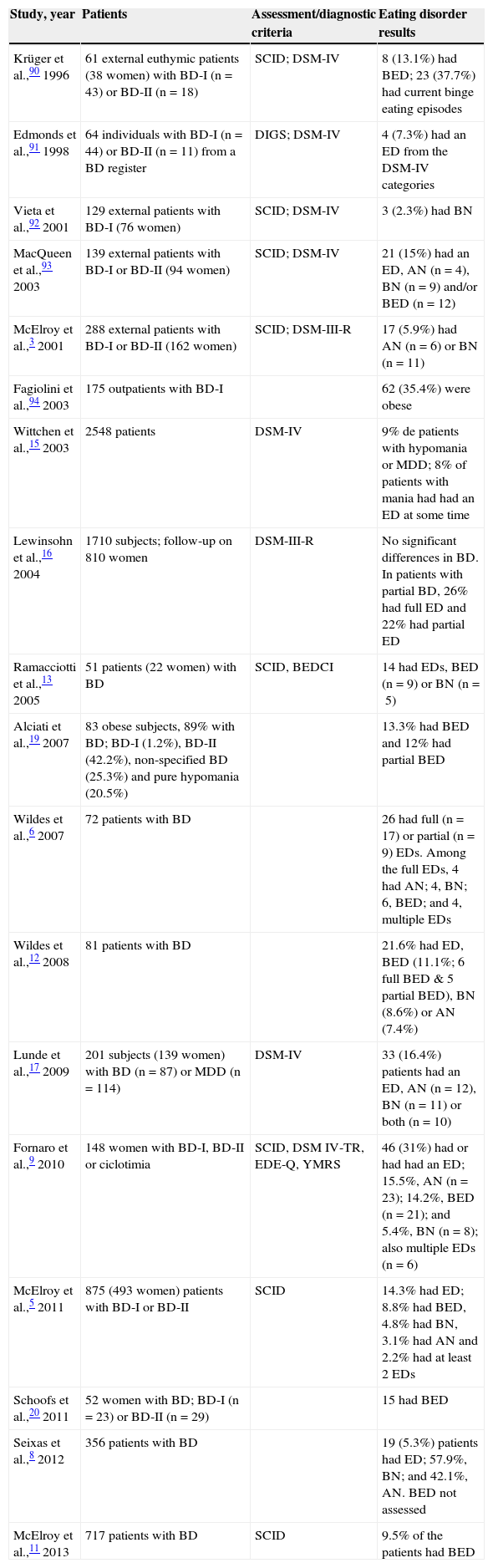
Eating disorders in bipolar disorderThe prevalence rate of EDs in BD vary substantially according to the studies in recent years, from 5.3%8 to 31%.9 One study found a rate of 1% current ED in BP3 (see Table 1 for a summary).
Studies on eating disorders in patients with bipolar disorder.
| Study, year | Patients | Assessment/diagnostic criteria | Eating disorder results |
|---|---|---|---|
| Krüger et al.,90 1996 | 61 external euthymic patients (38 women) with BD-I (n=43) or BD-II (n=18) | SCID; DSM-IV | 8 (13.1%) had BED; 23 (37.7%) had current binge eating episodes |
| Edmonds et al.,91 1998 | 64 individuals with BD-I (n=44) or BD-II (n=11) from a BD register | DIGS; DSM-IV | 4 (7.3%) had an ED from the DSM-IV categories |
| Vieta et al.,92 2001 | 129 external patients with BD-I (76 women) | SCID; DSM-IV | 3 (2.3%) had BN |
| MacQueen et al.,93 2003 | 139 external patients with BD-I or BD-II (94 women) | SCID; DSM-IV | 21 (15%) had an ED, AN (n=4), BN (n=9) and/or BED (n=12) |
| McElroy et al.,3 2001 | 288 external patients with BD-I or BD-II (162 women) | SCID; DSM-III-R | 17 (5.9%) had AN (n=6) or BN (n=11) |
| Fagiolini et al.,94 2003 | 175 outpatients with BD-I | 62 (35.4%) were obese | |
| Wittchen et al.,15 2003 | 2548 patients | DSM-IV | 9% de patients with hypomania or MDD; 8% of patients with mania had had an ED at some time |
| Lewinsohn et al.,16 2004 | 1710 subjects; follow-up on 810 women | DSM-III-R | No significant differences in BD. In patients with partial BD, 26% had full ED and 22% had partial ED |
| Ramacciotti et al.,13 2005 | 51 patients (22 women) with BD | SCID, BEDCI | 14 had EDs, BED (n=9) or BN (n=5) |
| Alciati et al.,19 2007 | 83 obese subjects, 89% with BD; BD-I (1.2%), BD-II (42.2%), non-specified BD (25.3%) and pure hypomania (20.5%) | 13.3% had BED and 12% had partial BED | |
| Wildes et al.,6 2007 | 72 patients with BD | 26 had full (n=17) or partial (n=9) EDs. Among the full EDs, 4 had AN; 4, BN; 6, BED; and 4, multiple EDs | |
| Wildes et al.,12 2008 | 81 patients with BD | 21.6% had ED, BED (11.1%; 6 full BED & 5 partial BED), BN (8.6%) or AN (7.4%) | |
| Lunde et al.,17 2009 | 201 subjects (139 women) with BD (n=87) or MDD (n=114) | DSM-IV | 33 (16.4%) patients had an ED, AN (n=12), BN (n=11) or both (n=10) |
| Fornaro et al.,9 2010 | 148 women with BD-I, BD-II or ciclotimia | SCID, DSM IV-TR, EDE-Q, YMRS | 46 (31%) had or had had an ED; 15.5%, AN (n=23); 14.2%, BED (n=21); and 5.4%, BN (n=8); also multiple EDs (n=6) |
| McElroy et al.,5 2011 | 875 (493 women) patients with BD-I or BD-II | SCID | 14.3% had ED; 8.8% had BED, 4.8% had BN, 3.1% had AN and 2.2% had at least 2 EDs |
| Schoofs et al.,20 2011 | 52 women with BD; BD-I (n=23) or BD-II (n=29) | 15 had BED | |
| Seixas et al.,8 2012 | 356 patients with BD | 19 (5.3%) patients had ED; 57.9%, BN; and 42.1%, AN. BED not assessed | |
| McElroy et al.,11 2013 | 717 patients with BD | SCID | 9.5% of the patients had BED |
AN: anorexia nervosa; BD: bipolar disorder; BED: binge eating disorder; BEDCI: Binge Eating Disorder Clinical Interview; BN: bulimia nervosa; DIGS: Diagnostic Interview Scale; DSM: Diagnostic and Statistical Manual of Mental Disorders; EDE-Q: Eating Disorder Examination Questionnaire; MDD: major depressive disorder; SCID: Diagnostic Clinical Interview for DSM Disorders; YMRS: Young Mania Rating Scale.
The BED cases were, in the studies reviewed, the most common EDs in the bipolar population; for that reason, specific studies on this comorbidity have been carried out.10,11 In one study, McElroy found that 9.5% of the patients with BD had BED.11 The second most common eating disorder in BD is BN, while the least common is AN, whose prevalence is uncertain.5,8,12 As for order of appearance, a study revealed that BD usually occurs before the ED in 55.7% of the cases, the ED appears before in 34.3%, and that joint appearance occurs in 10% of the patients.5 However, another study indicated that there are a greater number of patients that present onset at the same time than those that presented ED first.13
One of the few studies that analyse studies with samples composed of minors is that of McElroy et al.14 In one of the studies, it was indicated that 9% of the subjects with hypomania or major depressive disorder and 8% of the individuals with mania had had an ED at some time during their lives. The possibility or risk of having an ED was significantly greater in the individuals with hypomania or major depressive disorder than in the general sample, but not in the individuals with mania.15 Another study revealed that there were no significant differences between the 3 groups of ED in BD rates; however, when subthreshold BD was included, significantly elevated comorbidity rates appeared in the groups of full (26%) and partial (22%) syndromes compared with the non-ED group (4%).16
It seems that the likelihood that a patient with BD will have an ED is associated with:
- 1
BD severity: earlier BD onset (especially in AN),9 more mood episodes (predominantly depression2,5,6,17) and more symptomatic (especially with BED).3,5,9
- 2
Increased possibility of suicide: suicidal behaviour is common to both disorders and there is an association between ED presence and BP severity.2 The risk of suicide is consequently higher.2,5 Mood disorders are the alterations with the greatest number of suicidal behaviours, both in the general population (35.8%) and the hospitalised psychiatric population (20.8%).18
- 3
Negative correlation with the number of male participants and with the participants that have partners.8
- 4
Rise in the number of comorbidities (especially with BED), above all with substance abuse and anxiety disorders.2,5
- 5
Hyperactivity among the symptoms of hypomania19 in patients with bipolar spectrum disorder and morbid obesity.
- 6
The risk of being bipolar is increased when comorbid BN is diagnosed and rises when the broadest definitions of bipolarity are used.17
Patients with BD can present binges or loss of control over food at some time in their lives; in addition, they can carry out compensatory behaviours.12 Several studies have shown that the menstrual cycle affects binge eating frequency and intensity before and during menstruation and that these changes occur in patients with BD, with BED or both.
All the female participants with BED and BD (18/52) in a study20 indicated that bingeing episodes increased in frequency and severity the week before and during menstruation. Most of the female participants that did not have any EDs saw a greater increase of this impulse only during depressive episodes. A smaller number of subjects observed this increase only in manic episodes, while a few females reported this impulse in the euthymic stage only.
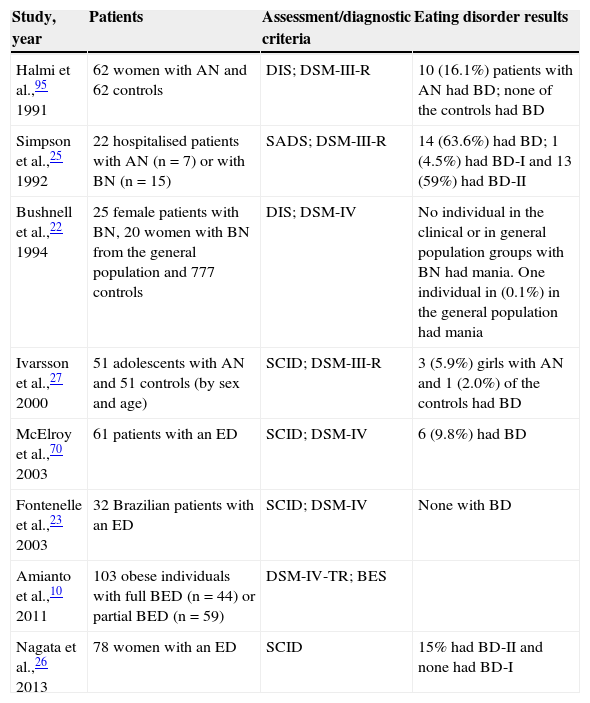
Bipolar disorder in eating disordersMcElroy et al.,4 after reviewing various studies, observed that BD ranged from the lack of EDs21–24 up to 63.6%25 (see Table 2 for a summary). The number of studies that specifically evaluate BD in the population that presents ED is much smaller in the last few years than the number of studies that evaluate the opposite.
Studies on bipolar disorders in patients with eating disorders.
| Study, year | Patients | Assessment/diagnostic criteria | Eating disorder results |
|---|---|---|---|
| Halmi et al.,95 1991 | 62 women with AN and 62 controls | DIS; DSM-III-R | 10 (16.1%) patients with AN had BD; none of the controls had BD |
| Simpson et al.,25 1992 | 22 hospitalised patients with AN (n=7) or with BN (n=15) | SADS; DSM-III-R | 14 (63.6%) had BD; 1 (4.5%) had BD-I and 13 (59%) had BD-II |
| Bushnell et al.,22 1994 | 25 female patients with BN, 20 women with BN from the general population and 777 controls | DIS; DSM-IV | No individual in the clinical or in general population groups with BN had mania. One individual in (0.1%) in the general population had mania |
| Ivarsson et al.,27 2000 | 51 adolescents with AN and 51 controls (by sex and age) | SCID; DSM-III-R | 3 (5.9%) girls with AN and 1 (2.0%) of the controls had BD |
| McElroy et al.,70 2003 | 61 patients with an ED | SCID; DSM-IV | 6 (9.8%) had BD |
| Fontenelle et al.,23 2003 | 32 Brazilian patients with an ED | SCID; DSM-IV | None with BD |
| Amianto et al.,10 2011 | 103 obese individuals with full BED (n=44) or partial BED (n=59) | DSM-IV-TR; BES | |
| Nagata et al.,26 2013 | 78 women with an ED | SCID | 15% had BD-II and none had BD-I |
AN: anorexia nervosa; BD: bipolar disorder; BED: binge eating disorder; BES: Binge Eating Scale; BN: bulimia nervosa; DIS: Diagnostic Interview Schedule; DSM: Diagnostic and Statistical Manual of Mental Disorders; SADS: Schedule for Affective Disorders and Schizophrenia; SCID: Structured Diagnostic Clinical Interview for DSM Disorders.
To establish the prevalence of hypomania in individuals with BED and subthreshold BED, an assessment was performed using the Hypomania Checklist-32, controlling personality features as variables of potential confusion. The subjects with BED had lower scores in self-direction and cooperativeness, and higher scores on the Hypomania Checklist-32 than the individuals with subthreshold BED. A significant association was also observed between BED diagnosis and female sex, cooperativeness and the Hypomania Checklist-32. The patients with BED had higher scores in hypomania, regardless of the personality features.10
In another study, with a sample of 78 women with EDs, 15% of the sample was found to have BD-II (hypomania) and no subject presented BD type I.26
Prevalence in studies with populations from different countries varied greatly. In a Swedish study,27 57% of the patients with AN had a depressive disorder, while only 3 out of 51 patients had BD. In another study, carried out in Japan,28 in which BED was not assessed, a small number of patients had had BD-II (3%) or hypomanic disorder (1%) over the course of their lives. The rates were even lower in the Brazilian population,23 in which no patient with BED was found to have BD, but BD was indeed found in obese individuals without BED (3%).
In a less rigorous study,29 a 15-year-old girl with AN presented an manic episode after a month of antidepressant treatment. The patient had shown irritability in food contexts, paranoid ideation and brief periods of euphoria and feelings of grandiosity with other periods of isolation, sadness and despondency in the 2 years before. Even after regaining weight and using 3 mood stabilisers, the patient continues presenting emotional instability. It is possible that the early non-affective symptoms (low self-esteem, loss of social contact, irritability, mood swings and insomnia) represent a precursor of the affective disorder.
Discussion (clinical implications and pharmacological approach)Assessment of comorbidity between eating and bipolar disordersDue to the amount of studies that reveal a strong comorbidity between EDs and BD, a scale called the Barcelona Bipolar Eating Disorder Scale (BEDS) was created to establish the intensity and frequency of food alterations in the bipolar population. It consists of a 10-item scale, whose mean completion time is 1min and 21s. This scale was administered to a healthy control group to assess its feasibility and to establish the cut-off point (which was pre-established at 13).30 The BEDS has shown appropriate psychometric properties for assessing food alterations in patients with BD in clinical practice and in research.30,31 As demonstrated in a 2008 study,31 the scale showed sufficient feasibility, discriminative validity (of the patients with respect to the controls) and sensitivity.
The only study found that assessed its patients with the Barcelona BEDS observed that the mean scale scores were significantly higher in patients with BD than in the controls. Surprisingly, 65.9% of the patients with BD had ED, with BED being the most prevalent.32
Therapeutic approach to comorbidityAs has been revealed, BD and the EDs are strongly comorbid. Consequently, when choosing a treatment for one of the disorders, you have to consider that the other may co-exist, and any intervention has to focus on both of them. Besides, the treatment for one may have a negative effect on the symptoms of the other, such as lithium, which has shown an association with weight gain in patients with BD.7 That is why the obesity of patients with BD may be caused by either the treatment or by a comorbid ED.
Next, we summarise the main drug groups (analysing the most important active ingredients) that have been used in approaching the treatment for both disorders.
Mood stabilisersLithiumLithium is considered an effective long-term mood stabiliser, especially for mania. Various reviews14,33,34 have found that it is also an effective agent for the treatment or improvement of patients with AN and/or BN, but there do not seem to be any studies demonstrating the efficacy of monotherapy lithium use for BED, perhaps because weight gain (a characteristic associated with this ED) is one of the side effects of lithium.7
In a placebo-controlled study, 16 individuals with AN35 were divided into 2 groups: with lithium or with placebo. The patients treated with lithium had a greater weight gain following 3 and 4 weeks of treatment, in addition to improved insight.
Less rigorous evidence taken from clinical cases36–38 indicate that lithium-treated patients with AN show positive results in improving symptoms of the disorder and in weight gain (with a variability of 9–15 in weight increase), some together with treatment with another drug, such as carbamazepine.37 In addition, the results are maintained in the medium term.
As far as the efficacy of lithium for BN, there are contrasting conclusions. In a placebo-controlled study,39 the results were similar for the lithium and placebo groups with respect to reducing binges. In another study,40 there were better results in the group treated with lithium than in the placebo group, but the individuals in the lithium group experienced weight gains.
Lithium moderately or notably improved the bulimic episodes in 12 of 14 women in an open clinical trial.41 In another trial by the same author, 11 of 17 patients reduced the bulimic episodes by 75% or more, combining the drug treatment with cognitive-behavioural therapy.42
Lithium has also been used to potentiate the effects of other drugs, such as topiramate (an anticonvulsant agent), for BED. In 1 study,43 lithium was added to the medication of the patients taking topiramate. Most patients showed improvements in affective symptoms, as well as a reduction of the BED symptoms, weight and binge frequency after the addition of lithium.
Although lithium has shown itself to be effective in treating BD as well as for AN and BN, above all, the professionals have to consider the side effects that may appear in the patients. Vestergaard et al.44 evaluated 237 patients treated with lithium as to side effects. One fourth of the patients had 3 or more complaints, among which hand tremors, excessive thirst, a weight gain of more than 10kg, diarrhoea and oedemas in the legs and face stood out.
OthersIn several reviews,14,33,45,46 drugs such as olanzapine or risperidone, valproate, carbamazepine, atypical antipsychotics and quetiapine also demonstrated positive results in the treatment of EDs; these drugs are also used, upon occasion, for BD. Valproate showed efficacy in reducing affective and bulimic symptoms in a patient with BD and BN;47 however, it generally seems to increase compulsive eating behaviour in patients with BED and comorbid BD,48 in BN33 and in BD.49
As for AN, atypical antipsychotics, olanzapine, quetiapine and risperidone seem to be generally safe. They are also effective in treating depression, anxiety and the symptoms of AN (reducing the fear of gaining weight, difficulties in eating and the distortion of the body image and insight).45,50–58 However, these drugs do not help to gain weight,46 one of the most important objectives in AN treatment.
AnticonvulsantsAnticonvulsants began to be studied as agents for ED treatment, especially in BED and BN, because of their weight-reducing effect in individuals with epilepsy. In fact, they are currently one of the most studied agents for treating EDs that include binge eating (above all BED)4,33,45,59–63 when these EDs make their appearance without the co-existence of other disorders or with comorbid BD; these agents are also effective in treating this.
The efficacy of topiramate and zonisamide has been studied for treating BN and BED.62,64 Various studies, randomised with placebo group, have been published on treatment with topiramate in patients with BN.65,66 The results showed that the topiramate group improved in areas such as excessive and uncontrollable food intake, discontent with the body, obsession for extreme thinness, and worry about food and diet.65 In addition, among other factors, there was a reduction in binge eating, in purging and in body weight with this drug.67,68
The studies with topiramate also focused on BED. In a study carried out with obese patients with BED,68 the group taking topiramate demonstrated a greater reduction of the binges than the placebo group. Topiramate efficacy in treating individuals with BED and obesity has been shown by various studies.69–72 Other studies, in which non-obese patients with BED were assessed,48 demonstrated topiramate efficacy in reducing weight and binge frequency. The most common side effects were nausea, paresthesia, upper respiratory tract infection, somnolence and headache. However, the side effects are not generally more frequent than with the use of the placebo.
Many studies have indicated that the combination of lithium with topiramate is very beneficial. Kotwal et al.43 selected 12 obese individuals with comorbid BED and BD for their study. These patients, who were being treated with topiramate for BED, received lithium as well when they presented mood instability. This addition was associated with an improvement in the mood symptoms. There were also numerical differences, although they were not statistically significant, in reduction of the binges and in weight loss, comparing pre- and post-addition of lithium.
Although topiramate is one of the most frequently-studied anticonvulsant drugs for ED treatment, zonisamide may also play an important role. McElroy et al.,73 with a sample of 60 outpatient patients with BED and obesity, gave 30 of the 60 zonisamide, while the rest received a placebo. Compared to the placebo, zonisamide was associated with a significantly larger rate in reducing binge frequency, body weight and body mass index (BMI).
Idini et al.74 reported a study carried out with 17 women having BED or BN, 10 of which continued treatment with zonisamide during the 12 months of follow-up (no prior medication was suspended). BMI was reduced by 5.72%, and there was a decrease in binges and in episodes of self-harm.
Other anticonvulsants such as carbamazepine and lamotrigine have shown good tolerance and treatment efficacy.34,75
AntidepressantsAntidepressants are generally used together with mood stabilisers in the treatment of bipolar depression, despite the fact that they can increase manic/hypomanic episodes. They have also shown efficacy in ED treatment, especially for BN and BED, given that they seem to reduce bingeing.14,34,45,59–61,76,77 Their efficacy in AN is very low, but they were used to treat this disorder in various studies, which did indeed obtain positive results, for the shortage of drug treatment.34,46,77
Desipramine,78 fluvoxamine79 and fluoxetine80 demonstrated their effectiveness for treating BN and BED and for preventing relapses. In a study,37 9 patients with AN were treated with antidepressants. Seven patients showed a significant improvement in weight and in other symptoms of AN and BN; the other 2 individuals showed moderate or great improvement in bulimic symptoms, but they did not gain weight.
Other drugsSome reviews indicated that atomoxetine,61,81 used in treating attention-deficit hyperactivity disorder (ADHD), can be effective in BED treatment. These studies showed that atomoxetine was associated, compared with the placebo, with a greater reduction of binges, body weight and BMI. In a single-case study with methylphenidate82 (also used for ADHD), complete medium-term remission of BN symptoms was achieved.
In several studies using sibutramine to treat obesity in individuals with BED, improvements in various variables were found in most of the patients. There was BED remission in the majority of the cases; in addition, most subjects experienced reduced their weight, BMI and binge eating.83–86
Psychological treatment- –
Cognitive-behavioural therapy: effective in patients with BED. It focuses on, among other things, reducing and controlling the binges, improving body image, emphasising and teaching structured patterns of food intake, and cognitive restructuring as to weight, shape, body image and food in general.87,88
- –
Group-format interpersonal therapy: supposes that the negative effects associated with interpersonal problems lead to the binges.87
- –
Behaviour therapy: uses traditional behaviour strategies aimed at modifying food intake and physical exercise habits to promote weight loss. Techniques: stimulus control and alternative behaviours instead of binge eating.87
Cognitive-behavioural and interpersonal therapies seem to give positive results in BD as well; however, psychoeducation is strongly recommended.89
As is the case in all reviews, it should be emphasised that a limitation in this study was that, in spite of the large number of studies found and that from those we chose only the ones that fulfilled specific quality criteria, the samples of patients studied were sometimes linked to hospital units or specific outpatient clinical centres with special patient samples. Consequently, it may not be possible to extrapolate our conclusions to the patients treated in normal clinical practice. Likewise, more and better randomised clinical trials in this specific patient population (that have comorbid BD and ED) are needed to assess the efficacy of the psychotropic drugs and the psychological treatments used with them.
ConclusionsA strong correlation was observed between EDs and BD, which was associated with greater BD severity and an under-recognition of EDS in medicated patients with BD, because one of the side effects of some drugs is increased food intake.13 In addition, the presence of depressive episodes was seen to be related to an overall deterioration.
Drug therapy is highly effective for the treatment of EDs and BD, both when these conditions are comorbid and when they occur independently. However, it is important to add that comorbidity has to be considered, given that the pharmacological treatment effective for one of the disorders may worsen the symptoms of the other.44
Optimum treatment should benefit both disorders, stabilising any affective alteration without lessening the effect on EDs. Further research is needed as to the possible side effects of drug treatment for one disorder on the other condition, and to ascertain in-depth knowledge as to which mechanisms, both psychological and biological, can determine this comorbidity.
Conflict of interestDr. L. Gutiérrez-Rojas declares that he has given conferences or received funding to attend congresses from Janssen, Astra Zeneca, Rovi, Lundbeck, Otsuka, GSK and Pfizer. E. Alvarez Ruiz has no conflicts of interest to declare.
Please cite this article as: Álvarez Ruiz EM, Gutiérrez-Rojas L. Comorbilidad entre el trastorno bipolar y los trastornos de la conducta alimentaria. Rev Psiquiatr Salud Ment (Barc.). 2015;8:232–241.